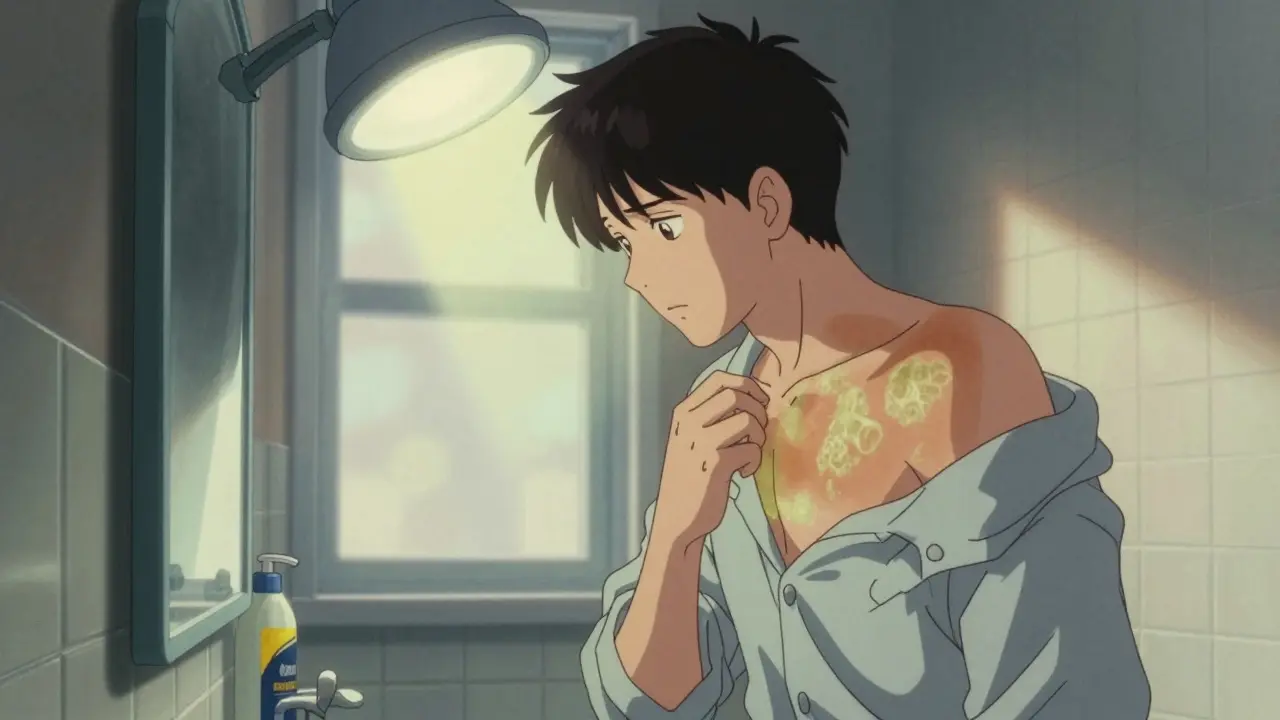
Ever looked in the mirror and seen patches of skin that just don’t tan like the rest? If you’ve got white, pink, or brown spots on your chest, back, or shoulders that won’t go away-even after sun exposure-you’re not alone. This isn’t a rash from allergies, not eczema, and definitely not poor hygiene. It’s tinea versicolor, a common but often misunderstood fungal skin condition caused by an overgrowth of yeast that lives naturally on your skin.
What Exactly Is Tinea Versicolor?
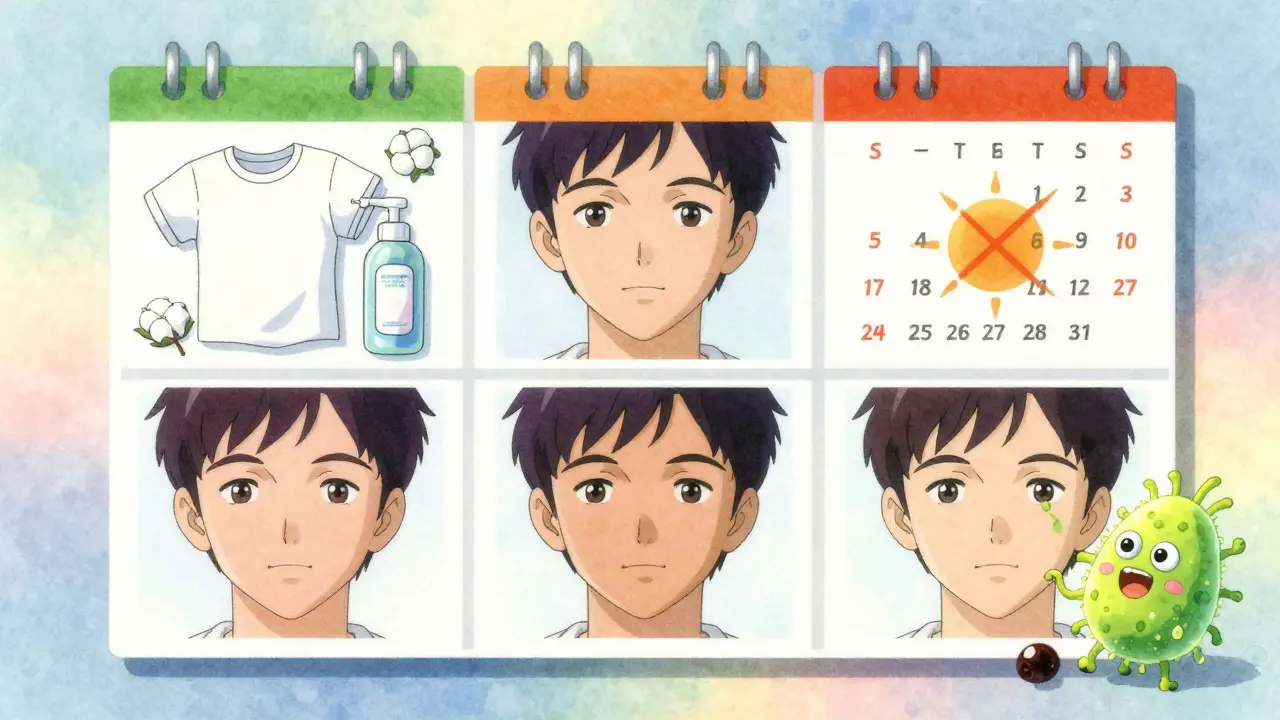
Tinea versicolor, also called pityriasis versicolor, happens when a type of yeast called Malassezia-which normally hangs out harmlessly on your skin-starts multiplying too fast. This isn’t an infection you catch from someone else. You already have this yeast on you. It’s your body’s own microbiome going rogue. The yeast doesn’t cause pain or itching in most cases. But it does mess with your skin’s pigmentation. In lighter skin tones, it often leaves pale or pink patches. In darker skin tones, it can look darker or lighter than surrounding skin. The reason? The yeast produces azelaic acid, which blocks melanin production in the skin. That’s why those patches stay lighter even when the rest of your skin tans in the sun. It’s most common in teens and young adults, especially between ages 15 and 30. That’s because oily skin and higher sweat levels create the perfect environment for the yeast to thrive. The condition shows up mostly on the chest, back, shoulders, and upper arms. It rarely affects the face-unless you’re a child.Why Does It Keep Coming Back?
Here’s the frustrating part: even after treatment, tinea versicolor comes back in 60 to 80% of people within the first year. That’s not because you didn’t do enough. It’s because the yeast never truly leaves your skin. It’s always there, waiting for the right conditions. Heat and humidity are the biggest triggers. In tropical climates, up to 50% of people experience it. Even in places like Melbourne, where summers get warm and sticky, recurrence rates jump during October to March. Sweating a lot, wearing tight synthetic clothes, using oily lotions, or having hormonal changes (like during pregnancy or puberty) can all set the stage for a flare-up. Some people are more prone to it due to genetics. Studies suggest about 30% of susceptibility comes down to how your immune system responds to the yeast. But it’s not about being dirty. In fact, scrubbing your skin too hard can make it worse by stripping away natural oils and irritating the barrier that keeps yeast in check.How Is It Diagnosed?
Doctors don’t usually need a fancy test. A quick look at the patches, especially if they’re scaly and don’t tan, is often enough. But to be sure, they might do a KOH test. A small scraping of skin is mixed with potassium hydroxide and looked at under a microscope. If you’ve got tinea versicolor, you’ll see the classic "spaghetti and meatballs" pattern-long strands of fungus with round yeast cells clinging to them. This test is 95% accurate. Some clinics use a Wood’s lamp, which makes the affected skin glow a yellowish-green under ultraviolet light. It’s not foolproof, but it helps confirm when the diagnosis isn’t clear.
Treatment: What Actually Works
You have two main options: topical treatments and oral meds. Topical treatments are the first line. The most effective and widely available is selenium sulfide 2.5% shampoo (like Selsun Blue). You apply it to the affected areas, leave it on for 10 minutes, then rinse. Do this daily for two weeks. Studies show it clears the infection in about 78% of cases. Ketoconazole 2% shampoo works similarly and is often used for maintenance after the initial treatment. Another option is antifungal creams like clotrimazole or miconazole. These are fine for small patches but less effective for widespread cases. Oral treatment is for stubborn or widespread cases. Fluconazole, taken as a single 300mg pill once a week for two to four weeks, clears the yeast in over 90% of people. But it requires a prescription and needs liver function monitoring, especially if you’re on other meds or have existing liver issues. Important note: Even after the yeast is gone, the discoloration stays. Your skin doesn’t regain its normal color overnight. It can take months-sometimes up to a year-for pigmentation to even out. That’s normal. Don’t mistake lingering patches for treatment failure.Prevention: The Real Game-Changer
Most people stop treatment once the patches fade. That’s the #1 mistake. To keep tinea versicolor away, you need a maintenance routine. The gold standard? Use ketoconazole 2% shampoo once a month during warm months. Apply it like you’re washing your hair-lather it on your chest, back, and shoulders. Leave it on for 5-10 minutes. Rinse. Do this every month from spring through fall. A UCLA Health study tracked 200 patients who did this. After one year, only 25% had a recurrence. Those who skipped maintenance? Nearly 80% came back with patches. Other proven prevention tips:- Avoid oil-based lotions, sunscreen, or moisturizers. They feed the yeast. Opt for water-based or "non-comedogenic" products.
- Wear loose, breathable, moisture-wicking fabrics. Cotton and bamboo are better than polyester or nylon.
- Shower right after sweating. Don’t sit in damp clothes. Change out of gym gear immediately.
- Use gentle, non-soap cleansers. Soap can dry out your skin and disrupt its natural pH, making it easier for yeast to take over.
- Don’t over-cleanse. Scrubbing hard or using antibacterial soaps daily can damage your skin barrier and backfire.
What Doesn’t Work (And Why)
There’s a lot of misinformation online. Here’s what to ignore:- Tea tree oil, apple cider vinegar, or coconut oil-no solid evidence they kill Malassezia yeast. Coconut oil? It’s fatty. That’s like pouring fuel on the fire.
- Sunbathing-it makes the patches look worse. Unaffected skin tans; the yeast-affected areas don’t. That contrast makes them stand out more.
- Antibiotics-they don’t touch fungi. They might even make it worse by killing off good bacteria that help keep yeast in check.
- Going to a spa or sauna regularly-heat and sweat are triggers. If you’re prone to this, limit steam rooms and hot yoga during peak months.
When to See a Dermatologist
You don’t need to rush to a doctor for every patch. But see one if:- The patches spread quickly or don’t improve after two weeks of OTC treatment.
- You have recurring episodes (two or more times a year).
- You’re on long-term steroids, have diabetes, or a weakened immune system.
- The discoloration is causing anxiety, social avoidance, or depression.
Long-Term Outlook and New Research
The good news? Tinea versicolor is not dangerous. It doesn’t cause scarring or spread internally. It’s a nuisance, not a threat. New research is promising. Scientists at UC San Diego found that certain skin bacteria can suppress Malassezia yeast by up to 68% in lab settings. That could lead to probiotic creams or sprays in the next few years. There’s also concern about antifungal resistance. A small but growing number of yeast strains are showing reduced sensitivity to ketoconazole. That’s why doctors now recommend rotating treatments or using combination therapy for recurrent cases. Clinical trials are underway to test new topical combinations that could cut recurrence rates even further. The key takeaway? You can live with this. You don’t have to let it control your life. With the right treatment and a simple monthly routine, you can keep it under control for years-even permanently.It’s not about perfection. It’s about consistency. One shampoo a month. No oils. Dry off fast. That’s it.
Is tinea versicolor contagious?
No, tinea versicolor is not contagious. You can’t catch it from someone else, even through skin contact or shared towels. The yeast that causes it lives on everyone’s skin. It only becomes a problem when it overgrows due to heat, sweat, or oily skin.
Can tinea versicolor be cured permanently?
It can be cleared effectively, but not permanently eradicated because the yeast is part of your natural skin flora. However, with consistent monthly maintenance treatment-like using ketoconazole shampoo once a month-you can prevent recurrence for years. Most people who stick to this routine go years without a flare-up.
Why do the patches stay white even after treatment?
The yeast produces azelaic acid, which blocks melanin production in the skin. Even after the yeast is killed, the skin needs time to rebuild its pigment. This can take 6 to 12 months. Sun exposure during this time makes the contrast worse because unaffected skin tans while the treated areas don’t. Patience is key-this is normal.
Can I use Selsun Blue every day to prevent it?
No. Selsun Blue is meant for short-term treatment, not daily use. Using it every day can dry out your skin and irritate it. For prevention, switch to ketoconazole 2% shampoo once a month. It’s gentler and specifically proven for maintenance.
Does stress cause tinea versicolor?
Stress doesn’t directly cause it, but it can weaken your immune system enough to let the yeast overgrow. If you’re under chronic stress, sleep-deprived, or sick, you may be more likely to experience a flare-up. Managing stress helps, but it’s not a substitute for antifungal treatment.
Are there natural remedies that work?
There’s no reliable scientific evidence that natural remedies like tea tree oil, apple cider vinegar, or garlic cure tinea versicolor. Some may even make it worse-coconut oil, for example, is fatty and feeds the yeast. Stick to proven antifungal treatments backed by clinical studies.
Can children get tinea versicolor?
Yes, though it’s less common. Children can develop it, especially if they’re in hot, humid climates or have oily skin. The patches may appear on the face in kids, unlike adults. Treatment is the same, but use lower concentrations and consult a pediatric dermatologist before starting oral meds.
How long should I keep using preventive shampoo?
Use it monthly for at least 6 to 12 months after your last flare-up. If you’ve had two or more recurrences in a year, experts recommend continuing it year-round. Stopping too soon is the main reason it comes back.
Next Steps: Your Simple Prevention Plan
If you’ve had tinea versicolor before, here’s what to do right now:- Buy ketoconazole 2% shampoo (available over-the-counter in Australia and many countries).
- Set a monthly reminder on your phone-for example, the first Saturday of every month.
- Apply it to your chest, back, and shoulders during your shower. Leave it on for 5-10 minutes.
- Switch to non-oily skincare and moisturizers.
- Wear loose cotton clothes after sweating.
- Shower within 30 minutes after exercise or being in the heat.


Milla Masliy - 13 January 2026
I’ve had tinea versicolor for years and honestly, the ketoconazole shampoo trick changed my life. I use it once a month like clockwork-first Saturday of every month, no exceptions. Even in humid summers in Florida, I’ve stayed clear for over two years now. It’s not glamorous, but it works. No more avoiding swimsuits or feeling self-conscious at the gym.
Also, switching to non-oily sunscreen was a game-changer. I used to think coconut oil was ‘natural’ so it must be good… turns out it’s basically yeast buffet. Who knew?
Pankaj Singh - 15 January 2026
Stop wasting time with shampoo. If you’re still getting flare-ups after using ketoconazole, you’re doing it wrong. Either you’re not leaving it on long enough, or you’re still using coconut-based lotions and pretending you’re ‘natural.’ This isn’t yoga class-it’s a fungal overgrowth. Get serious. Use the damn shampoo. Shower after sweat. Stop touching your face. Done.
Also, stop Googling ‘tea tree oil cure.’ It’s not a miracle. It’s a myth. And you’re not special.
Scottie Baker - 15 January 2026
Okay but why does no one talk about how embarrassing this is?? I had it on my chest for months and I literally stopped going to the beach, stopped dating, even avoided yoga class. I thought I was just ‘fair-skinned’ until I saw the patches in the mirror after tanning.
Then I found out it’s just yeast? Like… my own body betrayed me? I cried. Then I used Selsun Blue for two weeks and it faded. But the shame? That took longer to heal.
Also, why is this not on every dermatology 101 syllabus? Everyone should know this.
Anny Kaettano - 16 January 2026
As someone who’s worked with patients with chronic dermatological conditions, I want to emphasize the neuro-immunological component here. Malassezia is a commensal organism, but in susceptible hosts, it triggers a Th2-skewed immune response, which suppresses melanocyte activity via azelaic acid upregulation.
That’s why repigmentation is delayed-it’s not just about killing the yeast, it’s about resetting the skin’s epigenetic signaling. Maintenance therapy isn’t optional-it’s immunomodulatory. Monthly ketoconazole acts as a microbial reset button, preventing dysbiosis from re-establishing.
Also, avoid occlusive fabrics. They create a microenvironment that favors fungal biofilm formation. Cotton isn’t just ‘breathable’-it’s a barrier modulator.
Angel Molano - 17 January 2026
Stop using shampoo on your skin. It’s not a cure. It’s a band-aid. You’re just masking the problem. Real solution? Clean diet. No sugar. No carbs. No oils. Fix your gut. Fix your skin. Simple.
Randall Little - 18 January 2026
So let me get this straight: you’re telling me that a yeast that lives on 90% of humans suddenly becomes a problem because… we sweat? And we use lotion? And we’re 15-30 years old? That’s not a disease. That’s biology with bad marketing.
Also, why is this called ‘tinea versicolor’? It’s not tinea. Tinea is dermatophytes. This is pityriasis. Why are we still using outdated taxonomy? And why does every article say ‘it’s not contagious’ like that’s some kind of reassurance? Of course it’s not contagious-you’ve had it since birth.
Also, ‘spaghetti and meatballs’? Really? Who approved that term? I’m not laughing. I’m crying.
jefferson fernandes - 19 January 2026
For real, though-monthly ketoconazole? YES. But also, don’t forget the shower timing. Shower within 30 minutes after sweating? That’s not a suggestion-that’s a biological imperative.
And if you’re using ‘natural’ products, you’re basically feeding the fungus. I’ve seen people put olive oil on their chest and then wonder why it came back. Bro. It’s not a salad. It’s skin.
Also, if you’re still using soap, stop. Use pH-balanced cleansers. Your skin’s microbiome isn’t a battlefield-it’s a garden. Treat it like one.
And yes, it’s okay to feel embarrassed. But you’re not broken. You’re just human.
And no, your dog can’t give it to you. Stop asking.
Acacia Hendrix - 19 January 2026
Frankly, I find it astonishing that this is even a topic of public discourse. The fact that individuals are treating a microbiome dysbiosis with over-the-counter antifungals-without any baseline microbiome profiling or genetic susceptibility screening-is frankly irresponsible. The entire paradigm is rooted in symptomatic palliation, not systems biology.
Until we map individual lipidome profiles and correlate them with Malassezia colonization density, we’re just performing folk medicine with shampoo bottles.
Also, ‘Selsun Blue’? Please. That’s a 1990s relic. The real innovation lies in topical probiotic formulations-like Lactobacillus reuteri lysates-which modulate sebum composition and inhibit yeast adhesion. But no, let’s keep using dandruff shampoo like it’s 2003.