Rare Adverse Event Detection Calculator
How Many Records Do You Need?
Calculate how many claims records or registry records are needed to reliably detect rare adverse drug events based on event frequency.
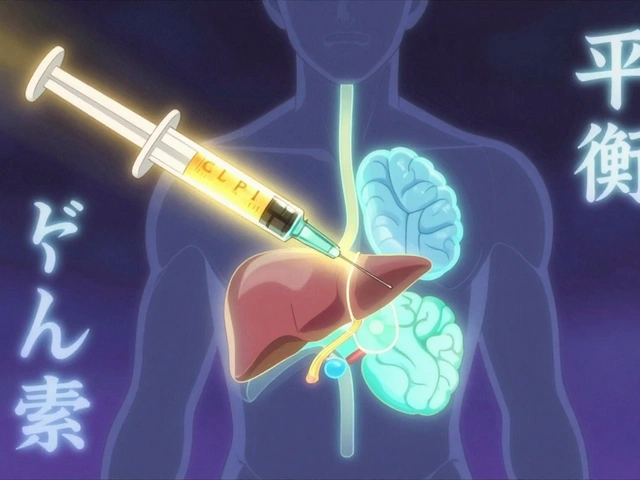
The FDA states: "Detecting a rare adverse event (1 in 10,000) requires 1 million claims records—but only 500,000 registry records."
Why the Difference?
Registries capture detailed clinical information (lab results, symptoms, treatment history) while claims data focuses on billing codes and medication fills. This allows registries to detect rare events with 50% fewer records because:
- Registries have cleaner data (fewer coding errors)
- Registries include clinical context (lab values, symptoms)
- Registries are more complete (80% data completeness vs 45-60% in claims)
The FDA found that combining both data sources reduces false alarms by 40% while maintaining detection power.
When a new drug hits the market, the real test of its safety doesn’t happen in a clinical trial. It happens in the real world-among millions of people with different health conditions, lifestyles, and genetics. That’s where real-world evidence comes in. Two of the most powerful tools for tracking drug safety after approval are patient registries and claims data. Together, they give regulators, doctors, and pharmaceutical companies a clearer picture of what’s really happening when drugs are used outside controlled studies.
What Is Real-World Evidence, Really?
Real-world evidence (RWE) isn’t guesswork. It’s data pulled from everyday healthcare systems-things like hospital billing records, insurance claims, disease registries, and electronic health records. The U.S. Food and Drug Administration (FDA) officially defined RWE in 2018 as clinical evidence derived from analyzing real-world data (RWD). Unlike clinical trials, which involve carefully selected patients under strict conditions, RWE captures how drugs behave in messy, real-life settings. This matters because rare side effects, interactions with other medications, or long-term impacts often don’t show up in trials that last only months or include a few thousand people.Registries: The Deep Dive into Patient Stories
Patient registries are structured databases that collect detailed, standardized information about people with specific diseases or those using particular drugs. Think of them as long-term medical diaries, but on a national or even global scale. Disease registries, like the SEER cancer registry in the U.S., track hundreds of thousands of patients over years. They record not just diagnosis codes, but lab results, imaging reports, treatment changes, and even how patients feel day to day. Product registries focus on patients using a specific drug-tracking everything from dosage adjustments to unexpected reactions. Why are they valuable? Because they capture clinical depth. A 2021 study showed registries offer 37.2% more detail on long-term outcomes than claims data alone. For example, the Cystic Fibrosis Foundation Patient Registry helped identify that ivacaftor, a drug for cystic fibrosis, worked exceptionally well in patients with certain genetic mutations-something clinical trials missed because those mutations were too rare to be included in sufficient numbers. But registries aren’t perfect. They’re expensive. Setting one up can cost $1.2 to $2.5 million and take 18 to 24 months. Maintenance runs $300,000 to $600,000 a year. Participation rates are often only 60-80%, meaning the data might not represent everyone. And nearly one-third of academic registries shut down within five years due to funding gaps.Claims Data: The Broad View of Healthcare Use
Claims data is what insurance companies and government programs like Medicare collect every time a patient visits a doctor, gets a prescription filled, or is admitted to a hospital. It includes ICD-10 diagnosis codes, CPT procedure codes, and NDC medication identifiers. It doesn’t tell you what a patient’s blood pressure was, but it tells you how often they went to the ER, what drugs they got, and whether they were hospitalized. The power of claims data is scale. IBM MarketScan covers 200 million lives. Optum has 100 million. Medicare claims alone span over 60 million people and can track the same patient for 15+ years. That’s more than enough to spot rare side effects-like a 1 in 10,000 risk of liver damage-that would never show up in a trial of 5,000 patients. The FDA has used claims data for decades. In 2015, they analyzed 1.2 million Medicare records to check if entacapone (used for Parkinson’s) increased heart risks. They found no link. In 2014, they reviewed 850,000 records to assess olmesartan (a blood pressure drug) for gastrointestinal issues in diabetics. The data helped shape safety labeling. But claims data has blind spots. It’s missing clinical details. Only 45-60% of lab values are recorded. Patient-reported symptoms like fatigue or dizziness? Rarely captured. Coding errors are common-up to 20% of diagnosis codes are wrong, according to the Agency for Healthcare Research and Quality (AHRQ). And it can’t explain why a patient stopped taking a drug-was it side effects? Cost? Or just forgetting?
Registries vs. Claims Data: When to Use Which
Here’s the practical difference:- Use registries when you need deep clinical insight: rare diseases, complex outcomes, genetic subgroups, or patient-reported symptoms.
- Use claims data when you need broad population coverage: detecting rare events, tracking long-term use, comparing drug safety across large groups, or monitoring usage patterns.
Hybrid Approaches Are the Future
The smartest moves now combine both. The International Council for Harmonisation (ICH) E2 proposal from June 2023 recommends using registries and claims data together. Why? Because when you cross-check signals, false alarms drop by 40%. Here’s how it works: Claims data flags a possible link between a drug and a spike in liver enzyme levels. Registries then pull in lab results, doctor notes, and patient histories to confirm whether it’s a real safety signal or just a coding error or unrelated condition. This hybrid approach is now standard in top pharmacovigilance programs. Novartis started blending claims data with wearable device readings (like heart rate and activity levels) in 2023 to monitor Entresto patients for heart failure worsening. AI tools now help analyze these combined datasets, cutting false positives by 28%, according to a 2024 JAMA Network Open study.Regulatory Acceptance Is Growing Fast
The FDA approved 12 drugs or new indications between 2017 and 2021 using RWE from registries or claims data. Five of those relied directly on registry or claims data. The EMA’s Darwin EU network, launched in 2021, now connects 32 databases across 15 countries, covering 120 million patients. The FDA’s 2022 guidance says claims data analyses must correct for “immortal time bias”-a statistical error where patients who survive longer are unfairly counted as safer. Proper methods reduce this bias by 35-50%. In January 2024, the FDA released draft rules requiring registries to maintain at least 80% data completeness on key variables to be accepted for regulatory use. Meanwhile, pharmaceutical companies are investing more. In 2017, only 3-5% of pharmacovigilance budgets went to RWE. By 2023, that jumped to 8-12%. Oncology leads with 38% of RWE submissions using registries. Cardiovascular drugs? 45% use claims data-the highest of any therapeutic area.
Challenges That Still Exist
Despite progress, big hurdles remain:- Data standardization: Getting different systems to talk to each other takes up to 60% of project time.
- Privacy rules: HIPAA in the U.S., GDPR in Europe-compliance is complex and costly.
- Expertise gap: Few data scientists know both healthcare coding systems and statistical methods for observational data.
- Selection bias: People who join registries are often more engaged or healthier than average.
- Funding instability: Academic registries die without steady funding. Industry-funded ones may be biased toward positive results.
What’s Next?
The FDA’s REAL program, launched in 2023, aims to standardize registry data collection for 20 priority diseases by 2026-with a focus on rare diseases. Meanwhile, AI-driven signal detection tools are becoming faster and more accurate. Wearables, genomics, and social determinants of health are being added to the mix. The bottom line? Registries and claims data are no longer backup tools. They’re central to modern drug safety. Regulators expect them. Companies are building them. And patients benefit when side effects are caught early-before they become widespread.For anyone tracking drug safety today, ignoring these sources isn’t just outdated-it’s risky.
What’s the difference between claims data and patient registries?
Claims data comes from insurance billing records and includes diagnosis codes, procedures, and medication fills-it’s broad but shallow. Patient registries are curated databases that collect detailed clinical information like lab results, imaging, and patient-reported symptoms-they’re deep but cover smaller groups. Claims data tells you what happened; registries tell you why and how.
Can claims data detect rare side effects?
Yes, but only if the database is large enough. For a side effect affecting 1 in 10,000 patients, you need about 1 million claims records to spot it reliably. Registries can detect the same signal with half as many records because their data is cleaner and more complete. Claims data is great for scale; registries are better for precision.
Why do regulators trust real-world evidence now?
Because it’s been validated. The FDA has used RWE to approve 12 drugs or new uses since 2017. Studies show well-designed registry and claims data can match the reliability of randomized trials for certain safety questions. The 21st Century Cures Act and EMA’s Darwin EU program formalized this shift. It’s no longer experimental-it’s expected.
Are there risks in using claims data for drug safety?
Yes. Up to 20% of diagnosis codes are inaccurate. Claims data lacks clinical context-like whether a patient had a pre-existing condition or took other drugs. It can’t explain why a patient stopped treatment. This leads to false alarms: one study found 22% of initial safety signals from claims data turned out to be unrelated after clinical review. That’s why experts recommend combining it with registry data.
How are companies using RWE today?
Pharmaceutical companies now spend 8-12% of their pharmacovigilance budgets on RWE, up from 3-5% in 2017. They use it to support label expansions, monitor long-term safety, and respond to regulatory requests. Oncology and cardiovascular drugs lead in RWE use. Some are even blending claims data with wearable device readings and AI tools to catch subtle safety signals faster.
Is real-world evidence replacing clinical trials?
No. Clinical trials are still the gold standard for proving a drug works. But RWE fills the gaps after approval-tracking long-term safety, rare side effects, and real-world effectiveness. The future isn’t either/or. It’s using trials to prove benefit, and RWE to confirm safety over time and across diverse populations.
Where This Is Headed
By 2026, the FDA plans to have standardized registry data collection for 20 priority diseases. The EMA’s Darwin EU will keep expanding. AI will get better at spotting patterns. Wearables and genomics will add layers of detail. The goal? A global, real-time safety net for medicines-one that catches problems before they hurt thousands.For patients, that means safer drugs. For doctors, better guidance. For the system, smarter spending. Real-world evidence isn’t the future of drug safety-it’s already here.




Jessie Ann Lambrecht - 8 January 2026
Love how this breaks down the real-world stuff without jargon overload. Registries are like the Netflix documentary version of drug safety-deep, personal, and full of nuance. Claims data? More like the Wikipedia summary: fast, broad, but missing the emotional beats. Together? Pure magic. I’ve seen a patient go from ‘mystery rash’ to ‘confirmed rare reaction’ because a registry had their lab notes from 2019. That’s not data-that’s saving lives.
And honestly? If your pharma company isn’t blending both, you’re flying blind with a parachute made of tissue paper.
Aparna karwande - 9 January 2026
How can you even trust Western data systems? In India, we have 1.4 billion people and zero proper registries, yet our doctors manage just fine with local knowledge. Claims data? Ha! Our insurance system is a joke-paper forms, handwritten codes, and 70% of patients pay out of pocket. You think your ‘1 million records’ matter when half the world doesn’t even have a digital footprint?
This isn’t science-it’s colonial data imperialism dressed up as innovation. We don’t need your fancy AI to tell us what works. We’ve been doing it for centuries.
Adam Gainski - 9 January 2026
Really appreciate the breakdown here. One thing I’d add-regardless of whether you’re using claims or registries, the biggest bottleneck isn’t the data, it’s the people. Too many teams still treat RWE like a black box. You need clinicians who understand coding, statisticians who know what ‘dizziness’ actually means in a patient’s note, and IT folks who can map ICD-10 to EHR fields without losing half the data.
It’s not about having more data. It’s about having smarter teams who can read between the lines. And that’s still rare.
Anastasia Novak - 10 January 2026
OMG I’m so over this ‘hybrid approach’ buzzword. It’s like saying ‘we use both a hammer and a screwdriver’ like that’s genius. Newsflash: if your safety signal needs a registry to ‘confirm’ what claims data flagged, you didn’t design your surveillance system-you built a Rube Goldberg machine out of spreadsheets.
And don’t even get me started on ‘AI cutting false positives by 28%.’ That’s just corporate fluff. The real 28%? The hours I wasted last month trying to convince my boss that ‘liver enzyme spike’ ≠ ‘drug toxicity’ when the patient was on 12 other meds and had hepatitis C.
Stop pretending tech fixes human chaos.
Elen Pihlap - 11 January 2026
but what if the registry just... stops working? like what if someone runs out of money and poof it’s gone? and then all those people’s data just disappears? and you have no idea what happened to them? like... what if someone died and you’ll never know because the registry shut down? i just think about that and it makes me so sad
Sai Ganesh - 13 January 2026
In India, we don’t have the luxury of million-record databases, but we do have something better: community trust. Our doctors know their patients by name, by family history, by which village they’re from. A patient comes in with a rash after starting a new drug? The doctor remembers they had a similar reaction last year to another med. No registry needed.
Western systems over-engineer because they’ve lost the human connection. We don’t need AI to tell us what a grandmother knows by instinct.
Paul Mason - 13 January 2026
Look, I’ve been doing this since the 90s. Back then, we used paper logs and fax machines. Now we’ve got AI and AI-powered AI. But guess what? The same mistakes still happen. Someone miskeys a code, someone forgets to update a med list, someone assumes ‘diabetes’ means Type 2 when it’s actually MODY.
Technology doesn’t fix dumb. It just makes dumb faster.
And don’t get me started on ‘FDA-approved’ RWE. That’s like saying your cousin’s TikTok diet plan is ‘clinically validated’ because it got 10K likes.
Katrina Morris - 14 January 2026
i love how this post explains things so clearly
registry data feels like listening to a patient’s whole story
claims data is like reading the hospital bill
both matter
but i just wish more people knew how fragile registries are
so many shut down and no one notices until someone gets hurt
steve rumsford - 16 January 2026
so like... if claims data is 20% wrong and registries cost millions and die after 5 years... why are we still pretending this is a perfect system?
it’s not. it’s a patchwork of half-dead databases and hopeful assumptions.
but hey at least we’re trying right?
also i just found out my cousin’s drug reaction was caught because of a registry that got funded by a nonprofit run by a guy who used to work at Pfizer
so... weird but true
Andrew N - 18 January 2026
Let’s be real. 8-12% of pharmacovigilance budgets? That’s still peanuts. Most companies treat RWE like a compliance checkbox, not a strategic asset. And the ‘AI cutting false positives’ claims? 90% of those models are trained on biased data from the same 3 big insurers. You’re not detecting safety signals-you’re reinforcing existing gaps.
Also, ‘1 in 10,000’ events? That’s not rare. That’s a national tragedy waiting to happen. We need systemic change, not better algorithms.
LALITA KUDIYA - 19 January 2026
i think both systems are good if we use them together
like a team
no need to fight
we just need more people to care
Poppy Newman - 19 January 2026
Okay but can we talk about how wild it is that we’re using insurance claims to track drug safety? Like... imagine if your Netflix watch history was used to diagnose your depression. That’s basically what’s happening here.
Also, why do we still use ICD-10 codes in 2024? We have voice assistants and smart fridges. Can’t we just ask patients, ‘Hey, did you feel weird after taking this?’ and record it? 🤔
Anthony Capunong - 20 January 2026
Let me stop you right there. You’re all talking like this is some neutral, objective science. Newsflash: registries are funded by pharma. Claims data is owned by insurance giants. The FDA? They’re staffed by ex-pharma execs.
This isn’t safety. It’s PR with a spreadsheet.
And don’t even get me started on ‘hybrid approaches’-that’s just a fancy way of saying ‘we’ll use your data to make our drug look better.’
Vince Nairn - 21 January 2026
So we spend millions to track a side effect that affects 1 in 10,000... but we can’t fix the 30% of Americans who can’t afford their meds?
Brilliant. Let’s use AI to detect liver damage while people skip doses because the copay is $500.
Real-world evidence? More like real-world irony.
Ayodeji Williams - 22 January 2026
yo this is all fine but what about africa? we got no registries no claims data no nothing
but we got people dying from drugs that never got tested here
so why are we all talking about 1 in 10k when 1 in 10 here is already dead?
why is this always about the west?
😂