Touch Korea Pharmacy Online Review: Get 15% Discount on International Pharmacy Products
Dec 7 2023 - Health and Wellness Reviews
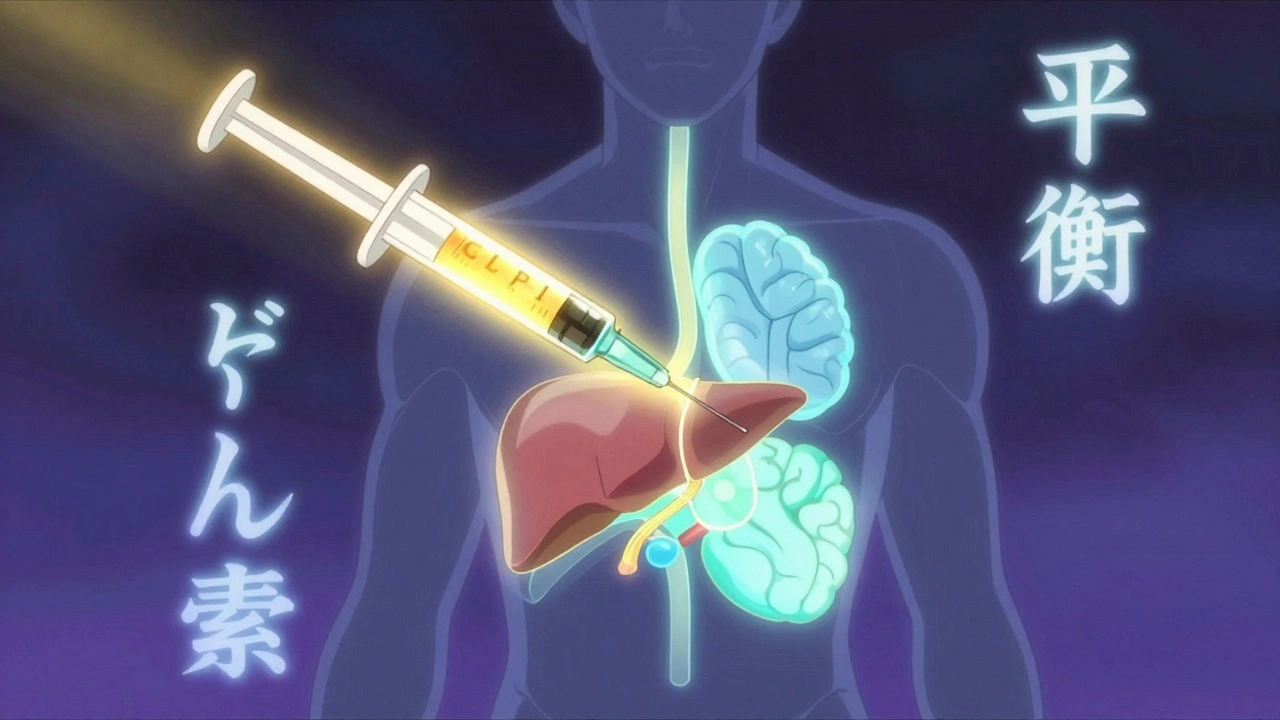
When you hear GLP-1 agonists, a class of prescription drugs that mimic a natural hormone in your gut to help control blood sugar and reduce appetite. Also known as incretin mimetics, they’re not just for diabetes—they’ve become one of the most studied tools for long-term weight management. Drugs like semaglutide and liraglutide don’t just lower blood sugar; they slow digestion, reduce hunger, and signal your brain that you’re full. That’s why they’re now used for both type 2 diabetes and obesity, even in people without diabetes.
These drugs work by activating the GLP-1 receptor, a protein found in the pancreas, brain, and stomach that helps regulate insulin and appetite. When you eat, your body naturally releases GLP-1, but it breaks down in minutes. GLP-1 agonists last much longer, giving your body steady signals to release insulin only when needed and to feel satisfied with less food. This is different from older diabetes drugs that force insulin out regardless of blood sugar levels, which can cause dangerous lows. With GLP-1 agonists, the risk of hypoglycemia is low unless you’re also taking insulin or sulfonylureas.
They’re not magic pills, though. Side effects like nausea, vomiting, and diarrhea are common at first but often fade. Some people experience more serious issues—pancreatitis, gallbladder disease, or rare cases of thyroid tumors in animal studies. That’s why they’re prescribed, not sold over the counter. The real value isn’t just in the scale dropping—it’s in improved blood pressure, cholesterol, and reduced risk of heart attacks in high-risk patients. Studies show people on these drugs lose 10-20% of their body weight over a year, often keeping it off longer than with diet and exercise alone.
These drugs are part of a bigger picture. They connect to insulin resistance, a condition where your body doesn’t respond well to insulin, leading to high blood sugar and fat storage, which is at the core of type 2 diabetes and obesity. They also tie into how medication adherence, how consistently patients take their drugs as prescribed affects long-term outcomes. If you skip doses, the hunger signals return, and weight creeps back. That’s why many users pair them with simple habits—like tracking meals, staying hydrated, or setting phone reminders.
You’ll find posts here that dig into how these drugs interact with other medications, why some people respond better than others, and what the real-world data says about safety over time. There’s also coverage on how insurance rules affect access, how pharmacists help patients manage side effects, and why switching between brands and generics can matter—especially when every milligram counts. Whether you’re on one of these drugs, considering it, or just trying to understand the hype, this collection gives you clear, no-fluff facts from people who’ve seen them in practice.
GLP-1 receptor agonists like Ozempic and Wegovy help lower A1C and promote significant weight loss by targeting appetite, insulin, and digestion. Learn how they work, which drugs are most effective, and what to expect before starting.
read more© 2026. All rights reserved.
