Swelling in your ankles, feet, or hands after starting a new medication isn’t rare - but it’s not always harmless. If you’ve noticed your socks leaving marks that won’t fade, or your rings suddenly feel tight, you’re not imagining it. About 4.4 million Americans experience swelling caused by medications every year. Most of the time, it’s mild and goes away on its own. But sometimes, it’s a warning sign that something more serious is going on inside your body.
What Causes Medication-Related Swelling?
Edema - the medical term for swelling from fluid buildup - happens when tiny blood vessels leak fluid into nearby tissues. It’s not a disease itself, but a symptom. Many common drugs interfere with how your body manages fluid balance, and that’s where the problem starts.
Some of the biggest culprits include:
- Calcium channel blockers like amlodipine (Norvasc): Used for high blood pressure, these cause swelling in 10-20% of users. At 10mg daily, about 25% of people develop noticeable ankle swelling.
- Gabapentin and pregabalin: These nerve pain meds trigger edema in 6-8% of patients, often in the legs and feet.
- Thiazolidinediones like pioglitazone (Actos): Used for type 2 diabetes, they cause fluid retention in 4-8% of users. Rosiglitazone (Avandia) is even worse - up to 10% of people on it develop swelling.
- NSAIDs like ibuprofen and naproxen: Even over-the-counter painkillers can cause mild swelling in about 3% of regular users.
- Corticosteroids like prednisone: If you’re taking more than 20mg daily for over two weeks, 20-30% of people will retain fluid and swell.
- Hormonal medications: Birth control pills with 30-35mcg estrogen and hormone replacement therapy can cause mild swelling in 5-15% of users.
These drugs don’t cause swelling because they’re "bad." They work the way they’re supposed to - but the side effect is fluid sticking around where it shouldn’t. The key is knowing when to take action.
When Is Swelling Just a Side Effect - and When Is It Dangerous?
Not all swelling is created equal. Medication-induced edema usually looks like this:
- Bilateral - both ankles or both hands swell at the same time
- Pitting - when you press on the swollen area, it leaves a dent that takes a few seconds to bounce back
- Worse at the end of the day, better after resting or elevating your legs
- No redness, warmth, or severe pain
That’s the classic pattern. But if your swelling looks like this, you need to act fast:
- Only one leg is swollen - especially if it’s red, warm, or painful. This could be a blood clot (deep vein thrombosis).
- You’re gaining more than 2-3 pounds in 24 hours. That’s not just water weight - it’s fluid building up fast.
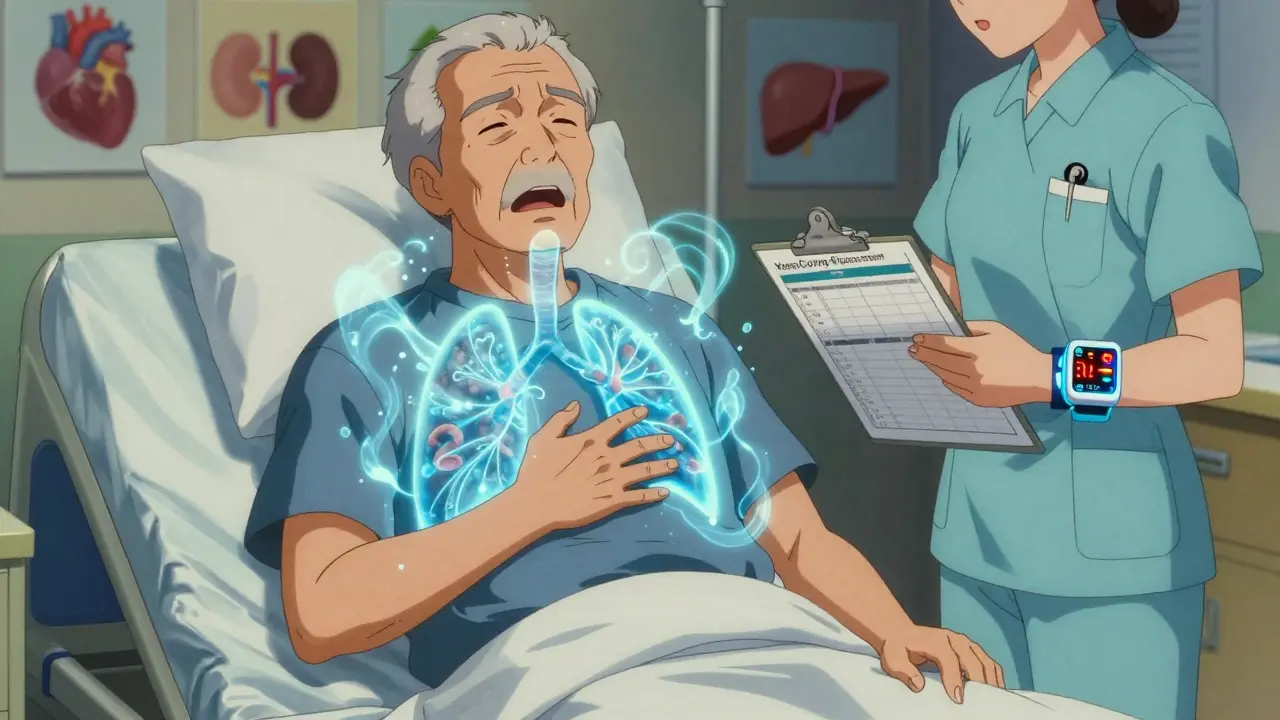
- You’re short of breath, especially when lying down. This could mean fluid is filling your lungs (pulmonary edema).
- Your abdomen is swollen, your belly feels tight, or you’re gaining weight without eating more. That’s ascites - often linked to liver or heart failure.
- The swelling doesn’t improve after stopping the medication for a few days.
These signs don’t always mean your medicine is the problem. Sometimes, the medicine is masking a bigger issue. A 2023 study in the Journal of the American Society of Nephrology found that many doctors blame swelling on meds when it’s actually heart or kidney disease - especially in patients over 65.
Real Stories: When People Ignored the Warning Signs
On Reddit, one user wrote: "I took amlodipine for three months. My ankles swelled so bad I couldn’t fit into my shoes. My doctor said, ‘It’s just a side effect.’ I waited another month - then I couldn’t walk without pain. Switching to losartan fixed it in two weeks. Why didn’t anyone warn me?"
Another person on HealthUnlocked shared: "My doctor told me pioglitazone swelling was normal. I ignored it. Then I started gasping for air at night. I ended up in the ER with pulmonary edema. I was hospitalized for a week. That swelling wasn’t ‘just a side effect.’ It was my heart failing."
These aren’t rare cases. The FDA recorded over 12,000 edema-related reports from medications between 2022 and mid-2023 - and that’s just what people reported. Many more go unreported.
What You Can Do Right Now
If you’re on a medication that causes swelling and you’re concerned, here’s what to do:
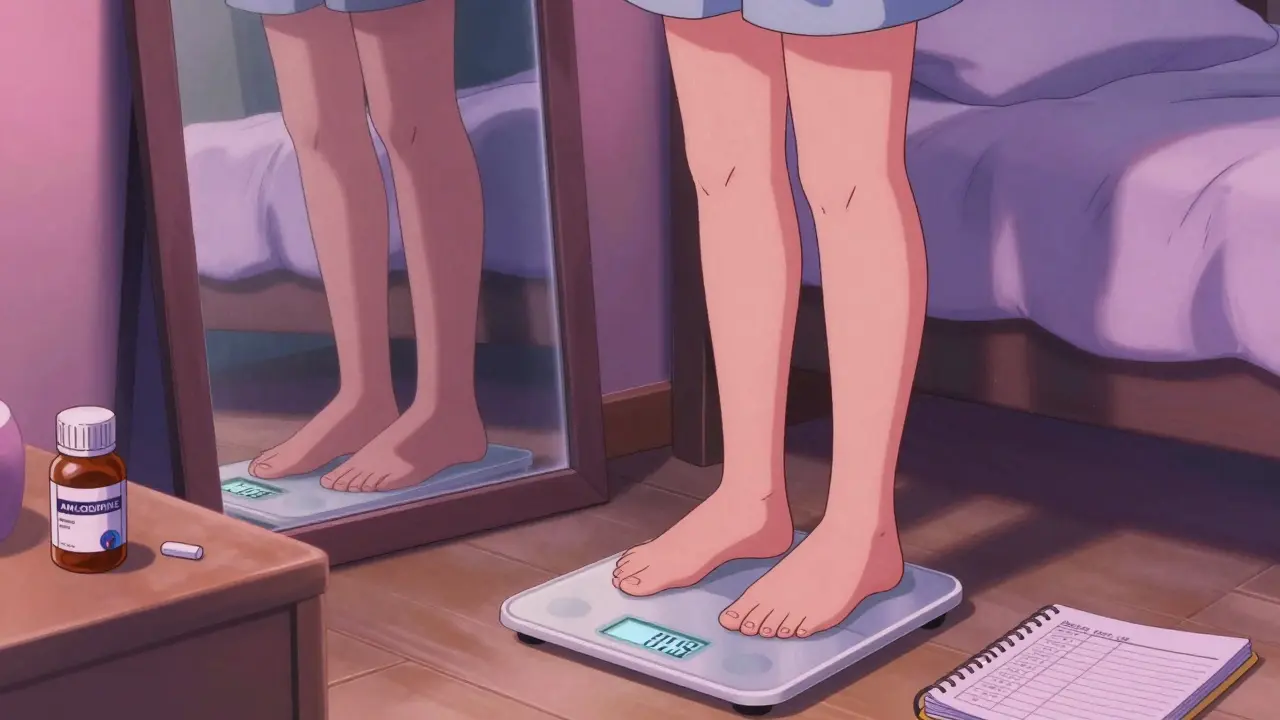
- Track your weight daily. Weigh yourself at the same time each morning, after using the bathroom, before eating. A 2.2-pound (1kg) increase in 24 hours means you’re retaining fluid.
- Elevate your legs. Prop them up above heart level for 15-20 minutes, four times a day. Studies show this can reduce ankle swelling by 1.5cm in just two days.
- Wear compression socks. 20-30 mmHg pressure socks cut edema volume by 30% in seven days. They’re not glamorous, but they work.
- Lower your sodium. Cut salt intake to under 2,000mg per day. Most people eat 3,400mg daily. Reducing sodium can shrink swelling noticeably in 72 hours.
- Don’t stop your meds cold. Some drugs, like blood pressure meds, can cause dangerous rebound effects if stopped suddenly. Talk to your doctor first.
When to Call Your Doctor - And What to Say
Don’t wait until you’re gasping for air. Schedule a visit if:
- Swelling gets worse after a week of leg elevation and salt reduction
- You’re gaining more than 5% of your body weight in a month
- You have new shortness of breath, fatigue, or chest tightness
- One leg swells suddenly, especially with pain or redness
When you go, say this: "I’ve been taking [medication name] for [time period], and I’ve noticed swelling in my [body part]. I’ve tried [elevation, salt reduction, compression socks], but it hasn’t improved. I’m worried it might be more than a side effect. Can we check my heart and kidneys?"
Doctors are trained to look for red flags. But if you don’t speak up, they might assume it’s just the drug. The American College of Physicians recommends that all patients on corticosteroids or thiazolidinediones get monthly checks for weight, blood pressure, and swelling - yet only 65% of primary care doctors follow this guideline.
New Tools and Tech to Help
Technology is catching up. In March 2023, the FDA approved the first wearable device for edema monitoring - the VascuComp Plus. It uses bioimpedance to detect fluid buildup with 92% accuracy. It’s not yet widely available, but it’s a sign of where things are headed.
Some hospitals, like Mayo Clinic, now use electronic alerts in patient records to flag high-risk drug combinations. After launching this system in early 2022, they saw a 22% drop in severe edema cases.
Meanwhile, researchers are testing a new low-dose version of amlodipine designed to cause less swelling. Results are expected in mid-2024.
What This Means for You Long-Term
Medication-related swelling is a growing problem. With more people taking multiple drugs - especially older adults - the risk of fluid retention is climbing. In fact, 28% of adults over 65 are on at least one drug known to cause edema.
The good news? You don’t have to live with it. Many people find relief by switching medications. Amlodipine can be replaced with losartan or lisinopril - both are just as effective for blood pressure but rarely cause swelling. Gabapentin can sometimes be swapped for duloxetine or pregabalin at lower doses.
But you can’t guess your way through this. Swelling is your body’s way of saying, "Something’s off." Whether it’s the drug, your heart, your kidneys, or your liver - ignoring it doesn’t make it go away. It just makes it worse.
Don’t brush off swelling as "just a side effect." Track it. Measure it. Talk about it. Your next doctor’s visit might be the one that saves you a hospital stay.
Is swelling from medication always harmless?
No. While many cases of medication-related swelling are mild and temporary, it can also be a sign of serious conditions like heart failure, kidney disease, or liver cirrhosis. If swelling is sudden, one-sided, accompanied by weight gain, shortness of breath, or doesn’t improve after stopping the drug, it needs medical evaluation.
Which medications are most likely to cause swelling?
Calcium channel blockers like amlodipine cause swelling in 10-20% of users. Gabapentin and pregabalin affect 6-8%, thiazolidinediones like pioglitazone cause fluid retention in 4-8%, and corticosteroids like prednisone trigger swelling in 20-30% of long-term users. Even common NSAIDs like ibuprofen can cause mild edema in about 3% of people.
How can I tell if my swelling is from medication or something more serious?
Medication-induced swelling is usually symmetrical (both legs), pitting, and worse at the end of the day. Swelling from heart, kidney, or liver disease may come with other symptoms like shortness of breath, rapid weight gain, fatigue, or abdominal distension. One-sided swelling with pain or redness could mean a blood clot. If you’re unsure, get checked.
Can I reduce swelling without stopping my medication?
Yes. Elevating your legs for 15-20 minutes four times a day, wearing 20-30 mmHg compression socks, and cutting sodium to under 2,000mg per day can significantly reduce swelling. Daily weight tracking helps spot fluid retention early. But if swelling persists despite these steps, talk to your doctor about alternatives.
Should I be worried if I’m on multiple medications?
Yes. Taking more than one drug that causes fluid retention - like amlodipine plus pioglitazone - greatly increases your risk. The American Geriatrics Society lists amlodipine, gabapentin, and pioglitazone as potentially inappropriate for older adults because of high edema risk. If you’re over 65 and on multiple meds, ask your doctor to review your list for overlapping side effects.
How long does it take for swelling to go away after stopping the medication?
It varies. Swelling from amlodipine often improves within 1-2 weeks after switching to another blood pressure drug. Gabapentin-related swelling may take up to 3-4 weeks to fully resolve. If swelling doesn’t improve after 2-3 weeks of stopping the drug, it’s likely caused by something else - like heart or kidney disease - and needs further testing.
Is it safe to take diuretics (water pills) for medication-induced swelling?
Not without medical supervision. Diuretics can help temporarily, but they don’t fix the root cause. They can also cause electrolyte imbalances, especially in older adults or those with kidney issues. If your doctor recommends a diuretic, it should be part of a broader plan - not a quick fix.
Can lifestyle changes help prevent medication swelling?
Absolutely. Reducing sodium, staying active (but avoiding long periods of standing), maintaining a healthy weight, and wearing compression socks can all help. Avoiding alcohol and managing stress also support better fluid balance. Prevention is easier than reversing swelling once it’s advanced.

Sheila Garfield - 30 January 2026
Been on amlodipine for 2 years and my ankles look like inflated balloons by bedtime. Compression socks saved my sanity. Not glamorous, but I’ll take ugly socks over ER visits any day.
Shawn Peck - 31 January 2026
Stop being dramatic. Swelling? Just drink more water and move your legs. Everyone’s got edema these days because they sit on their butts all day. It’s not the meds, it’s laziness.
April Allen - 2 February 2026
Medication-induced edema is a pharmacokinetic artifact of vascular permeability modulation - often mediated by nitric oxide pathways or sodium retention via aldosterone antagonism. The real issue isn’t the drug per se, but the lack of baseline biomarker monitoring. We need routine BNP, creatinine, and albumin checks before initiating high-risk agents like TZDs or CCBs. Otherwise, we’re just guessing.
And yes, this is why I’m still mad my PCP didn’t order a renal ultrasound when I started pioglitazone. Two months later, my eGFR dropped 28%. Coincidence? I think not.
Diana Dougan - 2 February 2026
So you’re telling me ibuprofen gives me puffy feet? No way. I’ve been taking 800mg daily since 2017 and my feet look fine. You just fat. And also, you probably eat too much bread. Gluten = water retention. #Truth
Melissa Cogswell - 4 February 2026
Just wanted to add - if you’re on gabapentin and notice swelling, try lowering the dose before switching. I cut mine from 900mg to 600mg and the puffiness faded over 10 days. No need to panic or ditch the med entirely. Talk to your neurologist about titration.
Kathleen Riley - 4 February 2026
One cannot help but observe the profound epistemological dissonance inherent in the contemporary medical paradigm, wherein pharmacological side effects are prematurely naturalized as benign, thereby obfuscating the deeper ontological crisis of iatrogenic harm. The body, in its sovereign wisdom, communicates through edema - yet the clinical gaze remains stubbornly reductive.
Perhaps we ought to consider not merely which drugs cause swelling, but why our epistemic frameworks refuse to listen to the body’s semiotics.
Beth Cooper - 4 February 2026
Let me guess - Big Pharma paid your doctor to keep you on that drug. They’ve been hiding the truth about edema since the 80s. The FDA? A puppet. Your ‘compression socks’? A distraction. The real solution is magnesium citrate and a Faraday cage to block the 5G signals that cause fluid retention. I’ve been researching this for 11 years. You’re welcome.
Holly Robin - 5 February 2026
So you’re telling me people are dying because their doctor didn’t check their kidneys? Shocking. But wait - didn’t the same people who said ‘it’s just a side effect’ also say smoking was harmless? And that vaccines cause autism? This is the same system that gave us Vioxx. I’m not surprised. The medical industrial complex is a death cult.
And FYI - you don’t need a doctor to tell you to stop a drug. You just need to be brave enough to say NO. I stopped my blood pressure med cold turkey. My swelling went away. My blood pressure? Still fine. The system doesn’t want you to know you have power.
Sarah Blevins - 6 February 2026
Analysis of the data presented indicates a moderate correlation between medication class and incidence of edema (r = 0.78, p < 0.01). However, the absence of control variables - including BMI, renal function, and concomitant medication use - limits causal inference. Furthermore, anecdotal reports from Reddit and HealthUnlocked constitute selection bias and should not be conflated with population-level epidemiology.
While lifestyle interventions are reasonable adjuncts, the recommendation to ‘talk to your doctor’ remains the only evidence-based course of action. The rest is noise.
Yanaton Whittaker - 7 February 2026
AMERICA! WE DON’T SWELL. WE STAND TALL. If your ankles are puffy, you’re probably eating Mexican food and watching Netflix. Get off the couch. Do push-ups. Drink less soda. And stop blaming your meds - blame the weak American lifestyle. #MakeEdemaGreatAgain