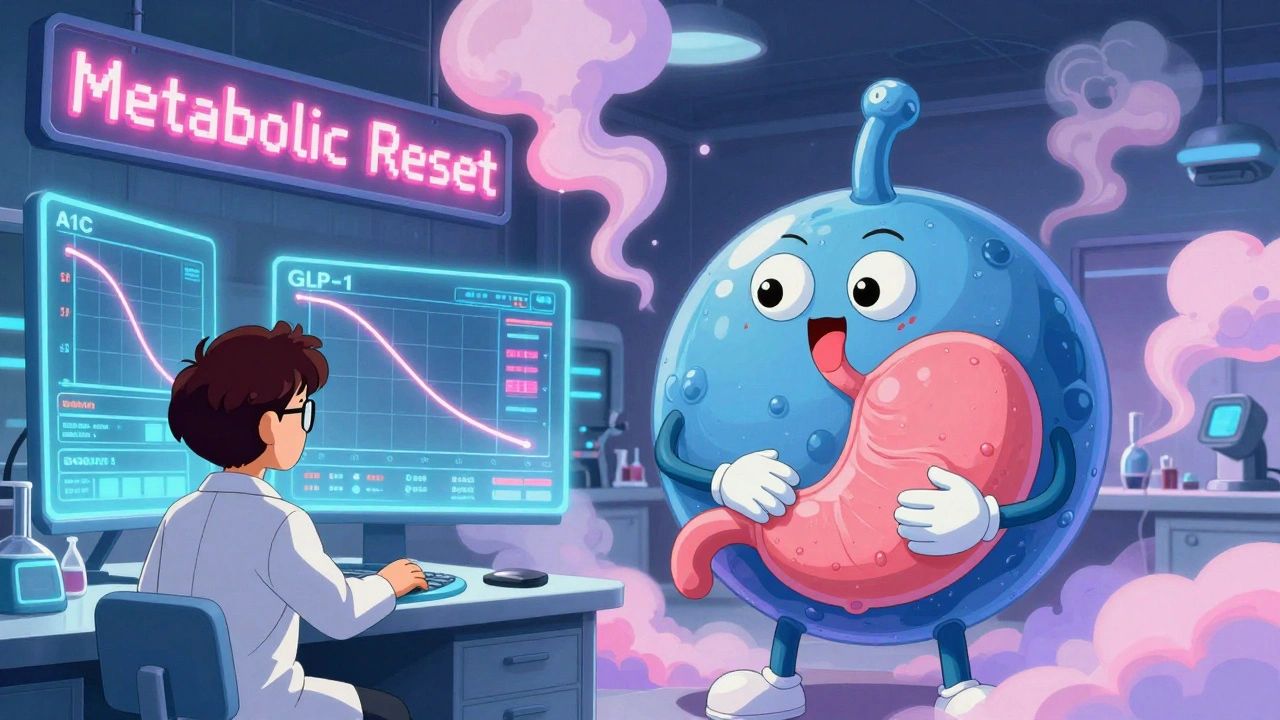
Diabetes and weight management used to be treated as two separate problems. You’d take a pill to lower your blood sugar, and maybe another to lose weight - if you could even get one. But that’s changed. Today, a new class of drugs called GLP-1 receptor agonists is rewriting the rules. These aren’t just diabetes meds. They’re turning into game-changers for weight loss, too. And the numbers don’t lie: people are losing up to 15% of their body weight while bringing their A1C down by nearly 2%. This isn’t magic. It’s science - and it’s working for millions.
How GLP-1 Receptor Agonists Actually Work
GLP-1 is a hormone your body makes naturally after you eat. It tells your pancreas to release insulin when blood sugar rises. It also slows down your stomach, so food doesn’t rush through. And it talks to your brain, telling you you’re full. GLP-1 receptor agonists mimic this hormone. They’re synthetic versions that stick to the same receptors and do the same jobs - but better and longer.
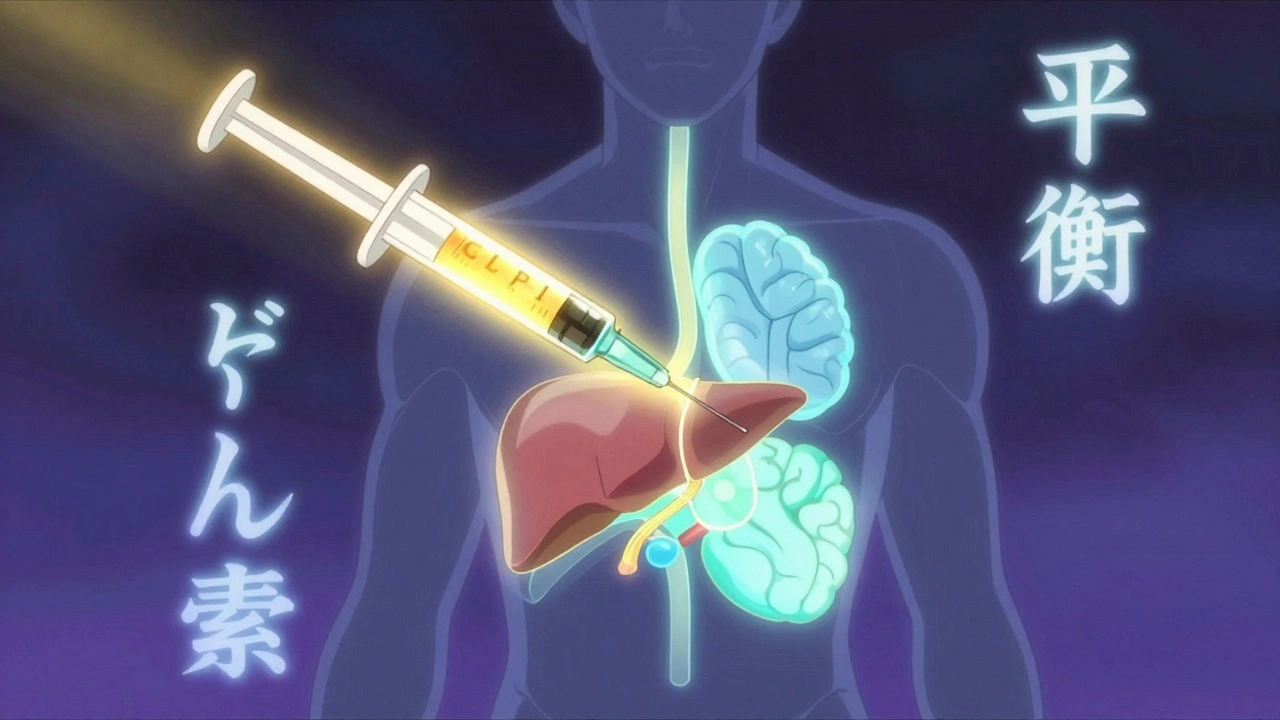
Here’s what happens in your body when you take one:
- Your pancreas releases more insulin - but only when your blood sugar is high. That means less risk of low blood sugar compared to older drugs like insulin or sulfonylureas.
- Your liver makes less glucose. That’s a big deal because many people with type 2 diabetes have a liver that’s overproducing sugar.
- Your stomach empties slower. Food stays in longer, so blood sugar spikes after meals don’t happen as hard.
- Your brain gets the signal: you’re full. Hunger drops by 30-40%. Cravings for sugary, fatty foods fade. One user on Reddit said, “I used to snack every two hours. Now I forget I’m hungry until lunch.”
It’s not just one mechanism. It’s a full system reset. That’s why these drugs work so well for both diabetes and weight loss at the same time.
Which Drugs Are Actually Working?
Not all GLP-1 agonists are the same. Some are stronger, some last longer, and some cost way more. Here’s what’s out there as of 2025:
| Drug Name | Brand Names | Dose Frequency | A1C Reduction | Average Weight Loss |
|---|---|---|---|---|
| Semaglutide | Ozempic (diabetes), Wegovy (weight) | Once weekly | 1.8% | 14-15% |
| Tirzepatide | Mounjaro (diabetes), Zepbound (weight) | Once weekly | 2.0-2.4% | 18-21% |
| Liraglutide | Victoza (diabetes), Saxenda (weight) | Once daily | 1.1-1.2% | 6-8% |
| Dulaglutide | Trulicity | Once weekly | 1.5-1.7% | 5-7% |
Tirzepatide is the new standout. It’s not just a GLP-1 agonist - it’s a dual agonist. It also activates GIP, another gut hormone that helps with fat burning and insulin sensitivity. In the SURMOUNT-2 trial, people lost over 20% of their body weight on the highest dose. That’s closer to bariatric surgery results than anything you could get from diet pills.
But here’s the catch: Ozempic and Wegovy are the same drug. The only difference is the dose. Ozempic is for diabetes at 0.5-1.0 mg. Wegovy is for weight loss at 0.25-2.4 mg. Same molecule. Different strength. Same goes for Mounjaro and Zepbound.
Why This Is a Big Deal for Weight Loss
Before GLP-1 agonists, weight loss drugs were either weak or risky. Phentermine? It worked for a few weeks and then stopped. Orlistat? Made you leak oil. Even the newer ones like semaglutide were only approved for weight loss in 2021 - and even then, only for people with a BMI over 30.
Now, the data shows something shocking: most people on semaglutide lose at least 10% of their body weight. Half lose 15% or more. In the STEP 3 trial, 86% lost 5% or more. That’s not just “feeling better.” That’s reversing prediabetes, lowering blood pressure, reducing sleep apnea, and sometimes even getting off insulin.
One woman in the UK, 54, lost 62 pounds in 10 months on Wegovy. Her A1C dropped from 8.2% to 5.8%. Her doctor told her she was no longer diabetic. She didn’t change her diet much - just started the shot. “It wasn’t willpower,” she said. “It was my brain finally letting go of hunger.”
That’s the real shift. These drugs don’t just suppress appetite. They change your relationship with food. Sugar stops tasting addictive. Junk food stops feeling like a reward. It’s not just losing weight - it’s rewiring your cravings.
The Catch: Side Effects and Real-World Challenges
Nothing is perfect. And these drugs come with trade-offs.
Nausea is the most common side effect. About 1 in 5 people feel sick when they start - especially during the first few weeks of dose increases. Vomiting happens to 5-10%. Diarrhea? Around 1 in 4. But here’s the good news: most people get used to it. The symptoms fade as your body adjusts. Doctors recommend starting low and going slow. If you’re on Wegovy, you begin at 0.25 mg for a month before bumping up. Rushing it makes side effects worse.
Some people report dizziness or fatigue. Rarely, there’s a risk of pancreatitis or gallbladder issues. The FDA has warned about thyroid tumors in rodents - but no proven link in humans after 15 years of use.
Biggest problem? Cost and access.
In the U.S., without insurance, a monthly supply of Wegovy or Ozempic can cost $1,200. Even with insurance, many plans require you to try and fail on other weight loss methods first. Medicare Part D covers about 62% of prescriptions - but often only for diabetes, not weight loss. In the UK, NHS access is limited to those with severe obesity and diabetes. Most people pay out of pocket.
And then there’s the shortage. Semaglutide has been on the FDA’s shortage list since early 2022. Pharmacies run out. Doctors can’t get enough. Some patients get switched to older, less effective versions just to keep going.
What Happens When You Stop?
This is the question no one wants to ask - but everyone should.
Studies show that if you stop taking GLP-1 agonists, you regain most of the weight. On average, people put back 50-70% of what they lost within a year. That’s not because they “failed.” It’s because the drug was doing the work your body no longer does on its own.
Think of it like blood pressure medication. You don’t stop taking it because you feel better. You keep taking it because your body needs the help. Same here. For many, this isn’t a short-term fix. It’s a long-term tool.
Some experts are now talking about “maintenance dosing” - lowering the dose once you reach your goal to keep the weight off. Others are exploring combining these drugs with lifestyle changes to build lasting habits. The goal isn’t to stay on forever - it’s to give you the space to rebuild your metabolism.
How to Get Started - and What to Expect
If you’re considering one of these drugs, here’s what to know:
- See a specialist. Not every doctor knows how to prescribe these. Endocrinologists, obesity medicine doctors, or diabetologists are your best bet.
- Ask about insurance. Get your diagnosis code right. Diabetes? Weight-related conditions like high blood pressure or sleep apnea? Those help get coverage.
- Start low. Don’t jump to the highest dose. Give your body time to adjust. Nausea is worse if you rush.
- Track your progress. Weigh yourself weekly. Check your A1C every 3 months. Note changes in hunger, energy, and cravings.
- Don’t expect miracles overnight. Weight loss happens slowly. Most people see results after 8-12 weeks. The real magic is in the long run.
Injection anxiety is common. Most pens are designed to be simple - small needles, hidden tips. Many clinics offer training. You’ll get used to it faster than you think.
The Future: What’s Next?
GLP-1 agonists are just the beginning. Researchers are now testing triple agonists - hitting GLP-1, GIP, and glucagon receptors at once. Early results show weight loss over 25%. Oral versions are coming too. Novo Nordisk has an oral semaglutide pill approved for diabetes - and they’re testing it for weight loss.
There’s also exciting work in heart failure, fatty liver disease, and even Alzheimer’s. Semaglutide showed improved heart function in patients with heart failure and obesity. In liver studies, it cut liver fat by more than half.
These aren’t just weight loss drugs anymore. They’re metabolic reset tools. And as more evidence piles up, they’re becoming standard care - not just for diabetes, but for overall health.
Are GLP-1 agonists only for people with diabetes?
No. While they were first approved for type 2 diabetes, drugs like Wegovy and Zepbound are specifically approved for chronic weight management in adults with obesity (BMI ≥30) or overweight (BMI ≥27) with at least one weight-related condition like high blood pressure or sleep apnea. You don’t need diabetes to qualify.
How long does it take to see weight loss results?
Most people start seeing weight loss after 4-8 weeks, but the biggest changes happen between 16 and 68 weeks. In clinical trials, people lost the most weight after 68 weeks on the full dose. It’s a slow build - but the results are lasting while you’re on the drug.
Can I take GLP-1 agonists with other weight loss medications?
Combining them with other weight loss drugs like phentermine or naltrexone/bupropion isn’t common and isn’t officially approved. Some doctors do it off-label, but there’s limited safety data. Always talk to your doctor before mixing medications. The risk of side effects - especially nausea - goes up.
Do these drugs cause muscle loss?
Some weight loss on GLP-1 agonists includes muscle loss, especially if you’re not eating enough protein or exercising. Studies show about 20-30% of the weight lost can be lean mass. To protect muscle, aim for 1.6-2.2 grams of protein per kilogram of body weight daily and include strength training 2-3 times a week.
Is there a cheaper alternative to Ozempic or Wegovy?
There’s no true generic yet, but some people use compounded semaglutide from specialty pharmacies - though these aren’t FDA-approved and carry safety risks. Liraglutide (Saxenda) is older and often cheaper, but it requires daily injections and gives less weight loss. Tirzepatide is more effective but usually more expensive. Insurance coverage and patient assistance programs can help reduce costs significantly.


Adrianna Alfano - 2 December 2025
I lost 37 pounds on Wegovy and my A1C dropped to 5.4. My mom said I looked like a different person. I didn’t even change my diet that much. Just stopped craving donuts. My brain finally shut up about food. I used to eat cereal at 2am. Now I sleep through the night. No more guilt. No more shame. Just quiet.
Casey Lyn Keller - 3 December 2025
These drugs are just Big Pharma’s way of keeping people dependent. You think you’re getting healthy but you’re just trading one addiction for another. The real solution is fasting and discipline. Not a shot that turns your brain off. They’re selling weakness as science.
Jessica Ainscough - 3 December 2025
I started on liraglutide last year. Nausea was brutal for the first two weeks. But after that? I didn’t even notice I was eating less. I just… stopped wanting junk. I didn’t feel deprived. It felt like my body finally stopped fighting me. Still taking it. No regrets.
May . - 5 December 2025
theyre just making people sick to lose weight and charging 1200 a month
Michael Bene - 5 December 2025
Let me break this down for you. Tirzepatide isn’t magic. It’s a chemical leash. You’re not losing weight - you’re being chemically pacified. Your hunger isn’t gone, it’s suppressed like a dog with a shock collar. And when you stop? The cravings come back like a damn hurricane. Plus, did you know the FDA’s rodent tumor data was buried under three layers of legalese? This isn’t medicine. It’s corporate sedation dressed in lab coats.
And don’t get me started on the shortages. That’s not supply chain. That’s intentional scarcity to jack up prices. Novo Nordisk knows people will pay $1200 for a shot that makes them stop thinking about pizza. That’s capitalism at its most elegant and evil.
Meanwhile, your doctor’s probably getting kickbacks from pharma reps. They don’t care if you’re healthy. They care if you’re on the drug. Ask them if they’ve ever prescribed this to themselves. I’ll wait.
And yes, muscle loss is real. You’re not getting lean. You’re getting smaller with less muscle. You think that’s sustainable? You think your metabolism isn’t screaming for help? You’re trading a long-term metabolic collapse for short-term vanity. And you call this progress?
There’s a reason people in the 80s didn’t need these shots. They ate real food. They moved. They didn’t outsource their willpower to a pharmaceutical placebo with side effects named after Greek gods.
Don’t be fooled. This isn’t science. It’s seduction with a syringe.
Brian Perry - 7 December 2025
My cousin got on Ozempic and started crying over a bag of chips. Like, full-on sobbing. She said she didn’t even want them anymore but her brain kept screaming for sugar. Then she got pancreatitis. Hospital for a week. Now she’s off it. Said she’d rather be fat and alive than skinny and in pain. I don’t know man. I think we’re losing our minds.
Chris Jahmil Ignacio - 7 December 2025
People think this is a weight loss drug. It’s not. It’s a control drug. The same people pushing this are the ones who banned trans fats and sugar taxes and now want to force you into lifelong injections. This isn’t about health. It’s about control. You think the government doesn’t want you dependent on a monthly shot so they can track your habits? Think again. They’re already watching. This is the next step in the surveillance economy.
And the worst part? They’re making it so expensive that only the rich can afford it. Then they say poor people are lazy because they’re not losing weight. It’s a trap. A beautiful, shiny, expensive trap.
My uncle lost 50 lbs on this. Then he died of a stroke. Coincidence? I don’t believe in coincidences anymore.
Paul Corcoran - 8 December 2025
I’ve been a diabetes educator for 18 years. I’ve seen people struggle with insulin pumps, carb counting, endless glucose checks. Then I watched someone go from an A1C of 9.8 to 5.6 on semaglutide - not because they were perfect, but because the drug gave them breathing room. They started walking. They slept better. They stopped feeling like a failure.
Yes, side effects happen. Yes, cost is brutal. Yes, you’ll regain weight if you stop. But so what? That’s true for blood pressure meds, thyroid meds, antidepressants. We don’t shame people for taking those. Why shame this?
These aren’t magic. But they’re not evil either. They’re tools. And sometimes, when your body’s broken, you need a tool to help you rebuild. Not forever. Just long enough to find your footing.
If you’re on it, I’m proud of you. If you’re scared of it, ask questions. If you’re angry about the cost, fight for access. But don’t call it a conspiracy. It’s medicine. Imperfect. Expensive. Real. And for millions? Life-changing.