Skipping a dose of your prescription medication might seem harmless-especially if you’re feeling fine, or if you’re just too busy. But that one missed pill can set off a chain reaction that puts your health at risk. It’s not about being perfect. It’s about keeping your body in the right balance, day after day. Your medicine isn’t just a backup plan. It’s doing critical work inside you right now, even when you don’t feel it.
Why Timing Matters More Than You Think
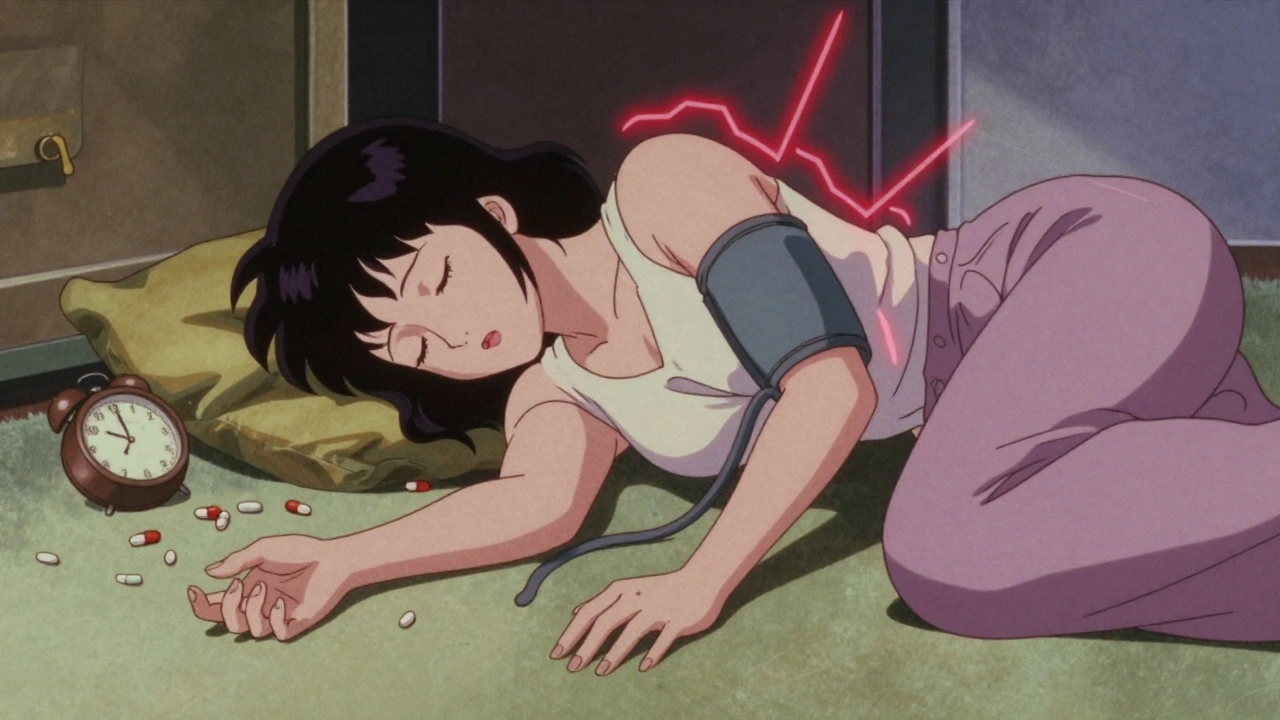
Your body doesn’t work on a schedule that matches your alarm clock or your lunch break. It works on chemistry. Every time you take a medication, your bloodstream absorbs it, and your body starts using it. But that drug doesn’t last forever. It gets broken down, flushed out, or used up. If you wait too long between doses, the level of medicine in your blood drops below what’s needed to do its job. Too much time passes, and the drug’s effect fades-sometimes dangerously. For example, if you’re on blood pressure medication, skipping even one dose can cause your pressure to spike. That spike doesn’t just make you feel off-it puts extra strain on your heart, arteries, and kidneys. Over time, those repeated spikes can lead to heart attack, stroke, or kidney failure. You might not notice the damage until it’s too late. High blood pressure doesn’t always come with symptoms. That’s why taking your pills on time isn’t optional. It’s protection. Antibiotics are another clear case. You finish your course because your doctor told you to. But why? Because when you stop early, the strongest bacteria survive. They multiply. Next time, the same infection won’t respond to the same drug. That’s how antibiotic resistance starts. The CDC says completing the full course is the single most important thing you can do to stop superbugs from spreading. One skipped dose could mean your next infection is harder-or impossible-to treat.Medicines That Can’t Wait
Some medications have zero room for error. Take warfarin, a blood thinner. It keeps clots from forming, but it’s a tightrope walk. Too little, and you risk a stroke or clot. Too much, and you could bleed internally. Your doctor checks your INR levels every few weeks to make sure you’re in the safe zone. But that balance depends on you taking the exact same dose at the same time every day. Miss a dose, or take it at 8 p.m. one night and 2 a.m. the next, and your INR swings unpredictably. That’s not a minor mistake. It’s a medical emergency waiting to happen. Same goes for transplant patients on immunosuppressants. Their bodies are trained not to attack the new organ. But if the drug level dips-even briefly-your immune system can wake up and start rejecting the transplant. That’s not hypothetical. It happens. And when it does, the organ can be lost. No second chances. For people with diabetes, timing is tied to meals. If you take your insulin or other glucose-lowering drug too early or too late, your blood sugar can crash. Hypoglycemia isn’t just dizziness or shakiness. It can lead to seizures, unconsciousness, or even death if not treated fast. That’s why doctors tell you to take certain meds with food or 30 minutes before eating. It’s not a suggestion. It’s physics and biology working together.Why People Skip Doses (And What to Do About It)
Let’s be real. Life gets in the way. You travel. You forget. You feel better and think you don’t need it anymore. You’re scared of side effects. Or maybe the cost is too high, and you’re rationing pills. These aren’t excuses-they’re real barriers. And they’re common. A study in the Annals of Internal Medicine found that for every extra pill you have to take each day, your chance of sticking to the schedule drops by about 16%. So if you’re on five different meds, taken at three different times a day, you’re fighting a 60%+ drop in adherence. That’s not just hard-it’s nearly impossible without help. The good news? You don’t have to do it alone. Start with simple tools. A pill organizer with days of the week and morning/afternoon/evening slots costs less than $10. Set phone alarms labeled “AM Blood Pressure” or “Insulin Before Breakfast.” Use apps like Medisafe or MyTherapy that send reminders and track your history. If you’re traveling, bring extra pills in your carry-on. Never rely on pharmacies abroad. Talk to your pharmacist. They’re not just the person who hands you the bottle. They’re trained to spot timing conflicts, simplify regimens, and even suggest combination pills that reduce your daily count. Many pharmacies offer free medication reviews. Use them. Ask your doctor to use the “teach-back” method: after they explain your schedule, ask you to repeat it back. If you can’t say it clearly, they haven’t explained it well enough. That’s on them-not you.
What Happens When You Skip-Real Stories
One woman in Perth, 72, skipped her heart medication for three days because she felt “fine.” She didn’t have chest pain. No dizziness. But her blood pressure climbed silently. On the fourth day, she collapsed at home. Paramedics found her with a stroke. She survived, but lost movement on her right side. Her doctor said: “If you’d taken those pills, this wouldn’t have happened.” A man in his 50s stopped his antibiotics after five days because his cough was gone. Two weeks later, he was back in the hospital with pneumonia. The bacteria had come back stronger. He needed IV antibiotics. He missed two weeks of work. His insurance bill jumped by $8,000. These aren’t rare. They’re routine. The U.S. Department of Health and Human Services estimates that medication non-adherence causes 125,000 deaths every year in the U.S. alone. That’s more than traffic accidents. And it’s mostly preventable.How to Build a Habit That Lasts
You don’t need willpower. You need a system. Link your pills to something you already do every day. Take your morning meds right after brushing your teeth. Put your evening pills next to your coffee mug. If you drink coffee every day, you’ll take your pill every day. That’s how habits stick. Keep a simple log. Write down each dose you take. No fancy app needed-just a notebook or a note on your phone. If you miss one, write why. Was it forgetfulness? A change in routine? A side effect? That’s your data. Bring it to your next appointment. Your doctor can adjust timing, switch meds, or help you solve the problem. If you’re on multiple meds, ask if any can be combined. Some drugs come in one pill that does two jobs. Fewer pills = fewer chances to miss one. And if cost is the issue? Talk to your pharmacist. Many drugmakers have patient assistance programs. Some pharmacies offer $4 generics. Medicare Part D and private insurers have programs to reduce out-of-pocket costs. You don’t have to choose between eating and taking your medicine.
When to Call Your Doctor
If you miss a dose, don’t panic. But do act. Most medications say what to do on the label: “If you miss a dose, take it as soon as you remember. If it’s almost time for the next dose, skip the missed one.” But not all are the same. For blood thinners, diabetes meds, or seizure drugs, the rules are strict. Call your doctor or pharmacist immediately if you miss one. Don’t guess. Don’t double up unless they tell you to. If you’re consistently forgetting, or if side effects are making you want to stop, tell your provider. There’s almost always a better option. A different time of day. A different formulation. A different drug. Your health isn’t a checklist. It’s a rhythm. And your medication is part of that rhythm. Skip a beat, and the whole song changes.What happens if I skip one dose of my blood pressure medication?
Skipping one dose can cause your blood pressure to rise suddenly, increasing your risk of stroke, heart attack, or kidney damage-even if you feel fine. Blood pressure meds work best when taken at the same time every day to keep levels steady. If you miss a dose, take it as soon as you remember, unless it’s close to your next scheduled dose. Never double up. Always check your label or call your pharmacist for specific instructions.
Can I stop taking antibiotics when I feel better?
No. Stopping antibiotics early lets the strongest bacteria survive and multiply. These surviving bacteria can become resistant to the drug, making future infections harder to treat. You might feel better before all the bacteria are gone. That doesn’t mean the infection is gone. Always finish the full course, even if symptoms disappear.
Why do some pills need to be taken with food and others on an empty stomach?
Food can change how your body absorbs a drug. Some medications are absorbed better with food-it helps reduce stomach upset or boosts effectiveness. Others are blocked by food, so they must be taken on an empty stomach to work properly. For example, certain antibiotics like tetracycline won’t work if taken with dairy. Always follow the label: “take with food,” “take 1 hour before meals,” or “take on empty stomach.”
How can I remember to take my meds if I’m forgetful?
Use a pill organizer with compartments for each time of day. Set alarms on your phone labeled with the medication name. Link your doses to daily habits like brushing your teeth, eating breakfast, or turning off the lights. Many pharmacies offer free pill organizers and reminder services. Ask your pharmacist about medication therapy management programs-they can help simplify your routine.
Is it safe to split pills or crush them to make them easier to take?
Only if your doctor or pharmacist says it’s okay. Some pills are designed to release medicine slowly over time. Crushing or splitting them can cause too much drug to enter your system at once, leading to dangerous side effects. Others have coatings that protect your stomach or prevent absorption in the wrong part of your gut. Never alter a pill without professional advice.
What should I do if I can’t afford my medication?
Talk to your pharmacist. Many drug manufacturers offer free or low-cost programs for people who qualify. Some pharmacies sell generic versions for as little as $4 per month. Medicare Part D and private insurers have cost-reduction plans. Never skip doses because of cost-there are solutions. Your health is worth the effort to find them.



Karandeep Singh - 1 December 2025
u forgot to mention the 3am panic when u realize u missed the pill n ur phone died
Lauryn Smith - 2 December 2025
I used to skip my BP meds until I started linking them to brushing my teeth. Now I don't even think about it. Habit > willpower.
Suzanne Mollaneda Padin - 3 December 2025
As a pharmacist in rural Ohio, I see this daily. People skip doses because they can't afford them, not because they're careless. We have $4 generics and patient assistance programs-ask. No one should choose between food and life-saving meds.
Bonnie Youn - 3 December 2025
You’re not lazy if you forget-you’re just not set up for success. Get a pillbox. Set alarms. Call your pharmacy. Your future self is begging you to start today 💪
Edward Hyde - 5 December 2025
This article reads like a pharmaceutical ad written by a cult leader. 'Never skip a dose'-except when the cost is $500/month and your insurance says 'nope'. Wake up. The system is rigged.
Debbie Naquin - 6 December 2025
The pharmacokinetic instability induced by erratic dosing creates nonlinear plasma concentration curves, which in turn compromise therapeutic efficacy and elevate toxicological risk. The body operates on circadian biochemistry-not your calendar. Skipping doses doesn't just 'risk' outcomes-it actively destabilizes homeostatic equilibrium.
Mary Ngo - 6 December 2025
Did you know the FDA is secretly funded by Big Pharma to scare people into taking pills? Your blood pressure doesn't need 'stabilizing'-it needs less stress, more meditation, and zero chemical interference. The real epidemic is pharmaceutical dependency.
Alexander Williams - 7 December 2025
Warfarin INR swings aren't 'medical emergencies'-they're data points. If your doctor can't manage your dosing with regular monitoring, they're not doing their job. Blaming patients for non-adherence ignores systemic failures in care coordination.
Charlotte Collins - 9 December 2025
The 125,000 deaths/year stat? Total myth. It's calculated by assuming every hospitalization where a patient wasn't 'adherent' was caused by non-adherence. Correlation ≠ causation. And who's to say those people weren't better off off the meds?
Amber-Lynn Quinata - 11 December 2025
I skipped my diabetes meds for a week because I was 'feeling great'... and then I blacked out at the grocery store. Woke up in the ER. My husband cried. I cried. Now I take them with my coffee every morning. 🥺☕️
James Allen - 11 December 2025
Americans are so weak. Back in my day, we took our pills like soldiers. No alarms. No pillboxes. Just grit. Now everyone needs an app to remember to swallow a tiny white thing. We’re becoming a nation of hypochondriacs with smartphones.
Rachel Stanton - 13 December 2025
If you're on five meds, ask your doctor about combination pills. I went from 12 pills/day to 4. Life changed. Also-pharmacists are your secret weapon. They know the shortcuts. Use them. You don't have to suffer in silence.