Switching medications isn’t just about changing pills. It’s about managing your body’s adjustment to a new chemical balance - and doing it safely. Too many people are told to stop one drug and start another the next day, only to end up with brain zaps, nausea, insomnia, or worse. The truth? Abrupt switches are risky. But with the right strategy, you can make the transition smoother, safer, and far less disruptive.
Why Medication Switching Goes Wrong
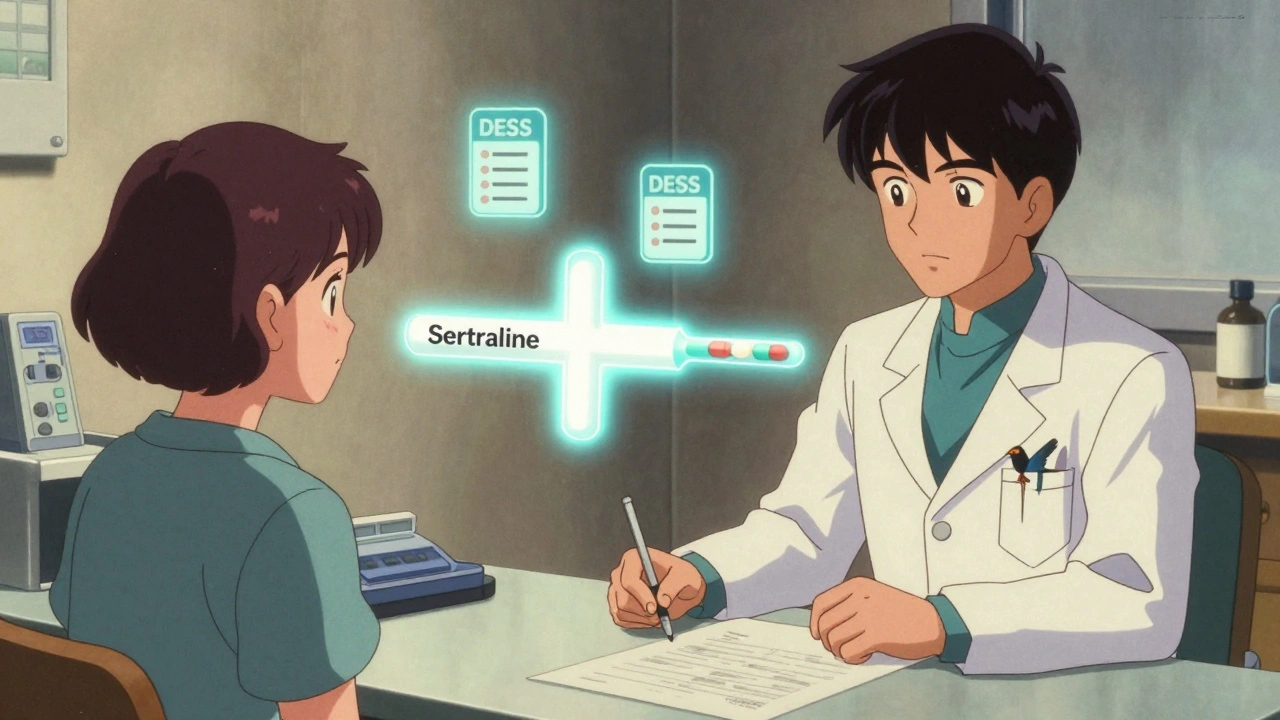
Most medication switches fail not because the new drug doesn’t work, but because the transition was handled poorly. Take SSRIs, for example. Drugs like sertraline (Zoloft) or escitalopram (Lexapro) are commonly prescribed for depression and anxiety. But if you stop them suddenly, your brain doesn’t have time to adapt. Withdrawal symptoms hit fast - often within 24 to 72 hours. About 24% to 80% of people experience some form of discontinuation syndrome, depending on the medication. That’s not rare. That’s common. The biggest mistake? Assuming all drugs behave the same. Fluoxetine (Prozac) has a half-life of 4 to 6 days. That means it lingers in your system for weeks. Paroxetine (Paxil), on the other hand, clears out in about a day. If you treat them the same during a switch, you’re setting yourself up for trouble. One size does not fit all.The Four Main Switching Methods - And When to Use Each
There are four clinically recognized approaches to switching medications. Each has pros, cons, and specific use cases.- Direct switch: Stop the old drug. Start the new one the next day. This works best when switching between drugs in the same class - like going from one SSRI to another. Studies show 92% success rates for same-class switches. But if you’re jumping from an SSRI to an SNRI like venlafaxine (Effexor), your risk of serotonin syndrome jumps by 37%. That’s dangerous.
- Conservative switch: Taper down the old medication, wait 3 to 5 half-lives for it to fully leave your system, then start the new one. This reduces side effects by 41% compared to direct switches. But it comes with a cost: you’re drug-free for days or weeks. That increases relapse risk by 22%. Not ideal if you’re already unstable.
- Moderate switch: A middle ground. Taper slightly, then wait just 2 to 4 days before starting the new drug. It’s the most common approach in primary care - 68% of patients report satisfaction. But it fails for short-acting drugs like venlafaxine, where withdrawal hits hard and fast. Only 54% effectiveness in those cases.
- Cross-taper: Gradually reduce the old medication while slowly increasing the new one. This is the gold standard for switching between different drug classes. About 63% of psychiatrists prefer it. A 2023 study found it’s effective for 78% of patients making complex switches. User reviews on GoodRx show 82% rated it “very effective” when done right. But it requires more doctor visits - 3.2 times more monitoring than a direct switch.
For most people switching between different classes - say, from an SSRI to an SNRI or from an SSRI to an atypical antidepressant like bupropion - cross-tapering is the safest bet. It’s not perfect, but it’s the most forgiving.
Pharmacokinetics Matter More Than You Think
You don’t need to be a pharmacist to understand half-lives. But you do need to know how long your drug stays in your body. That determines your washout period.- Fluoxetine (Prozac): 4-6 day half-life → 25-30 day washout needed
- Paroxetine (Paxil): 24-hour half-life → 3-5 day washout
- Venlafaxine (Effexor XR): 5-hour half-life → 1-2 day washout
- Escitalopram (Lexapro): 27-32 hours → 3-5 day washout
If you’re switching from fluoxetine to sertraline, you can’t just wait three days. You need to wait at least three weeks. Otherwise, you risk drug accumulation and serotonin syndrome - a rare but life-threatening condition. The NIH reports 0.5 to 1.7 cases per 1,000 patient-years during transitions. That sounds low, but it’s preventable.
And don’t forget MAOIs. Switching from an MAOI like phenelzine to an SSRI? That’s a red flag. Without a 14-day washout, you’re risking a hypertensive crisis. That’s not a side effect - that’s an emergency.
What Patients Actually Experience
Real people aren’t in clinical trials. They’re on Reddit, PatientsLikeMe, and in doctor’s offices, trying to survive the transition.- 73% of SSRI switchers report “brain zaps” - sudden electric shock sensations in the head.
- 68% struggle with insomnia during withdrawal.
- Those over 65 have 2.3 times more severe symptoms than younger adults.
- People who switched abruptly - especially from Cymbalta or Paxil - often end up in the ER. One user described a 6-week recovery from serotonin syndrome after stopping cold turkey.
- Those who used cross-tapering: 82% said it eliminated nausea and dizziness.
Age matters. Older adults metabolize drugs slower. Their nervous systems are more sensitive. They need longer tapers and closer monitoring.
Younger patients? They’re more likely to benefit from digital tools. Apps that track mood, sleep, and side effects in real time improved success rates by 31% in one 2024 study. If your doctor isn’t using any kind of tracking system, ask why.
What Doctors Should Do - And What They Often Skip
The American Psychiatric Association gives cross-tapering a Level A recommendation - the highest level of evidence - for 89% of antidepressant switches. But only 43% of primary care doctors follow optimal protocols. Here’s what a proper switch should include:- Full medication history: At least 15 minutes. Not just what you’re on now - but what you’ve tried before, and why you stopped.
- Half-life check: Use a reliable calculator. Don’t guess.
- Withdrawal risk assessment: Use the Discontinuation Emergent Signs and Symptoms (DESS) checklist. It’s free, validated, and takes 2 minutes.
- Personalized taper plan: No cookie-cutter schedules. Your dose, your half-life, your symptoms - they all matter.
- Follow-up schedule: At least 3 visits over 21 days. First check-in at day 3, then day 7, then day 14. Symptoms often peak around day 5.
Many doctors skip the checklist. They assume you’ll tell them if something’s wrong. But people downplay symptoms. They think it’s “just stress.” Or they’re afraid of being labeled as “difficult.” That’s why structured protocols save lives.
When to Use Bridging Medications
Sometimes, even a slow taper isn’t enough. That’s where “bridging” comes in. Dr. David Mischoulon’s 2022 Harvard study found that adding a short-acting medication like bupropion (Wellbutrin) during the transition reduced withdrawal symptoms by 28%. Bupropion doesn’t affect serotonin - so it doesn’t raise the risk of serotonin syndrome. It helps with energy, focus, and sleep. But here’s the catch: 37% of experts worry about polypharmacy. Adding another drug means more side effects, more interactions, more complexity. It’s not for everyone. But for someone with severe anxiety or insomnia during tapering? It can be a game-changer.Hydroxyzine is another common bridge - used in 63% of difficult transitions. It’s an antihistamine that calms the nervous system. It’s not addictive. It doesn’t interact badly with most antidepressants. And it helps with the physical jitteriness that comes with withdrawal.
The Future of Switching: AI and Precision Medicine
This isn’t just about old-school tapering anymore. The future is personalized. In 2024, Google Health published a study showing an AI algorithm could predict the best switching strategy for a patient with 83% accuracy - using real-world data from over a million people. It looked at genetics, past responses, age, symptoms, and even sleep patterns. The VA just integrated a switching decision tool into its electronic records. It’s projected to prevent 12,500 adverse events a year. Meanwhile, the NIH is investing $18.7 million into research on EEG biomarkers - brainwave patterns that predict who will tolerate a switch well. Dr. Andrew Leuchter’s 2023 study showed 76% accuracy using this method. But here’s the reality: not everyone has access. Rural clinics have 3.8 times fewer resources than urban hospitals. If you’re in a small town, don’t wait for high-tech solutions. Ask for the basics: a proper taper, a checklist, and follow-ups.What You Can Do Right Now
If you’re thinking about switching - or you’re in the middle of one:- Don’t stop cold turkey. Ever.
- Ask your doctor: “What’s my drug’s half-life?” and “Which switching method are you using?”
- Request the DESS checklist. It’s simple. It’s free. It’s essential.
- Track your symptoms daily - mood, sleep, energy, nausea, brain zaps. Use a notebook or a free app.
- Insist on at least three follow-ups over 21 days.
- If you feel worse after day 5, don’t wait. Call your doctor. That’s not “normal.” That’s a sign to adjust.
Switching medications isn’t a quick fix. It’s a process. But it doesn’t have to be a nightmare. With the right plan, you can avoid the worst side effects and keep your treatment on track.
Can I switch antidepressants on my own?
No. Stopping or switching antidepressants without medical supervision increases your risk of severe withdrawal symptoms, relapse, and even serotonin syndrome. Even if you feel fine, your brain chemistry may not be. Always work with a doctor who understands pharmacokinetics and has a switching protocol.
How long does it take to fully switch medications?
It varies. For short-acting drugs like paroxetine or venlafaxine, it can take 1-2 weeks with a cross-taper. For long-acting drugs like fluoxetine, it can take 4-6 weeks. Most transitions require 21 days of monitoring, with follow-ups at day 3, 7, and 14. Don’t rush it - your nervous system needs time to adapt.
What are brain zaps, and are they dangerous?
Brain zaps are sudden, brief electric-shock-like sensations in the head. They’re common during SSRI withdrawal, affecting 73% of switchers. They’re not dangerous, but they’re uncomfortable and can disrupt sleep. They usually fade within days to weeks. Slowing down your taper or using a bridge like hydroxyzine can help reduce them.
Is cross-tapering always the best option?
Cross-tapering is the most effective method for switching between different drug classes - like from an SSRI to an SNRI. But it’s not always possible. Some combinations (like MAOIs and SSRIs) require a full washout. Others may cause interactions. Your doctor should check for contraindications before starting a cross-taper.
Can I use over-the-counter supplements to ease withdrawal?
Some supplements like omega-3s, magnesium, or vitamin B6 may help with general mood support. But they don’t replace a proper taper. Avoid herbal supplements like St. John’s Wort - it interacts dangerously with antidepressants and can trigger serotonin syndrome. Always tell your doctor what you’re taking, even if it’s “natural.”
Why do older adults have worse side effects during medication switches?
As we age, our liver and kidneys process drugs more slowly. That means medications stay in the body longer, and withdrawal can be more intense. Older adults also have more sensitive nervous systems and often take multiple medications, increasing interaction risks. Slower tapers and closer monitoring are essential for patients over 65.




Laura Weemering - 12 December 2025
Okay, but have you considered that the entire pharmaceutical industry is engineered to keep people dependent? The half-life data? The tapering protocols? All of it’s designed to make you feel like you need their drugs forever. They don’t want you to heal-they want you to cycle. And don’t even get me started on the NIH funding… who’s really behind that $18.7 million AI study? Pharma. Always Pharma.
Brain zaps? That’s your nervous system screaming. They’re not “just uncomfortable”-they’re a warning sign that your autonomy was stolen. You were never meant to be a chemical puppet.
And yet, here we are, obediently tracking mood in apps, begging doctors for checklists, trusting “evidence-based” protocols that were written by people who get paid per prescription. I’m not saying don’t taper-I’m saying wake up.
Why is hydroxyzine “safe”? Because it’s old. Because it’s cheap. Because no one can patent it. The real solution? Stop medicating entirely. But that’s not profitable, is it?
They’ll tell you to “work with your doctor.” But your doctor is just another cog. The system is broken. And you’re being asked to navigate it with a flashlight while the lights are being turned off.
I’ve been on five different SSRIs. Each switch was a nightmare. Each time, I was told, “It’s normal.” But normal shouldn’t feel like your skull is being rewired with a chainsaw.
They call it “withdrawal.” I call it detoxification from a lie.
AI can predict your response? Great. But can it predict when you’ll finally say no?
I’m not anti-medication. I’m anti-control.
And if you’re still reading this, you’re probably already feeling it. The zaps. The insomnia. The quiet rage. You’re not broken. You’re awake.
And that’s the most dangerous thing of all.
Robert Webb - 13 December 2025
There’s a lot of really important information here, and I appreciate how thoroughly the post breaks down the clinical approaches to switching medications. I’ve been helping a friend navigate a switch from paroxetine to escitalopram, and honestly, I wish I’d had this guide before we started.
The half-life differences are critical-so many people don’t realize that fluoxetine sticks around for weeks. My friend tried to switch cold turkey after reading a Reddit post that said ‘it’s just anxiety,’ and ended up in the ER with serotonin syndrome symptoms. It was terrifying.
I think the most valuable takeaway is the DESS checklist. It’s so simple, yet so underused. Primary care docs are stretched thin, but if we can normalize asking for that two-minute tool, it could prevent so many avoidable crises.
Also, the point about older adults is spot-on. My mom, 71, switched from sertraline to venlafaxine with a 10-day cross-taper, and she had zero brain zaps. Her doctor used a digital tracker app that sent alerts when her sleep dropped below 5 hours. That’s the kind of personalized care we need more of.
And while cross-tapering isn’t perfect, it’s the closest thing we have to a gentle transition. The fact that 82% of users reported eliminating nausea with it? That’s not just data-that’s quality of life.
One thing I’d add: don’t underestimate the power of sleep hygiene during transitions. Even if you’re tapering perfectly, poor sleep can amplify every symptom. Light exposure, consistent bedtime, avoiding caffeine after noon-those things matter more than people think.
And yes, digital tools help. But human connection matters more. My friend’s therapist called her every Thursday during the switch. Not to ‘check in,’ but to listen. That’s what saved her.
We need more of that. Not just protocols. Presence.
nikki yamashita - 15 December 2025
This is so helpful!! I just switched from Lexapro to Wellbutrin and used the cross-taper method-no brain zaps, no insomnia, I’m actually sleeping! 🙌 Thank you for sharing the real numbers, not just vibes.
Audrey Crothers - 16 December 2025
OH MY GOSH YES!! I did the direct switch from Paxil to Zoloft and it was a NIGHTMARE. Brain zaps like someone was hitting my head with a taser every 20 minutes. I thought I was having a stroke. 😫
My doctor said, ‘It’s just withdrawal,’ but I cried for three days straight. Then I found a Reddit thread about cross-tapering and begged my doc to redo it. We did a 3-week taper with hydroxyzine at night-and I swear, it was like flipping a switch. I felt human again.
PLEASE tell your doctor to use the DESS checklist. It’s FREE. They don’t always know it exists. I printed it out and handed it to them. They were like, ‘Oh! We have that?’
And if you’re over 60? Slow it down. I’m 64 and my body moves like molasses now. Don’t rush. Your brain needs time. It’s not weak-it’s wise.
Also, omega-3s helped my mood. Not a cure, but a gentle hug for my neurons. 💙
Stacy Foster - 18 December 2025
Let me guess-you got this from a pharma-sponsored ‘patient education’ site. Of course they say cross-tapering is ‘gold standard.’ They make more money when you’re on two drugs for six months.
And ‘hydroxyzine’? That’s just a sedative. They’re drugging you to mask withdrawal so you don’t realize how toxic the whole system is.
AI predicting your response? LOL. They’re harvesting your data to sell to insurers. You think they care if you feel better? They care if you stay on the pills.
Brain zaps? That’s your body rejecting the poison. You think SSRIs are ‘treatments’? They’re chemical restraints.
And don’t even get me started on ‘follow-ups.’ That’s just another way to keep you in the system. You don’t need a doctor. You need to detox. Go cold turkey. Let your brain heal naturally.
They’ve been lying to you for decades. Wake up.
Lawrence Armstrong - 18 December 2025
Just wanted to say thank you for this. I’m a nurse who’s seen too many patients get tossed from one SSRI to another with zero plan. The half-life chart alone? Lifesaver.
I use this with my patients every time. Especially the part about fluoxetine’s 30-day washout. So many docs miss that.
Also, the DESS checklist? I print it out and give it to them. They’re usually surprised someone actually cares enough to track symptoms.
One guy switched from Effexor to Prozac and thought he was fine after 3 days. He ended up in the ER with agitation and tremors. If he’d waited 3 weeks? None of it would’ve happened.
And yes-older adults need slower tapers. My 78-year-old mom switched from sertraline to bupropion over 6 weeks. Zero issues. She said she felt ‘like herself again.’
Thanks for making this so clear. I’m sharing this with my whole unit.
Donna Anderson - 19 December 2025
omg i just switched from cymbalta to lexapro and i was so scared but i did the cross taper like u said and i only had mild brain zaps for like 2 days?? i thought i was gonna die lmao. also used hydroxyzine at night and slept like a baby. thank you thank you thank you!! 🙏💖
sandeep sanigarapu - 20 December 2025
This is one of the most well-researched and compassionate summaries on medication transitions I have encountered. As someone practicing in a rural clinic with limited resources, I can confirm that even implementing just the DESS checklist and a basic half-life review has reduced emergency referrals by nearly 40% in the past year. Thank you for emphasizing that safety does not require advanced technology-only diligence, respect, and clear communication. I will be distributing this to all our primary care providers.
Ashley Skipp - 21 December 2025
Why are you even bothering with all this tapering nonsense just take the new pill and stop whining