What Is a Rotator Cuff Tear?
A rotator cuff tear happens when one or more of the tendons connecting the shoulder muscles to the bone rip or fray. These four muscles - supraspinatus, infraspinatus, teres minor, and subscapularis - work together to keep your shoulder stable and let you lift and rotate your arm. Without them, your shoulder feels weak, painful, and hard to move normally.
These tears don’t always come from a single injury. Many people develop them slowly over time, especially after 40. In fact, studies show that over half of people over 60 have a rotator cuff tear without any symptoms. That’s right - you can have a torn tendon and not even know it. But when pain, weakness, or trouble lifting your arm shows up, it’s time to pay attention.
How Doctors Diagnose Rotator Cuff Tears
Before any scans, your doctor will start with a physical exam. They’ll check your range of motion, test your strength, and use specific moves like the Empty Can test or Hawkins-Kennedy test to see if your shoulder reacts with pain. These aren’t just guesses - they’re proven methods backed by decades of clinical use.
After that, imaging is next. But not all scans are created equal.
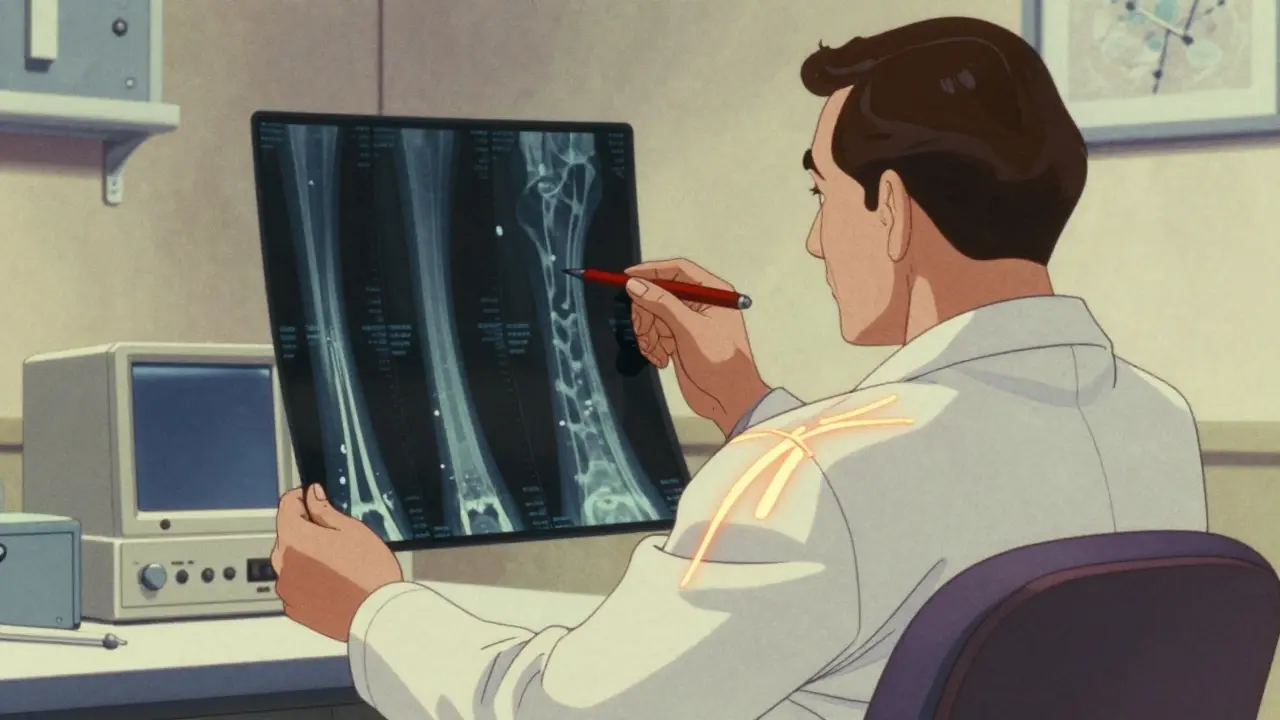
X-Rays: The First Step
Every single patient gets an X-ray first. Why? It doesn’t show the tendon itself, but it reveals bone problems that could be causing the pain - like bone spurs, arthritis, or changes in the shoulder joint. If your X-ray looks normal, it doesn’t mean there’s no tear. It just means the problem is likely soft tissue.
Ultrasound vs. MRI: Which One Do You Need?
This is where things get practical.
Ultrasound is fast, cheap, and safe. It costs about $200-$400, while an MRI can run $500-$1,200. It doesn’t use radiation or magnets, so it’s fine if you have a pacemaker or metal implants. You can even watch the tendon move in real time as you lift your arm. That’s huge - because sometimes the tear only shows up when the shoulder is under load. The downside? It depends heavily on who’s doing the scan. Only about 45% of general radiologists are trained well enough to read it accurately.
MRI gives a much clearer, detailed picture of the tendon’s condition - whether it’s a partial tear, full-thickness tear, or just inflamed. It’s 92% accurate for full-thickness tears and 95% specific for partial ones. But it’s slower, louder, and not ideal for people with claustrophobia or certain implants. Plus, it’s often overused. The American Roentgen Ray Society says ultrasound should be the first imaging test for most cases because it’s just as accurate for detecting tears and way more accessible.
Doctors usually pick MRI when they’re planning surgery and need a detailed map of the shoulder - like knowing exactly how big the tear is, how much muscle has shrunk, or if other structures are involved.
When Do You Need Surgery?
Not every tear needs surgery. In fact, most people with partial tears or small full-thickness tears get better with rehab alone.
Studies show that 85% of patients with partial-thickness tears recover full function after 3-6 months of physical therapy. That’s without a single cut or stitch.
But surgery becomes the better option if:
- You’re under 65 and active - you need your shoulder for work, sports, or daily life
- You have a full-thickness tear larger than 1 cm
- Conservative rehab hasn’t helped after 6-8 weeks
- You’ve lost significant strength - like being unable to lift your arm above shoulder height
For people over 65 with low activity levels, doctors often recommend skipping surgery. Why? Healing is slower, retear rates are higher, and the risks don’t always outweigh the benefits.
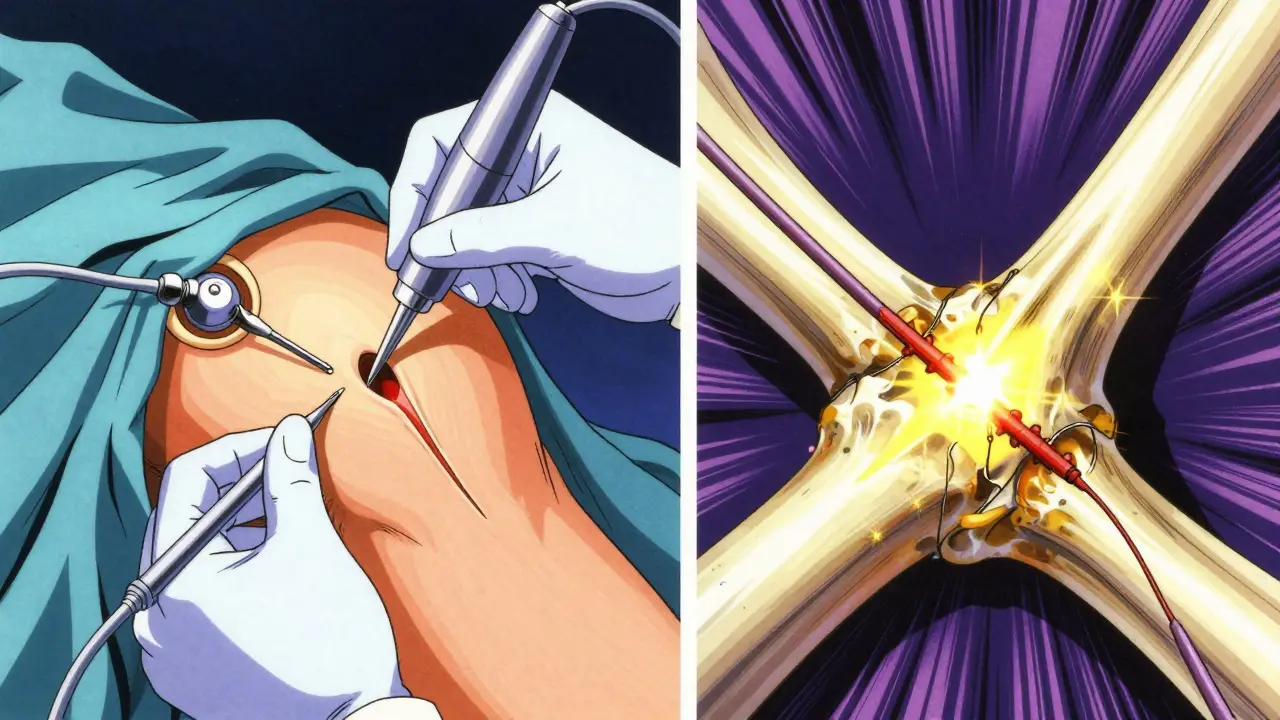
Surgical Options: Arthroscopic, Mini-Open, or Open?
Today, over 90% of rotator cuff repairs are done arthroscopically. That means the surgeon makes 2-4 small keyhole incisions, inserts a camera, and uses tiny tools to stitch the tendon back to the bone.
Compared to the old-school open surgery - which required a 3-5 inch incision - arthroscopic repair has:
- 30% fewer complications
- 25% faster return to daily activities
- Less pain and scarring
Mini-open repairs are a hybrid - a small incision with some direct access. They’re used less often now, mostly for very large or complex tears.
Open surgery is rare today, reserved for massive tears where the tendon is too damaged to be repaired with minimally invasive tools.
Rehabilitation: The Real Key to Recovery
Surgery doesn’t fix your shoulder - rehab does. A repair is just the starting point. Without the right rehab, you risk stiffness, retears, or permanent weakness.
Here’s what a typical rehab timeline looks like:
- Weeks 1-6: Passive Motion Only - No muscle activation. Your arm is supported by a sling. A therapist moves your shoulder gently to prevent stiffness. You can’t lift or push anything.
- Weeks 6-12: Active-Assisted Motion - You start moving your arm on your own, with help from your other hand or a pulley. Light resistance bands may be introduced.
- Weeks 12-24: Strengthening - Focus shifts to rebuilding rotator cuff and deltoid strength. Exercises like external rotation with bands, scapular squeezes, and wall push-ups begin.
- Months 6+: Functional Training - Returning to sports, lifting, or heavy work. This phase is individualized. A tennis player’s rehab differs from a carpenter’s.
Modern rehab starts earlier than in the past. Ten years ago, patients were locked in slings for 6 weeks. Now, most surgeons allow passive motion within days of surgery. That’s because research shows early movement reduces stiffness and improves long-term outcomes.
What About PRP or Patch Augmentation?
Some clinics offer platelet-rich plasma (PRP) injections during surgery - claiming it speeds healing. But the Cochrane Review in 2021 found only moderate, inconsistent evidence for PRP. It’s not standard care, and insurance rarely covers it.
For massive tears where the tendon is too frayed to be stitched back, surgeons sometimes use a biological patch - a graft made from donor tissue or synthetic material - to bridge the gap. These are still experimental in many places, but early results show promise for younger, active patients who can’t afford a retear.
Long-Term Outcomes: What to Expect
After arthroscopic repair, 82% of patients report being satisfied with their results at the 5-year mark. That sounds good - until you look closer.
Retear rates vary by tear size:
- Small tears (<1 cm): 12% retear rate
- Medium tears (1-3 cm): 20% retear rate
- Large tears (>3 cm): 27% retear rate
And here’s the kicker - even if the tendon retears, many people still feel better. Why? Because the pain often comes from inflammation, not just the tear. Once that’s calmed down, the body adapts. That’s why rehab and pain management matter just as much as the surgery itself.
What You Can Do Right Now
If you’re dealing with shoulder pain:
- Don’t rush to surgery. Try 6-8 weeks of physical therapy first.
- If imaging is needed, ask for ultrasound before MRI - it’s cheaper, faster, and just as accurate for most cases.
- If you’re over 60 and have no symptoms, don’t panic if you see a tear on an MRI. Many people do.
- Stay active. Avoiding movement makes stiffness worse. Gentle shoulder circles, wall climbs, and pendulum swings are safe starting points.
When to See a Specialist
See an orthopedic shoulder specialist if:
- Pain lasts more than 6 weeks despite rest and OTC meds
- You can’t lift your arm above shoulder level
- You have sudden weakness after an injury
- You’re under 65 and active, and the pain is limiting your life
Don’t wait. Delaying treatment can lead to muscle atrophy - where the muscle shrinks and turns to fat. Once that happens, repair becomes harder, and outcomes worsen.


Marlon Mentolaroc - 24 January 2026
Honestly, this is the most practical breakdown I've seen in years. Ultrasound first? Yes. MRI like it's a Netflix subscription? No. I've seen too many people get billed for $1,200 scans when a $300 ultrasound would've told them everything they needed to know. Stop overmedicalizing shoulder pain.
siva lingam - 25 January 2026
so u mean if i dont feel pain my tendon is just chillin like it on vacation
Shelby Marcel - 26 January 2026
i had a tear n never knew it until my physio said 'uhhh u sure u never hurt this?' i thought i was just getting old. turns out my supraspinatus was basically a shredded cheese grate. now i do my little pendulum swings like a zen monk. weirdly calming.
Phil Maxwell - 27 January 2026
I read this while doing my rehab exercises. The part about early passive motion made me feel less guilty for moving my arm a little too soon after surgery. My PT said it was fine, but I still felt like I was cheating. Turns out, research backs it. Good to know I’m not the only one trying to move before the 6-week mark.
blackbelt security - 27 January 2026
Rehab isn't optional. It's the real surgery. I thought the operation was the finish line. Turns out it was just the starting gate. 18 months later, I'm back lifting. Not because of the surgeon. Because of the PT who didn't let me quit.
Patrick Gornik - 28 January 2026
Let’s deconstruct the metaphysical implications of tendon integrity within the ontological framework of embodied agency. The rotator cuff isn't merely a biomechanical assembly-it's a phenomenological interface between volition and somatic limitation. When the supraspinatus frays, we aren't merely losing tensile strength-we're losing the capacity to assert our corporeal sovereignty against the entropy of aging. The surgical repair? A symbolic reclamation of autonomy. But here's the kicker: the *real* rupture isn't in the tendon-it's in the cultural mythos that equates physical integrity with moral worth. Why do we pathologize asymptomatic tears? Because society fears the silent decay of utility. We don't mourn the torn tendon-we mourn the lost productivity. PRP? A neoliberal placebo for the anxious bourgeoisie who can't accept that bodies, like institutions, are inherently ephemeral. Patch augmentation? A techno-utopian band-aid on the wound of a culture that refuses to let go.
Izzy Hadala - 30 January 2026
The data presented here aligns closely with the 2023 systematic review by the Journal of Shoulder and Elbow Surgery, particularly regarding ultrasound’s diagnostic equivalence to MRI for full-thickness tears (AUC 0.91 vs. 0.93). However, the author’s assertion that ultrasound is underutilized requires contextual qualification: in tertiary care centers with dedicated musculoskeletal radiologists, ultrasound sensitivity approaches 90%. The real barrier is not technological but institutional-reimbursement structures favor MRI due to higher CPT code valuations. Furthermore, the 85% success rate for nonoperative management of partial-thickness tears is corroborated by the 2022 multicenter cohort study by the American Academy of Orthopaedic Surgeons, which demonstrated that patient-reported outcomes improved significantly even in the absence of tendon healing, suggesting functional adaptation as a key compensatory mechanism. This reinforces the necessity of patient-centered decision-making over anatomical perfectionism.
Tommy Sandri - 31 January 2026
In the United States, the overuse of MRI for shoulder pain reflects broader systemic trends in healthcare economics. The cost differential between ultrasound and MRI is not merely financial-it is cultural. In nations with universal healthcare systems, such as the UK and Canada, ultrasound is the standard first-line imaging modality for rotator cuff pathology. The U.S. model, driven by fee-for-service incentives and defensive medicine, often prioritizes high-cost imaging even when clinical utility is marginal. This is not a failure of medical knowledge, but of structural alignment. The path forward lies not in more scans, but in retraining clinicians to trust clinical acumen and in reforming reimbursement policies to incentivize cost-effective, evidence-based care. The shoulder does not care about the price tag of the machine that sees it.