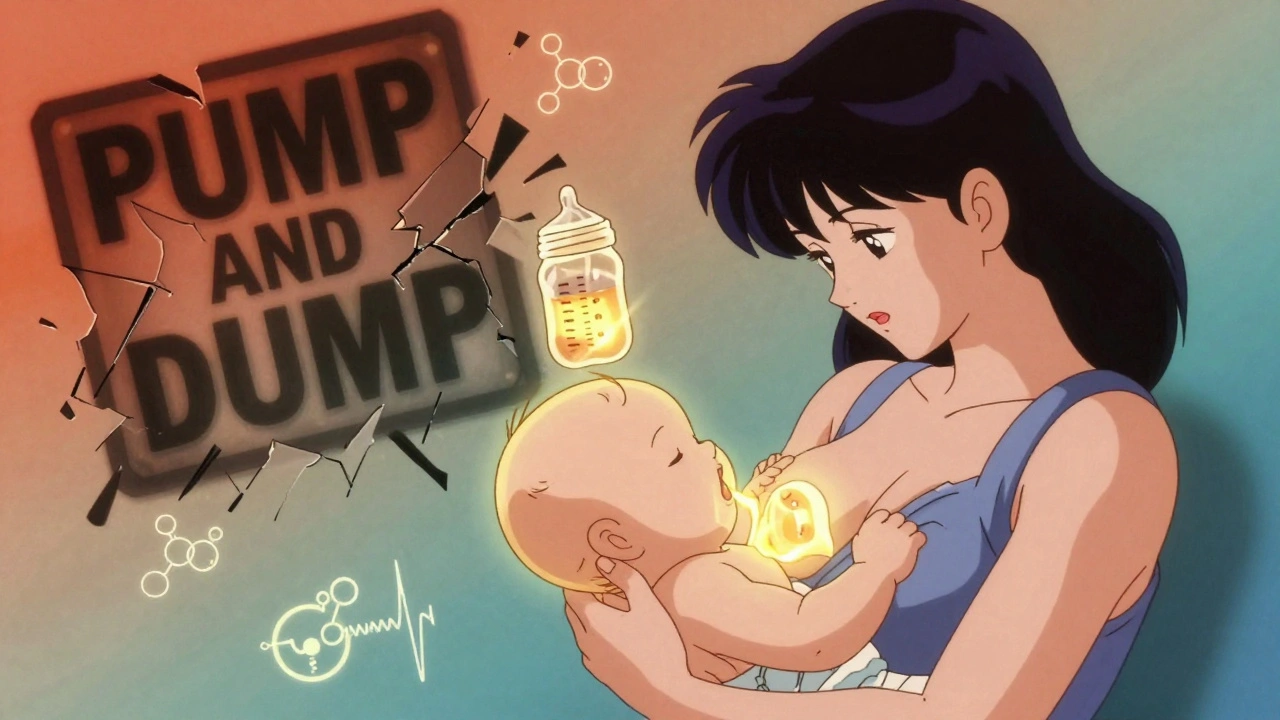
Most new mothers are told to pump and dump when they need to take medicine-antibiotics, painkillers, even antidepressants. But here’s the truth: in nearly every case, you don’t have to. Discarding your breast milk isn’t just unnecessary-it can hurt your supply, stress you out, and make feeding harder than it already is. The real answer isn’t throwing milk away. It’s knowing when to pump, how to store it, and which meds are actually safe.
Why Pump and Dump Is Usually Wrong
The idea that you must dump your milk after taking medicine comes from old warnings on drug labels. Those labels say "avoid during breastfeeding" not because the medicine is dangerous, but because manufacturers don’t want to get sued. The American Academy of Pediatrics says less than 2% of medications are unsafe for breastfeeding. That means 98% are fine.Dr. Thomas Hale, who wrote the go-to guide Medications and Mother’s Milk, found that only 0.7% of commonly prescribed drugs are risky enough to require stopping breastfeeding. Most medicines transfer into breast milk in tiny amounts-so small they don’t affect your baby. For example, when you take 650 mg of acetaminophen, your baby gets less than 0.1% of your dose through breast milk. That’s less than what they’d get from a drop of medicine.
Yet, a 2021 study in the Journal of Human Lactation found that 68% of mothers were told to pump and dump-even when taking safe meds like ibuprofen or amoxicillin. That’s not just misleading. It’s harmful. One mom in Chicago pumped and dumped for three days after being told to avoid antibiotics. Her milk supply dropped by 40%. She never got it back.
How Medications Actually Move Into Breast Milk
Not all drugs behave the same way. The science behind how much gets into your milk depends on a few key things:- Molecular size: If the drug molecule is bigger than 500 Daltons, it’s unlikely to pass into milk. Most prescription meds are too large to cross easily.
- Protein binding: If the drug sticks tightly to proteins in your blood (over 80%), it can’t float freely into your milk.
- Half-life: How long it stays in your system matters. Drugs with a short half-life (under 4 hours) clear out fast. That’s why timing helps.
- Oral absorption in babies: Even if a little drug gets into your milk, your baby’s gut might not absorb it well. Many meds just pass right through.
Take sertraline (Zoloft), a common antidepressant. Studies show it transfers at 0.5-2.5% of the mother’s dose. In over 1,000 cases tracked by LactMed, only 1.3% of babies showed any possible side effect-and those were mild, like fussiness. Compare that to paroxetine, which transfers more and has been linked to more infant reactions. The difference isn’t just in the drug-it’s in the science.
Safe Pain Relief: Ibuprofen vs. Naproxen
Pain is common after birth. But not all painkillers are equal when you’re breastfeeding.Ibuprofen (Advil, Motrin) is one of the safest. It transfers in amounts so low-0.02 to 0.1 mg/L-that it’s practically negligible. The relative infant dose is just 0.01% of your weight-adjusted dose. No documented harm in thousands of cases.
Naproxen (Aleve) is different. It has a 14-hour half-life. That means it lingers. Between 2018 and 2022, LactMed recorded three cases of exclusively breastfed newborns under one month old who developed bleeding or anemia after their moms took naproxen regularly. Not common-but avoidable.
Stick with ibuprofen. Take it right after you nurse. Wait 4-6 hours before the next feed. That way, the peak concentration in your milk passes before your baby feeds again.
Antibiotics: Cephalexin vs. Clindamycin
Antibiotics are one of the most common reasons mothers are told to dump. But again, most are safe.Cephalexin (Keflex) is a top choice. In over 1,200 reported cases, no adverse effects were found in babies. The relative infant dose is only 0.5-1.5%. Penicillin and amoxicillin are just as safe.
Clindamycin (Cleocin) is another story. It transfers at 5-15% of the maternal dose. Studies show 12% of breastfed babies get diarrhea when their moms take it. Not always serious, but enough to warrant caution. If you’re prescribed clindamycin, monitor your baby closely for loose stools or fussiness. Talk to your doctor about alternatives.
Don’t assume all antibiotics are dangerous. Most aren’t. Ask your provider: "Is this safe for breastfeeding?" If they don’t know, ask them to check LactMed.
When Timing Matters More Than Dumping
The biggest mistake? Dumping milk instead of timing your doses.Here’s how to do it right:
- Take your medication right after you nurse. That gives your body time to clear it before the next feed.
- If you take it once a day, do it after the longest stretch your baby sleeps-usually at night.
- If you take it multiple times a day, space it out. Nurse right before each dose.
- For short-acting meds (like ibuprofen or amoxicillin), wait 4-6 hours before the next feed.
- For longer-acting meds, check LactMed or call MotherToBaby for specific timing.
This strategy keeps your milk supply steady and your baby safe. Interrupting breastfeeding-even for 24 hours-can slash your supply by 30-50%, according to Breastfeeding Medicine. And once it’s gone, it’s hard to get back. One mom in Texas pumped and dumped for a week because she was scared. She had to switch to formula permanently.
Storage Rules Don’t Change
You might think meds change how long milk lasts. They don’t. Your milk stays safe under the same rules whether you’re on medication or not:- Room temperature (up to 25°C): 4 hours
- Fridge (4°C or colder): 4 days
- Freezer (-18°C): 6 months
Label your containers with the date and time you pumped. If you’re taking a med that’s safe, store the milk normally. No need to throw it out. No need to label it "medicated." The milk isn’t contaminated-it’s just milk.
What to Do If You’re Unsure
You don’t have to guess. There are free, reliable resources:- LactMed (from the National Institutes of Health): Updated weekly. Covers over 1,300 drugs with scientific references. Search by drug name or condition.
- MotherToBaby (866-626-6847): Free, confidential advice from experts. They speak multiple languages and can walk you through your specific meds.
- InfantRisk Center: Offers a free app with real-time safety ratings. Downloaded over 250,000 times.
Don’t rely on your pharmacist’s general advice or a drug label. Those are often outdated or overly cautious. LactMed is the gold standard. Hospitals across the U.S. use it now-your provider should too.

What Your Doctor Might Not Tell You
Here’s the uncomfortable truth: most doctors aren’t trained in breastfeeding pharmacology. A 2021 survey found only 32% of obstetricians and 28% of family doctors could correctly name a safe antidepressant for breastfeeding mothers.If your provider says "dump it," ask: "Can you check LactMed?" Or say: "I read that sertraline is safe. Can we confirm that?" Most will appreciate you being informed. If they push back, ask for a referral to a lactation consultant.
La Leche League and the International Lactation Consultant Association both have free decision trees and guides. Use them. You’re not being difficult-you’re being smart.
Real Stories, Real Outcomes
On Reddit’s breastfeeding community, 63% of mothers said they were told to dump milk unnecessarily. Many reported losing supply, feeling guilty, or switching to formula.But here’s what happens when you do it right:
- A mom in Texas took sertraline while breastfeeding her 6-week-old. She timed her doses after nighttime feeds. Her baby slept fine. No fussiness. No issues.
- A mom in Australia took cephalexin for a UTI. She pumped and stored milk normally. Her supply stayed strong. Her baby stayed healthy.
- A mom in California was told to stop breastfeeding while on antibiotics. She called MotherToBaby. They said it was safe. She kept nursing. Her supply didn’t drop.
These aren’t rare exceptions. They’re the norm-if you have the right info.
What’s Changing in 2025
The tide is turning. In 2023, the American Academy of Pediatrics updated its guidelines to say: "The benefits of breastfeeding generally outweigh theoretical risks of medication exposure for nearly all pharmaceuticals."The FDA is now requiring drug labels to include more specific breastfeeding info-no more blanket "avoid" warnings. By 2024, new drugs will have clearer guidance. And the CDC’s 2023-2025 plan aims to eliminate unnecessary barriers to breastfeeding during medication use.
That means the future is clearer. But right now, you still have to be your own advocate. Don’t wait for your doctor to know everything. Use LactMed. Call MotherToBaby. Trust the data, not the fear.
Do I need to pump and dump if I take ibuprofen?
No. Ibuprofen is one of the safest pain relievers for breastfeeding mothers. It transfers in extremely small amounts-less than 0.01% of your dose-and has no documented harm to infants. Take it right after nursing, and wait 4-6 hours before the next feed to minimize exposure. There’s no need to dump your milk.
Is it safe to breastfeed while taking antidepressants?
Yes, most are. Sertraline (Zoloft) is the most studied and safest option, with a relative infant dose of only 0.5-2.5%. Paroxetine and fluoxetine transfer more and may cause fussiness in some babies. Always check LactMed or call MotherToBaby for personalized advice. The benefits of treating your depression usually outweigh any small risk to your baby.
How long should I wait after taking medication before breastfeeding?
For most short-acting meds (like ibuprofen or amoxicillin), wait 4-6 hours after taking the dose. For longer-acting drugs, check LactMed. The best strategy is to take your medication right after you nurse-this gives your body time to clear it before the next feeding. Avoid taking meds right before a feed.
Can I store milk that I pumped while on medication?
Yes, if the medication is safe for breastfeeding. Medications don’t change how long milk lasts. Store it the same way you normally would: 4 hours at room temperature, 4 days in the fridge, 6 months in the freezer. Only discard milk if you’re taking a drug that’s known to be unsafe-like certain chemotherapy agents or radioactive isotopes.
What if my doctor says to stop breastfeeding?
Ask them to check LactMed or refer you to MotherToBaby (866-626-6847). Most doctors aren’t trained in breastfeeding pharmacology. Over 90% of medication cases reviewed by InfantRisk Center result in recommendations to continue breastfeeding with proper timing. Don’t accept a blanket "stop" without evidence. Your milk supply and your baby’s health depend on accurate info.
Next Steps
If you’re currently on medication and breastfeeding:- Go to LactMed and search your drug.
- Call MotherToBaby at 866-626-6847 if you’re unsure.
- Time your doses after nursing, not before.
- Store your milk normally-don’t dump unless the drug is confirmed unsafe.
- Share this info with your partner, family, or support group. You’re not alone.
You don’t have to choose between being healthy and feeding your baby. With the right knowledge, you can do both.




Ben Choy - 4 December 2025
This is so needed. I was told to dump for ibuprofen after my c-section. Lost 30% of my supply in 48 hours. No one told me it was safe. Thank you for putting this out there.
😭
Bill Wolfe - 6 December 2025
I'm genuinely astonished that anyone still believes the outdated "pump and dump" dogma in 2025. The science is unequivocal: less than 1% of medications pose any measurable risk, and even then, the infant's gut absorption is often negligible. The fact that medical professionals continue to propagate fear-based misinformation speaks to a systemic failure in pharmacological education. LactMed has been the gold standard for decades, yet hospitals still rely on outdated drug inserts printed in the 90s. This isn't just negligence-it's malpractice disguised as caution. If you're still dumping, you're not protecting your baby-you're betraying your own biology and your right to informed consent.
Rudy Van den Boogaert - 6 December 2025
I took amoxicillin while nursing my twins and just stored it like normal. No issues. My pediatrician didn’t even blink when I told him I didn’t dump. He just said, 'Good. That’s what we recommend.'
Why do people still think this is risky?
George Graham - 7 December 2025
I’m a dad, and I didn’t know any of this until my wife went through it. I thought dumping was the rule, not the exception. I’ve been sharing this post with every new parent I know. The guilt and confusion new moms face around meds is so unnecessary. This isn’t just medical advice-it’s emotional relief.
Thank you for writing this.
John Filby - 8 December 2025
Just took my first dose of sertraline and I’m storing milk like normal. I called MotherToBaby before even telling my doctor. They said it was fine. I feel so much better now. I was so scared I was gonna mess up my baby.
Also-why do we still have to fight for this? It’s 2025.
Elizabeth Crutchfield - 10 December 2025
i just dumped for 3 days b/c my dr said to. now my supply is gone. i cry every time i pump. this post made me feel less alone.
Augusta Barlow - 10 December 2025
Let’s be real-this whole thing is a corporate ploy. Big Pharma doesn’t want you to know meds are safe because then you wouldn’t panic-buy formula. And hospitals? They make money off formula partnerships. Look at the funding sources for the AAP guidelines. Who’s really behind this? The same people who told you vaccines cause autism. This isn’t science-it’s profit-driven fear. And they’re using new moms as bait.
Rebecca Braatz - 11 December 2025
If you’re reading this and you’re scared-stop. You’re not failing. You’re not broken. You’re doing the best you can with the info you were given. But now you have better info. Go to LactMed. Call MotherToBaby. Store your milk. Keep nursing. You’re not just feeding your baby-you’re teaching them that their body is safe, strong, and trusted. That’s the real legacy.
And if someone tells you to dump? Tell them you’re done listening to fear. You’re done.
Michael Feldstein - 12 December 2025
My wife took clindamycin and our baby got really fussy for a day. We didn’t dump-we just timed it after feeds and cut back to once a day. Baby was fine by day 3. The key isn’t dumping-it’s awareness. This post is a game-changer.
jagdish kumar - 14 December 2025
We are all just trying to survive motherhood. The system gives us fear. The truth gives us power. Choose power.
michael booth - 14 December 2025
The empirical data supporting the safety of most medications during lactation is overwhelming. It is therefore both scientifically and ethically imperative that healthcare providers prioritize evidence-based guidance over anecdotal or precautionary advice. The persistence of the pump-and-dump paradigm reflects a critical gap in continuing medical education. This is not a matter of opinion-it is a matter of public health.
Heidi Thomas - 15 December 2025
I’ve seen so many moms get gaslit by their doctors. I’m a nurse. I’ve seen the charts. Most OBs can’t tell you the half-life of ibuprofen. Don’t trust your provider’s memory. Go to LactMed yourself. Don’t wait. Don’t ask. Just look. And if they argue? Walk out. Your milk is worth more than their ego.