When a woman reaches menopause, her body doesn’t just stop having periods-it starts changing how it handles every medication she takes. Hormone levels drop, liver function slows, kidney filtration decreases, and muscle mass declines. These aren’t minor shifts. They alter how drugs are absorbed, broken down, and cleared from the body. For post-menopausal women, who often take four to five prescriptions daily, these changes can turn a safe dose into a dangerous one. Medication safety isn’t just about avoiding side effects-it’s about recognizing that the same pill that worked at 50 might harm at 65.
Why Hormone Therapy Isn’t One-Size-Fits-All
Estrogen therapy used to be prescribed widely to prevent heart disease and osteoporosis after menopause. That changed after the Women’s Health Initiative study in 2002 showed that combined estrogen-progestin therapy increased breast cancer risk by 24% and raised the chance of stroke and blood clots. The U.S. Preventive Services Task Force now gives a D recommendation against using combined hormone therapy for chronic disease prevention in post-menopausal women. But that doesn’t mean hormone therapy has no place. For women under 60 or within 10 years of menopause onset, it can still be the most effective treatment for hot flashes, night sweats, and vaginal dryness.The key is choosing the right type and route. Oral estrogen passes through the liver first, increasing clotting factors and triglycerides. Transdermal estrogen-applied as a patch or gel-bypasses the liver. Studies show it cuts the risk of venous thromboembolism by more than half compared to pills. For women with a history of blood clots, migraines with aura, or high triglycerides, transdermal is often the only safe option. The Endocrine Society recommends starting with the lowest effective dose for the shortest time needed. For women who’ve had a hysterectomy, estrogen alone may be safer than combined therapy, with no significant increase in breast cancer risk.
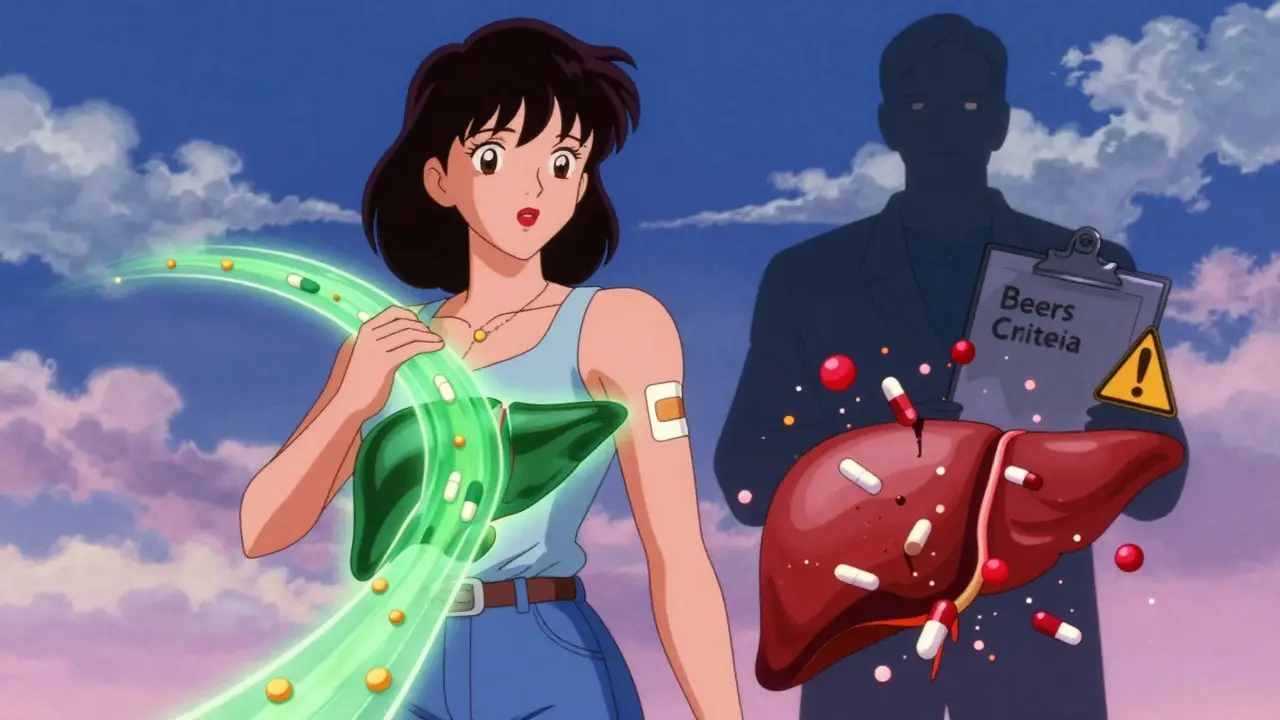
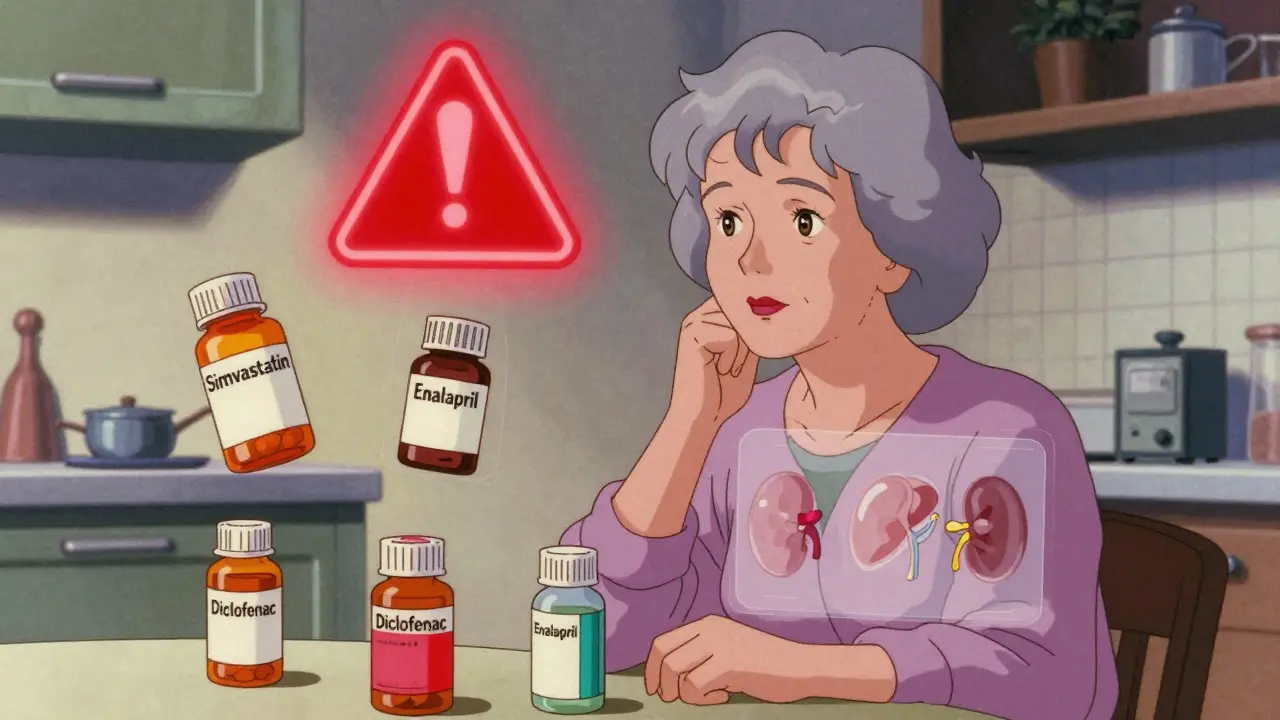
Polypharmacy: When More Medicines Mean More Risk
Post-menopausal women are the most likely group to take multiple medications. About 44% of women over 65 are on five or more prescriptions. Some are for menopause symptoms, others for high blood pressure, cholesterol, arthritis, diabetes, or depression. But when you stack drugs together, interactions multiply. A common combination-simvastatin for cholesterol, enalapril for blood pressure, and diclofenac for joint pain-can lead to kidney damage, muscle breakdown, or bleeding ulcers. The WHO calls this polypharmacy a global crisis. One study found that 40% of older adults get prescriptions from multiple doctors, with no one reviewing the full list.Many medications commonly prescribed to older adults are now flagged as risky. The Beers Criteria, updated in 2019, lists 30 drugs to avoid in people over 65. Long-acting benzodiazepines like diazepam increase hip fracture risk by 50%. Anticholinergics like diphenhydramine (Benadryl) worsen memory and confusion. Nonsteroidal anti-inflammatories (NSAIDs) like ibuprofen and naproxen raise the risk of stomach bleeding, especially in women over 65. One case study described a 72-year-old woman who developed a life-threatening ulcer after continuing diclofenac despite being told to stop. Her hemoglobin dropped from 12.5 to 8.1 g/dL in just a week.
Deprescribing: The Art of Stopping What’s Not Needed
The goal isn’t just to add more drugs-it’s to stop the ones that don’t help anymore. Deprescribing means safely reducing or stopping medications that no longer benefit the patient. It’s not easy. Many patients fear stopping a pill, even if it’s causing harm. Doctors often don’t know how to start the conversation. But evidence shows it works. A 2019 WHO report found that structured deprescribing reduced medication burden by 1.4 drugs per patient and cut adverse drug events by 33%.Start with a full medication review. Bring every pill, supplement, and over-the-counter drug to your appointment-this is called a “brown bag review.” Ask: Is this still needed? What’s the goal? Is the benefit greater than the risk? For example, many women take low-dose aspirin for heart protection. But for women over 65, aspirin increases gastrointestinal bleeding risk by 58%. The benefit for primary prevention is often too small to justify the danger. The same goes for statins in women over 75 with no history of heart disease-many don’t gain meaningful protection.
Some drugs need slow tapering. Stopping antidepressants or benzodiazepines suddenly can cause rebound anxiety, insomnia, or seizures. Tapering should take 4 to 12 weeks, depending on the drug. Use tools like START/STOPP criteria, which identify 116 inappropriate medications and 81 underused ones for older adults. These aren’t just guidelines-they’re lifesavers.
Non-Hormonal Alternatives for Hot Flashes and More
Not every woman wants hormones. And not every woman can have them. The good news? There are effective non-hormonal options. Selective serotonin reuptake inhibitors (SSRIs) like paroxetine and escitalopram can reduce hot flash frequency by 50-60%. They’re not FDA-approved for this use, but multiple studies confirm their effectiveness. Gabapentin, originally for seizures, also helps with night sweats. Both can cause side effects-sexual dysfunction in 30-40% of users, dizziness, or weight gain-but for many, these are easier to live with than breast cancer risk.Other approaches include cognitive behavioral therapy (CBT), which reduces hot flash distress by 40-50%, and clinical hypnosis, shown in small trials to cut frequency by up to 75%. Lifestyle changes matter too: keeping the bedroom cool, avoiding alcohol and spicy food, and practicing paced breathing can reduce symptoms without pills. The NIH is investing $25 million into research on non-hormonal treatments through the MsFLASH network, signaling a shift away from one-size-fits-all hormone therapy.
Medication Errors Are Common-and Preventable
Even when prescriptions are right, mistakes happen. The National Poll on Healthy Aging found that 28% of women over 65 still make medication errors. The most common? Taking a pill twice (42%) or missing a dose (38%). Pill organizers help-studies show they reduce errors by 81%. But they’re not foolproof. If you’re taking 10 pills a day, even a good organizer can get confusing. Use color-coded labels. Set phone reminders. Ask a family member to check your pillbox weekly.Also, don’t assume your pharmacist knows your full list. Many pharmacies don’t communicate with each other. If you switch providers or get prescriptions from different clinics, your medication history can be fragmented. Always ask: “Is this new drug safe with everything else I’m taking?” And if you’re hospitalized, insist on a full medication reconciliation before discharge. One study showed that 60% of medication errors happen during hospital transitions.
What to Ask Your Doctor
You don’t need to be an expert to protect yourself. Here are five questions to ask at every medication review:- Is this medication still necessary, or is it just on autopilot?
- What are the risks versus benefits for someone my age and health status?
- Are there non-drug options I should try first?
- Is there a safer version of this drug-for example, transdermal instead of oral?
- Can we try reducing or stopping one of my meds to see how I feel?
Doctors are trained to add treatments. They need you to push back. If you’re unsure, ask for a referral to a geriatric pharmacist or a menopause specialist. These professionals specialize in medication complexity in older women.
Looking Ahead: Personalized Medicine is Coming
The future of medication safety for post-menopausal women is personal. Pharmacogenomics-testing how your genes affect drug metabolism-is becoming more accessible. For example, women taking tamoxifen for breast cancer prevention need to be tested for CYP2D6 gene variants. Some versions of this gene make tamoxifen ineffective. Others increase side effects. This kind of testing isn’t routine yet, but it’s coming.AI tools are also emerging. Pilot studies show AI-driven medication reconciliation systems reduce errors by 45% by spotting dangerous combinations, duplicate prescriptions, and outdated dosages. These tools aren’t perfect, but they help doctors see the whole picture.
For now, the best protection is awareness. Know your meds. Question them. Track your symptoms. Don’t accept a prescription just because it’s been on your list for years. Your body changed at menopause. Your medications should change too.
Is hormone therapy safe for post-menopausal women?
Hormone therapy can be safe for some women, especially those under 60 or within 10 years of menopause onset. Transdermal estrogen (patch or gel) is safer than oral forms because it avoids the liver, reducing blood clot risk. It’s recommended for managing hot flashes and vaginal symptoms, not for preventing heart disease or dementia. Absolute contraindications include a history of breast cancer, blood clots, stroke, or liver disease. Always discuss your personal risk factors with a specialist.
What medications should post-menopausal women avoid?
The Beers Criteria lists 30 drugs to avoid in adults over 65. These include long-acting benzodiazepines (like diazepam), anticholinergics (like diphenhydramine), NSAIDs (like ibuprofen and naproxen), and certain antipsychotics. These drugs increase risks of falls, confusion, stomach bleeding, and kidney damage. Even common OTC meds like sleep aids or allergy pills can be dangerous. Always review your full list with a pharmacist or geriatric specialist.
How can I reduce my risk of medication errors?
Use a pill organizer with clear labels, set phone alarms for doses, and keep an updated list of all medications-including supplements and OTC drugs. Bring this list to every doctor’s visit. Ask for a “brown bag review” where you bring all your pills in a bag. Ask your pharmacist to check for interactions. If you’re hospitalized, make sure your medication list is reviewed before discharge. Studies show these steps reduce errors by up to 80%.
Are non-hormonal treatments effective for hot flashes?
Yes. SSRIs like paroxetine and escitalopram reduce hot flash frequency by 50-60%. Gabapentin and clonidine also help. Cognitive behavioral therapy and hypnosis have shown strong results in clinical trials. Lifestyle changes-cooling your bedroom, avoiding alcohol and spicy foods, and practicing slow breathing-can reduce symptoms without drugs. These options are often safer than hormone therapy, especially for women with a history of breast cancer or blood clots.
What is deprescribing, and why is it important?
Deprescribing means safely stopping medications that are no longer needed or are doing more harm than good. Many older adults take drugs that were prescribed years ago for conditions that have changed or resolved. These can cause side effects, interactions, or falls. Studies show structured deprescribing reduces the number of medications by 1.4 per person and cuts adverse drug events by 33%. It requires careful planning, gradual tapering, and regular follow-up-but it can greatly improve quality of life.



Gregory Parschauer - 15 January 2026
Let me just say this: if you’re still taking oral estrogen like it’s 2001, you’re not just outdated-you’re a walking liability. Transdermal is the only ethical choice for women over 55. The liver doesn’t care about your convenience. It’s not a suggestion-it’s a biological imperative. And don’t even get me started on NSAIDs. Ibuprofen for ‘a little arthritis’? That’s not self-care, that’s slow-motion suicide with a side of GI bleed. The Beers Criteria isn’t a suggestion-it’s a warning label written in blood.
Vinaypriy Wane - 16 January 2026
I’ve been a pharmacist for 27 years, and I’ve seen too many women on 8+ meds, none of which were ever reviewed together. One woman came in with 14 prescriptions-three of them for the same condition, two were expired, and one was for a dog. We deprescribed five drugs in one visit. Her BP dropped, her cognition improved, and she cried because she hadn’t slept through the night in seven years. It’s not magic-it’s just listening. Please, bring your brown bag. Please.
Diana Campos Ortiz - 17 January 2026
My mom took benadryl for sleep for 15 years. She didn’t even realize it was making her foggy. When we switched her to CBT and a fan, she said she felt like herself again. I didn’t know non-hormonal options were this effective. I’m so glad I read this. Thank you for sharing the real stuff-not just the pharma ads.
Jesse Ibarra - 18 January 2026
Oh, so now we’re supposed to trust ‘guidelines’ written by bureaucrats who’ve never met a post-menopausal woman? Tell me, does the USPSTF have ovaries? No? Then why are they deciding what my body can handle? Estrogen patches are safer? Sure, if you’re a lab rat in a controlled trial. But real women? We have jobs, grandkids, and chronic pain. We need options-not dogma. And don’t get me started on SSRIs for hot flashes-those things turn you into a zombie with no libido. Thanks for the solution, Dr. Google.
Randall Little - 19 January 2026
So let me get this straight: the same pills that were deemed ‘safe’ in the 90s are now ‘dangerous’ because science advanced? Shocking. Meanwhile, the FDA still approves new statins with the same efficacy as a placebo but twice the cost. The real crisis isn’t polypharmacy-it’s pharmaceutical marketing. You think your doctor chose that pill because it was best? Nah. They got a free lunch and a branded pen. Ask them who funded the study. They’ll change the subject.
Acacia Hendrix - 20 January 2026
Pharmacogenomic-guided deprescribing is the future, and frankly, it’s long overdue. The CYP2D6 polymorphism prevalence in post-menopausal women is significantly correlated with differential metabolizer phenotypes-yet we still default to empirical dosing. The START/STOPP criteria are merely the tip of the iceberg. We need AI-driven, longitudinal pharmacovigilance platforms integrated with EHRs to mitigate iatrogenic harm. Until then, we’re just rearranging deck chairs on the Titanic.
Adam Rivera - 21 January 2026
My aunt just turned 70 and she’s on six meds. She started asking questions like you said-and now she’s down to three. She says she feels like she’s 55 again. I told her to keep a journal of how she feels after each med change. She’s now teaching her book club about deprescribing. We need more of this. Not just for us-but for our moms, our aunts, our sisters. Thank you for giving us the words to talk about it.
John Tran - 21 January 2026
You know, I’ve been thinking about this whole thing like a metaphysical paradox-our bodies are these intricate, evolving ecosystems, and we treat them like machines that need new parts every five years. But menopause isn’t a malfunction-it’s a transition. A cosmic recalibration. And yet we rush to chemically silence the symptoms instead of listening to what the body is trying to say. We’re medicating away the wisdom of aging. The pill is a symbol of our fear of mortality. And every time we pop another one without questioning it, we’re just feeding the machine that wants us to believe we can outsmart death with a prescription pad. It’s not just about drugs-it’s about surrender. And maybe… maybe the bravest thing we can do is stop taking something.
mike swinchoski - 23 January 2026
You’re all overthinking this. Just stop the bad pills. Done.