For decades, leukemia and lymphoma were treated the same way: harsh chemotherapy that attacked fast-growing cells-cancerous or not. Patients lost hair, got sick from nausea, and often faced relapse with few options left. Today, that’s changing. Targeted therapy and CAR T-cell therapy are no longer experimental. They’re standard care for many patients, offering deeper remissions, fewer side effects, and sometimes, a real chance at cure.
How Targeted Therapies Work
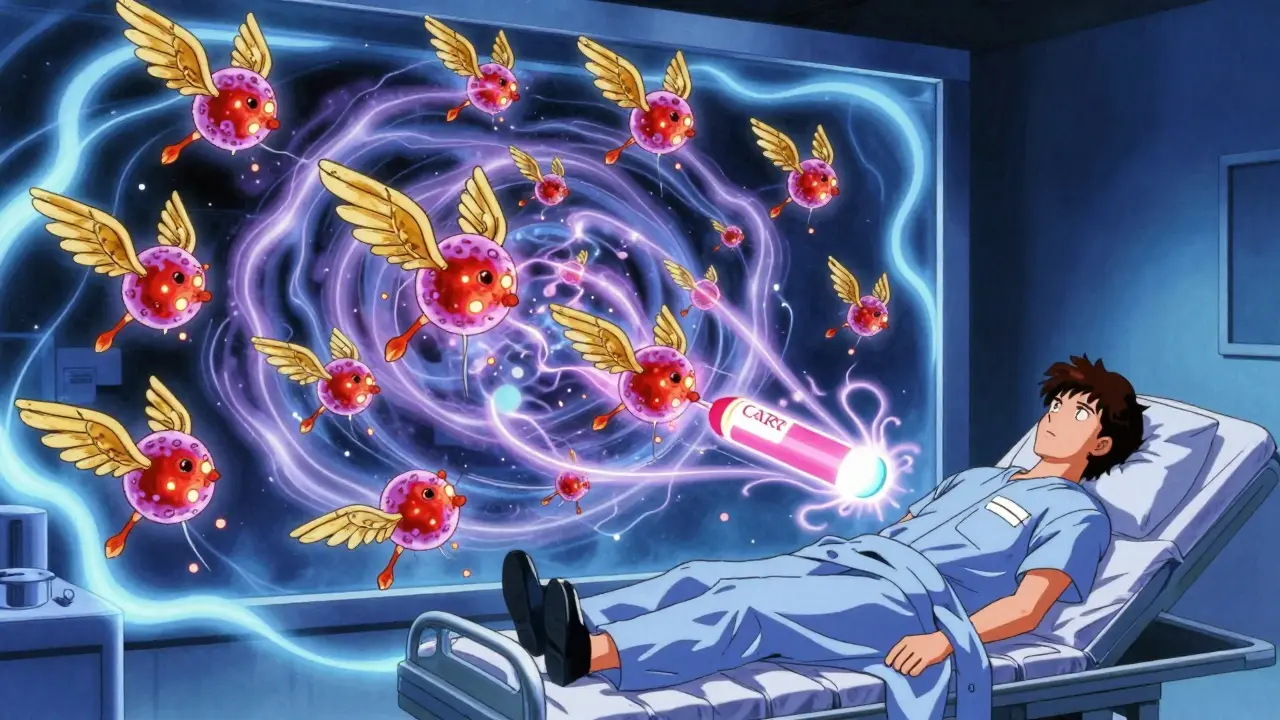
Targeted therapies don’t blast through the body like chemotherapy. They’re like smart missiles. They lock onto specific proteins or signals that cancer cells rely on to grow and survive. In leukemia and lymphoma, these signals often come from overactive kinases or anti-death proteins inside B-cells. Take ibrutinib (Imbruvica). It blocks Bruton’s tyrosine kinase (BTK), a protein that tells B-cells to keep multiplying. In chronic lymphocytic leukemia (CLL) and mantle cell lymphoma, stopping BTK slows the cancer down. Patients take one pill a day-420 mg-and most can keep working, traveling, even exercising. No hospital stays. No IV lines. Then there’s venetoclax (Venclexta). It targets BCL-2, a protein that acts like a shield, keeping cancer cells alive even when they should die. Venetoclax removes that shield. But it’s not simple. Because it triggers massive cancer cell death, patients start with a low dose and slowly ramp up over five weeks. That’s to avoid tumor lysis syndrome-a dangerous flood of toxins from dying cells. Many need to be hospitalized during this phase. These drugs changed everything for CLL. Before targeted therapies, patients with high-risk mutations like del(17p) or TP53 had survival times under a year. Now, many live five, seven, even ten years. The CLL Society found that the time between starting treatment and a dangerous transformation called Richter’s syndrome jumped from 2.2 years to 4.9 years with targeted drugs. That’s not just longer life-it’s better quality life.CAR T-Cell Therapy: Rewiring the Immune System
If targeted therapies are smart bullets, CAR T-cell therapy is a living drug. It takes your own immune cells-T-cells-and turns them into cancer hunters. Here’s how it works: First, doctors collect your blood through a process called leukapheresis. Then, in a lab, your T-cells are genetically modified to carry a special receptor-chimeric antigen receptor (CAR)-that lets them recognize CD19, a protein found on most B-cell lymphomas and leukemias. These engineered cells are multiplied in the lab, sometimes into the billions. Then they’re infused back into you. The result? A living army inside your body that keeps hunting cancer cells, sometimes for years. The first FDA-approved CAR T-cell therapy, tisagenlecleucel (Kymriah), was approved in 2017 for kids with relapsed acute lymphoblastic leukemia. Since then, others like axicabtagene ciloleucel (Yescarta) and lisocabtagene maraleucel (Breyanzi) have followed. In relapsed or refractory large B-cell lymphoma, Yescarta showed a 42.6% four-year survival rate in the ZUMA-7 trial-far better than the old salvage chemo options. Even more exciting? Newer versions are coming. Gilead’s KITE-363 and KITE-753 target not just CD19, but CD20 too. Why? Because some cancers escape by losing CD19. Hitting two targets at once makes it harder for the cancer to hide. Early data from June 2025 showed a 63.6% complete remission rate in patients who had failed other treatments.Why These Therapies Are Better-But Not Perfect
Compared to chemo, targeted and cellular therapies offer clear advantages:- Less toxicity: No more days spent vomiting or too weak to get out of bed. Many patients on ibrutinib or venetoclax report near-normal daily lives.
- Higher response rates: In relapsed mantle cell lymphoma, one CAR T-cell therapy (LV20.19) achieved a 100% overall response rate and 88% complete remission in a 2025 trial.
- Potential for cure: For patients who’ve exhausted all other options, CAR T-cell therapy can lead to long-term remission-or even cure.
Cost, Access, and the Real-World Hurdles
These therapies are expensive. A single CAR T-cell treatment can cost $373,000 to $475,000. Even targeted pills like ibrutinib or venetoclax can run $15,000-$25,000 per month out-of-pocket. Insurance helps, but not always enough. Access is another issue. CAR T-cell therapy requires a certified center with ICU capability, specialized staff, and months of training to set up. Only 89% of NCI-designated cancer centers offer it. In community hospitals? Just 32%. That means patients in rural areas often must travel hundreds of miles, take time off work, and find housing near a major city. Manufacturing also takes time. From blood draw to infusion, it’s 3-5 weeks. For someone with aggressive lymphoma, that delay can be deadly. Newer “off-the-shelf” CAR T-cells are in trials, but none are approved yet.Who Benefits Most?
Not everyone needs these therapies. For early-stage CLL, watchful waiting is still standard. For younger, fit patients with relapsed disease, CAR T-cell therapy is often the best shot. For older patients with comorbidities, targeted oral drugs might be safer. Doctors now use genetic testing to decide. If you have a TP53 mutation, targeted therapy is preferred over chemo. If you’ve had two or more relapses, CAR T-cell therapy is often the next step. In mantle cell lymphoma, CAR T-cells are now used after first relapse-not as a last resort. The future? Earlier use. A 2025 ASCO survey found 68% of hematologists believe CAR T-cell therapy will become first-line treatment for high-risk lymphomas by 2030. Imagine skipping chemotherapy entirely and going straight to a one-time infusion that might cure you.
What’s Next?
The pipeline is full. New drugs are targeting different proteins: BCL-XL, PI3K, SYK. Bispecific antibodies-like teclistamab-bind T-cells directly to cancer cells without needing genetic modification. They’re given as injections, not infusions, and are already approved for multiple myeloma. Trials for lymphoma are underway. Researchers are also working on ways to reduce side effects. New CAR designs are being tested to lower CRS risk. Some are even being built to self-destruct if they become too active. And while cost remains a barrier, value-based pricing models are being discussed. If a therapy gives you 10 years of life instead of 2, is $400,000 too much? That’s the question oncologists are now facing.Real Stories, Real Outcomes
One patient in Perth, diagnosed with relapsed follicular lymphoma after two rounds of chemo, received Yescarta in late 2024. Six months later, his scans were clear. No more fatigue. No more monthly infusions. He’s back to gardening. Another, a 68-year-old with CLL and del(17p), started on venetoclax plus obinutuzumab. After 12 months, his cancer was undetectable. He’s off treatment and feeling better than he has in a decade. But not all stories end well. Some patients develop resistance to both BTK and BCL-2 inhibitors. For them, options are still limited. That’s why research continues.What You Need to Know
If you or someone you know has leukemia or lymphoma:- Ask about genetic testing. Mutations matter.
- Ask if targeted therapy is an option. Oral drugs can be life-changing.
- If you’ve relapsed, ask about CAR T-cell therapy-even if you’re older or have other health issues. Eligibility is broader than you think.
- Find a center with experience. Not every hospital can safely deliver these treatments.
- Know the costs. Ask about financial aid, manufacturer support programs, and insurance appeals.
What is the difference between targeted therapy and CAR T-cell therapy?
Targeted therapy uses drugs that block specific proteins cancer cells need to grow-like ibrutinib or venetoclax. These are taken as pills. CAR T-cell therapy is a personalized treatment where your own immune cells are removed, genetically changed to attack cancer, and then reinfused. It’s a one-time infusion, but requires hospitalization and carries risks like cytokine release syndrome.
Are targeted therapies better than chemotherapy?
For many patients, yes. Targeted therapies often cause fewer side effects like nausea, hair loss, or low blood counts. They also work better in patients with high-risk genetic mutations. Studies show longer progression-free survival and better quality of life compared to traditional chemo-immunotherapy.
How long does CAR T-cell therapy take to work?
It takes 3-5 weeks to manufacture the cells after your blood is collected. After infusion, responses can be seen within days or weeks. Some patients show dramatic improvement in just 10-14 days. But full remission can take up to 3 months. Monitoring continues for months to years to track durability.
Can CAR T-cell therapy cure leukemia or lymphoma?
For some patients, yes. In relapsed or refractory cases where other treatments failed, CAR T-cell therapy has led to long-term remission-or cure-in a significant number. For example, in certain lymphomas, nearly half of patients treated with Yescarta are alive and disease-free at four years. But it’s not guaranteed. Some cancers return, and research is ongoing to improve long-term results.
What are the side effects of CAR T-cell therapy?
The two main risks are cytokine release syndrome (CRS) and neurotoxicity. CRS causes high fever, low blood pressure, and trouble breathing. Neurotoxicity can lead to confusion, seizures, or trouble speaking. Both are serious but treatable if caught early. Most patients are monitored in the hospital for at least a week after infusion. Long-term side effects can include low antibody levels, requiring IVIG infusions.
Is CAR T-cell therapy available everywhere?
No. It requires specialized centers with ICU capabilities, trained staff, and experience managing toxicities. Only about 89% of major cancer centers in the U.S. offer it. In Australia and other countries, access is even more limited. Patients often need to travel to major cities for treatment. Community hospitals rarely have the infrastructure.
How much does CAR T-cell therapy cost?
The treatment itself costs between $373,000 and $475,000 in the U.S. In Australia, Medicare covers most of it, but patients may still face out-of-pocket costs for travel, accommodation, and medications. Some manufacturers offer patient assistance programs. The total cost includes hospitalization, monitoring, and managing side effects-often adding tens of thousands more.
What happens if targeted therapy stops working?
If resistance develops, doctors may switch to another targeted drug, combine therapies, or move to CAR T-cell therapy. For patients who fail both BTK and BCL-2 inhibitors, options are limited-but clinical trials are exploring new drugs like next-generation BTK inhibitors, bispecific antibodies, or combination cellular therapies. Clinical trials are often the best next step.



Ryan Riesterer - 22 January 2026
Targeted therapies represent a paradigm shift in hematologic oncology. The pharmacokinetic profiles of BTK inhibitors like ibrutinib demonstrate sustained occupancy kinetics, leading to durable suppression of BCR signaling. Venetoclax’s BH3-mimetic mechanism induces apoptosis via BCL-2 displacement, but tumor lysis syndrome remains a non-trivial risk requiring prophylactic hydration and uric acid control. The clinical utility of these agents is well-documented in NCCN guidelines for CLL and MCL.
Akriti Jain - 23 January 2026
So let me get this straight 🤔 Big Pharma invented ‘smart missiles’ so they can charge $400K for a one-time infusion and call it ‘cure’? 🤡 Meanwhile, my cousin’s chemo was covered by Medicaid and he’s alive 7 years later. Coincidence? Or just another capitalist fairy tale? 💸💉 #CancerIndustry
Liberty C - 24 January 2026
How utterly pedestrian. You speak of ‘targeted therapy’ as if it’s some miraculous breakthrough, yet you fail to contextualize the sheer arrogance of medical elitism - these treatments are accessible only to those with the right insurance, the right zip code, the right pedigree. The fact that you celebrate this as progress reveals your detachment from the reality that medicine has become a luxury good. If your ‘cure’ requires a six-figure payment and a pilgrimage to a coastal academic center, it’s not medicine - it’s performance art for the privileged.
Hilary Miller - 25 January 2026
My dad got CAR T in ’23. No chemo. No hospital stays after infusion. Just tired for a week. Now he’s hiking again. Life-changing.
Margaret Khaemba - 26 January 2026
This is so fascinating! I’ve been reading up on bispecific antibodies too - like teclistamab - and it’s wild how they’re kind of like a bridge between targeted drugs and CAR T. No genetic engineering needed, just an injection. I wonder if they’ll eventually replace CAR T for some patients? Also, the cost issue is insane… I read that some hospitals are starting payment plans. Has anyone here used manufacturer assistance programs?
Malik Ronquillo - 27 January 2026
Man I used to work in oncology and let me tell you this whole targeted therapy thing is just a money grab. They keep tweaking the same damn proteins and calling it innovation. Half these patients are just trading one set of side effects for another. And don't get me started on the cost. My uncle paid $20K a month and still ended up in hospice. They're selling hope like it's a subscription box.
Alec Amiri - 29 January 2026
Let’s be real - if you’re not rich or in a major city, this stuff is just a fantasy. My cousin in rural Kansas had to drive 6 hours just to get evaluated for CAR T. They told her she wasn’t ‘a good candidate’ because she had high blood pressure. Meanwhile, the guy in the next state got it because he ‘had good insurance.’ This isn’t medicine. It’s a lottery.
Lana Kabulova - 29 January 2026
Wait - you mention ‘off-the-shelf’ CAR T in trials? That’s huge. But why is no one talking about the manufacturing bottleneck? The 3–5 week window? For aggressive lymphomas, that’s an eternity. And you say ‘only 89% of NCI centers offer it’ - but what about the other 11%? Are those patients just abandoned? Also - how many of these ‘complete remissions’ are actually durable? 42% at 4 years? That’s not a cure. That’s a pause.
Mike P - 30 January 2026
Yeah right, 'targeted therapy' - sounds fancy but it's just another way for the U.S. to charge the world for science we didn't even invent. Germany and Japan had similar drugs years ago. Now they're making them cheaper. Meanwhile we're out here charging $400K like we're selling rocket fuel. And don't even get me started on how we treat patients like test subjects instead of people. This isn't progress - it's exploitation.
Keith Helm - 1 February 2026
It is imperative to note that the administration of CAR T-cell therapy necessitates a multidisciplinary team, including hematologists, intensivists, pharmacists, and specialized nursing staff. The infrastructure required is non-trivial, and the standard of care must adhere strictly to ASH and EBMT guidelines to mitigate cytokine release syndrome and immune effector cell-associated neurotoxicity syndrome. Without such protocols, outcomes deteriorate significantly.
Daphne Mallari - Tolentino - 1 February 2026
One cannot help but observe the dissonance between the clinical triumphs described and the socioeconomic reality of their delivery. The commodification of cellular therapeutics, while scientifically laudable, reflects a systemic failure of healthcare equity. The rhetoric of ‘cure’ obscures the fact that access is contingent upon wealth, geography, and institutional affiliation - not medical need. This is not innovation. It is exclusion dressed in white coats.
Chiraghuddin Qureshi - 2 February 2026
My brother in Delhi got ibrutinib through a patient access program - cost was $200/month. He’s been on it for 4 years. No side effects. Still teaching school. The real story isn’t the tech - it’s how the world works. In the U.S., they charge $25K. In India, they make it affordable. Science is global. Profit? Not so much. 🌍❤️