Living with IBS-Mixed means your gut feels like a rollercoaster-some days you’re stuck on the toilet with hard, painful stools, and other days you’re racing to the bathroom with watery diarrhea. There’s no warning. No pattern. Just unpredictable, frustrating shifts that make planning a day out, going to work, or even sleeping through the night feel impossible. You’re not alone. About 1 in 5 people with IBS experience this back-and-forth, and it’s one of the hardest subtypes to manage because treating one symptom often makes the other worse.
What Exactly Is IBS-Mixed?
IBS-Mixed, or IBS-M, is a subtype of irritable bowel syndrome defined by the Rome IV criteria: you have abdominal pain at least once a week for the past three months, and your bowel habits alternate between constipation and diarrhea. To qualify, you need to have hard or lumpy stools (Bristol Stool Scale 1-2) and loose or watery stools (Bristol Stool Scale 6-7) in at least 25% of your bowel movements. That’s not just occasional changes-it’s a pattern that’s been going on for months, sometimes years.
Unlike Crohn’s disease or ulcerative colitis, IBS-M doesn’t show inflammation or damage on scans or biopsies. Instead, it’s about how your gut nerves and muscles behave. Your gut is overly sensitive, moves too fast or too slow, and your gut bacteria are out of balance. Stress and food can trigger flare-ups, but they don’t cause the condition-they just light the fuse.
Why Is IBS-Mixed So Hard to Treat?
Most IBS medications target one direction: either constipation or diarrhea. But IBS-Mixed? It goes both ways. Take loperamide (Imodium)-it stops diarrhea, but if you take it on a constipation day, you’ll be stuck. Laxatives like polyethylene glycol help with hard stools, but if you use them during a diarrhea phase, you’ll make things worse. It’s a constant balancing act.
Studies show that drugs designed for IBS-Constipation (like linaclotide) or IBS-Diarrhea (like eluxadoline) only help about 20% of IBS-M patients. That’s because these drugs don’t account for the switching nature of your symptoms. The same goes for over-the-counter remedies. Many people try peppermint oil capsules or fiber supplements, but without a plan, they’re just guessing.
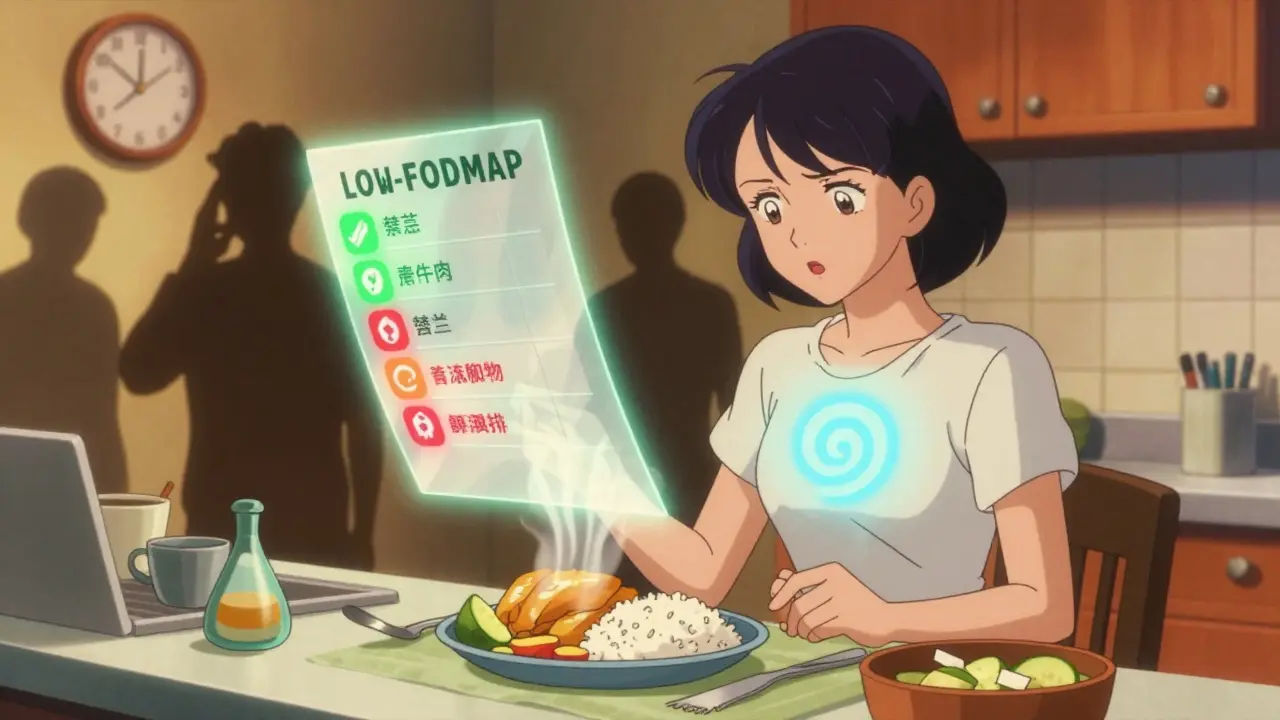
The Low FODMAP Diet: Your Best Shot at Stability
If you’ve tried everything and nothing sticks, the low FODMAP diet is the most evidence-backed tool you’ve got. It’s not a weight-loss plan. It’s a diagnostic tool. FODMAPs are short-chain carbs that ferment in your gut and pull water in, causing bloating, gas, and erratic bowel movements. Common triggers include onions, garlic, wheat, dairy, apples, and artificial sweeteners like sorbitol.
A 2021 study in Gastroenterology found that 50-60% of IBS-M patients saw symptom improvement on the low FODMAP diet. That’s lower than the 70-75% seen in IBS-D, but still better than most medications. The key? You don’t stay on the strict version forever. You eliminate high-FODMAP foods for 2-6 weeks, then slowly reintroduce them one at a time to find your personal triggers.
Most people notice a difference within 4-6 weeks. One user on Reddit shared: “After three months on low FODMAP and daily peppermint oil, I went from 25 symptom days a month to 8.” That’s life-changing. But don’t try this alone. Work with a dietitian who knows IBS. Messing up the reintroduction phase can make you more sensitive than before.
Medications That Actually Work for IBS-Mixed
There’s no magic pill for IBS-M, but some medications help more than others. Antispasmodics like dicyclomine (10-20mg as needed) relax gut muscles and reduce cramping. They work equally well for constipation and diarrhea phases, and many people find them useful for sudden pain flare-ups.
Antidepressants are another surprise winner. Low-dose tricyclics like amitriptyline (10-25mg at night) don’t treat depression-they calm overactive gut nerves. A 2021 Cochrane review found they improved pain and overall symptoms in 55-60% of IBS-M patients, better than any other drug class. SSRIs like sertraline help too, but tricyclics are more effective for pain.
For acute symptoms, keep two tools handy: one for diarrhea (loperamide, 2-4mg as needed) and one for constipation (polyethylene glycol 17g daily, or magnesium citrate 200-400mg). Don’t take them daily. Only use them when your symptoms shift. This is called “symptom-triggered therapy,” and it’s the most effective way to avoid making things worse.
Stress, Anxiety, and Your Gut
More than half of IBS-M patients say stress makes their symptoms worse. It’s not “all in your head”-it’s science. Your gut and brain are connected by the vagus nerve. When you’re stressed, your gut slows down or speeds up. That’s why panic before a meeting can trigger diarrhea, or prolonged anxiety can lead to constipation.
Cognitive Behavioral Therapy (CBT) is now a strong recommendation from the American Gastroenterological Association. It’s not talk therapy to fix your life-it’s practical training to change how you respond to gut sensations. A 2021 study showed CBT reduced IBS symptom scores by 40-50%, compared to just 15-20% with basic education. Apps like Cara Care and The IBS Clinic offer guided CBT programs you can do at home.
Other stress-reduction tools like diaphragmatic breathing, yoga, or even 20 minutes of daily walking can lower your overall sensitivity. You don’t need to meditate for an hour. Just 5 minutes of slow breathing before bed can help your gut reset overnight.
What Doesn’t Work (And Why You Should Stop Trying It)
Many people waste months on things that don’t help-or make things worse. Here’s what to avoid:
- Long-term laxatives: They train your gut to rely on them. You’ll need higher doses over time, and when you stop, constipation returns worse.
- Probiotics without strain specificity: Not all probiotics are equal. The strain Bifidobacterium infantis 35624 has been shown to help IBS-M, but generic brands like Culturelle or Align often do nothing.
- Eliminating entire food groups: Cutting out gluten or dairy without testing for sensitivity can lead to nutrient deficiencies and unnecessary restrictions.
- Overusing fiber supplements: Insoluble fiber (like wheat bran) can worsen bloating and gas. Stick to soluble fiber like psyllium husk (5g daily), which gently regulates both constipation and diarrhea.
Tracking Your Symptoms: The Key to Control
Without tracking, you’re flying blind. You might think dairy triggers you-but what if it’s the onion in your sauce, or the artificial sweetener in your protein bar? A symptom diary is non-negotiable.
Track for at least four weeks: record bowel movements (use the Bristol Stool Scale), pain level (0-10), food eaten, stress level, and sleep quality. Use an app like Cara Care or IBS Buddy-they auto-calculate patterns and flag triggers. One 2022 study found people using apps improved 35% more than those using paper logs.
Look for patterns: Do symptoms spike after coffee? After sleepless nights? After eating out? Once you spot them, you can plan around them.
What’s Coming Next for IBS-Mixed?
The future looks promising. In 2023, the FDA approved a new drug called ibodutant, which targets nerve signals in the gut. In phase 3 trials, it improved symptoms in 45% of IBS-M patients-nearly double the placebo rate. It’s not available yet, but it’s a sign that researchers are finally focusing on IBS-M specifically.
Microbiome testing is also getting smarter. Companies like Viome use AI to analyze your gut bacteria and suggest personalized diets. In a 2023 pilot study, users saw 58% symptom improvement. It’s expensive now, but it’s the direction medicine is heading: no more guesswork, just precision.
The Rome V criteria, expected in 2024, will raise the bar for diagnosis: instead of alternating symptoms in 25% of bowel movements, you’ll need to see them in 30%. That means fewer people will be misdiagnosed, and better treatments will follow.
Real-Life Management: A Simple Routine
Here’s what works for people who’ve finally found control:
- Start with the low FODMAP elimination phase for 4-6 weeks (with a dietitian).
- Take 5g of psyllium husk daily-mixed in water or smoothies-to keep things regular.
- Keep loperamide and polyethylene glycol on hand-use only when needed.
- Take a low-dose tricyclic antidepressant (like amitriptyline) at night if pain is frequent.
- Use enteric-coated peppermint oil (IBgard) 2x daily to reduce cramping and bloating.
- Practice 5 minutes of deep breathing before bed every night.
- Track everything in an app for at least 3 months.
It takes 3-6 months to get good at this. Don’t expect overnight results. But if you stick with it, most people see a 50-70% reduction in symptoms. You won’t be “cured,” but you’ll be in control.
When to See a Doctor
Before assuming it’s IBS-Mixed, rule out other conditions. Get tested for celiac disease, thyroid issues, and inflammatory bowel disease. A simple blood test (CBC, CRP, tTG-IgA) can rule out serious problems. If you have weight loss, blood in stool, fever, or a family history of colon cancer, don’t delay-see a gastroenterologist.
Also, if you’ve tried diet, stress management, and medications for 6 months with no improvement, ask about referral to a specialized IBS clinic. Not all doctors know how to manage IBS-M. Find one who does.
IBS-Mixed is exhausting, but it’s not hopeless. With the right tools, you can stop letting your gut run your life.




Melissa Melville - 1 February 2026
This post is a godsend. I’ve been Googling for years and this is the first time someone actually explained why my gut hates me.
vivian papadatu - 2 February 2026
I’ve been on low FODMAP for 5 months now. Started with zero hope, but after week 6, I could actually plan a weekend trip without packing extra underwear. It’s not perfect, but it’s the first time I feel like I’m not just surviving.
Naomi Walsh - 3 February 2026
Low FODMAP? Please. That’s just a trendy diet for people who think their digestive system is a personal brand. Real medicine is about pharmaceuticals, not kale smoothies. And don’t get me started on ‘gut-brain axis’-it’s all just neurohype wrapped in organic packaging.
Angel Fitzpatrick - 5 February 2026
They don’t want you to know this, but IBS-M is a government bioweapon disguised as a syndrome. The FDA approved ibodutant? That’s just a cover. They’re testing gut-targeted neurochemicals on the population to make us docile. You think your bloating’s random? Nah. It’s programmed. Check your water supply. And your probiotics? Probably laced with glyphosate.
Jamie Allan Brown - 6 February 2026
I’ve been living with IBS-M for 12 years. The antidepressants were the real game-changer for me. Not because I’m depressed-because my gut nerves are screaming. Amitriptyline at night? I didn’t believe it until I slept through the night for the first time in a decade. No jokes. Just quiet.
Nicki Aries - 7 February 2026
Just want to say-thank you for mentioning the Bristol Scale. So many people say ‘I’m constipated’ or ‘I’m diarrhea’ without realizing they’re describing two different medical conditions. Tracking with an app changed everything for me. I finally saw that my ‘stress spikes’ were always after eating gluten-free bread with inulin. Who knew?
Ed Di Cristofaro - 7 February 2026
People act like this is some big revelation, but I’ve been doing this since 2018. Low FODMAP, peppermint oil, amitriptyline-same damn routine. The only thing new here is the fancy formatting. You’re not special. You’re just late to the party.
Lilliana Lowe - 8 February 2026
The author cites a 2021 Cochrane review but fails to mention that the effect size was clinically marginal (Cohen’s d = 0.32). Also, the Rome V criteria revision to 30% is statistically arbitrary-why not 35%? Or 28%? The entire diagnostic framework lacks reproducibility. This article reads like a marketing brochure for a gut-health influencer.
Bob Cohen - 9 February 2026
Okay, but have you tried intermittent fasting? I know it sounds wild, but cutting your eating window to 6 hours dropped my flare-ups by 80%. No meds, no diet shifts. Just stop snacking. Your gut needs a break, not another supplement.
Ishmael brown - 11 February 2026
Low FODMAP? That’s just the Paleo diet with extra steps. Also, I’m pretty sure ‘enteric-coated peppermint oil’ is just a fancy way of saying ‘expensive mint capsules.’ I used to chew raw peppermint leaves before bed. Worked better than any pill. And cheaper.
Nancy Nino - 13 February 2026
While I appreciate the clinical rigor of this article, I must respectfully note that the inclusion of ‘5 minutes of deep breathing’ as a therapeutic intervention borders on the patronizing. The human gut is not a relaxation app. It is a complex neuroendocrine organ. Reducing its management to mindfulness is both reductive and dismissive of the physiological burden borne by patients.
Deep Rank - 14 February 2026
you know what really helped me? giving up on trying to fix it. i mean, like, i just accepted that my gut is a chaotic mess and now i just wear dark pants and carry wipes everywhere. also, i stopped caring if people think i’m weird for leaving dinner early. honestly, life got better when i stopped fighting it. and yes, i still eat onions but now i just say ‘it’s my vibe’ and move on. also, i tried every probiotic known to man and only the one with the weird blue capsule worked, but i don’t remember the name. it was like $40 and i bought it at a gas station in texas. the guy behind the counter said ‘that’s the one the doctor uses’ so i trusted him. he had a tattoo of a colon. i think he knew.
June Richards - 15 February 2026
Why is everyone so obsessed with FODMAPs? I just eat more carbs and it’s fine. Also, IBS is just stress. Go outside. Get a dog. Stop overthinking your poop.
Lu Gao - 17 February 2026
Low FODMAP? Nah. I tried that. Then I went full keto. Then I did carnivore. Then I ate only bananas and oatmeal for 3 weeks. Still had diarrhea. Then I started drinking kombucha with lemon juice and ginger. Now I’m fine. Turns out, your gut just needs a little rebellion. 🍌🍋