Every year, people in hospitals and pharmacies across the world get the wrong medicine-not because of a mistake in dosage, but because two drugs look or sound almost exactly the same. These are called look-alike, sound-alike (LASA) medications, and they’re one of the most dangerous, yet under-discussed, causes of preventable harm in healthcare.
What Exactly Are LASA Medications?
LASA errors happen when two or more drugs have names that are visually or phonetically similar. It’s not just about spelling. It’s about how they’re written, how they’re said, how they’re packaged, and even how the pills look. Take HYDROmorphone and hYDROcodone. Both are opioids. One is for severe pain in hospitals. The other is for moderate pain at home. But if a nurse reads “hydro” quickly during a busy shift, or if a pharmacist grabs the wrong bottle off the shelf, the result could be a fatal overdose. That’s why the FDA requires tall man lettering-capitalizing the different parts of the name-to make the difference obvious. But even that doesn’t always work. Another dangerous pair: doxorubicin and daunorubicin. Both are chemotherapy drugs. One treats leukemia. The other treats breast cancer. Mix them up, and you’re not just giving the wrong treatment-you’re potentially killing the patient. A 2022 study in Pharmacy Practice found that over 64% of LASA errors came from drug names alone. Packaging and pill appearance made up another third. Even small differences matter. Simvastatin 10 mg and simvastatin 20 mg caused confusion so often, they were the most frequently reported LASA pair in the study.Where Do These Errors Happen?
You might think errors happen mostly in pharmacies. But they happen everywhere. - Prescribing: 24% of errors start here. A doctor says “synthroid” during a phone order. The pharmacist hears “levothyroxine.” Same drug, right? Actually, no-synthroid is a brand, levothyroxine is the generic. But they’re often used interchangeably, and if the provider doesn’t specify, the wrong one gets dispensed. - Dispensing: Pharmacists juggle hundreds of pills a day. In high-pressure moments, especially during shift changes, a bottle that looks like another can slip through. One nurse on Reddit shared how she almost gave levoTHYroxine instead of SYNTHROID during a night shift because both vials looked identical. - Administration: This is the biggest problem area. 68% of LASA errors happen when the medicine is being given to the patient. Nurses rushing between rooms, interrupted by alarms, distracted by paperwork-these are the moments when names blur. A ICU nurse recounted nearly giving vecuronium (a paralytic) instead of versed (a sedative). “Thank god I caught it,” she wrote. And the stakes? Sky-high. The American Society of Health-System Pharmacists says LASA errors most often involve high-alert medications: insulin, opioids, anticoagulants, chemotherapy, and neuromuscular blockers. One wrong dose can mean brain damage, cardiac arrest, or death.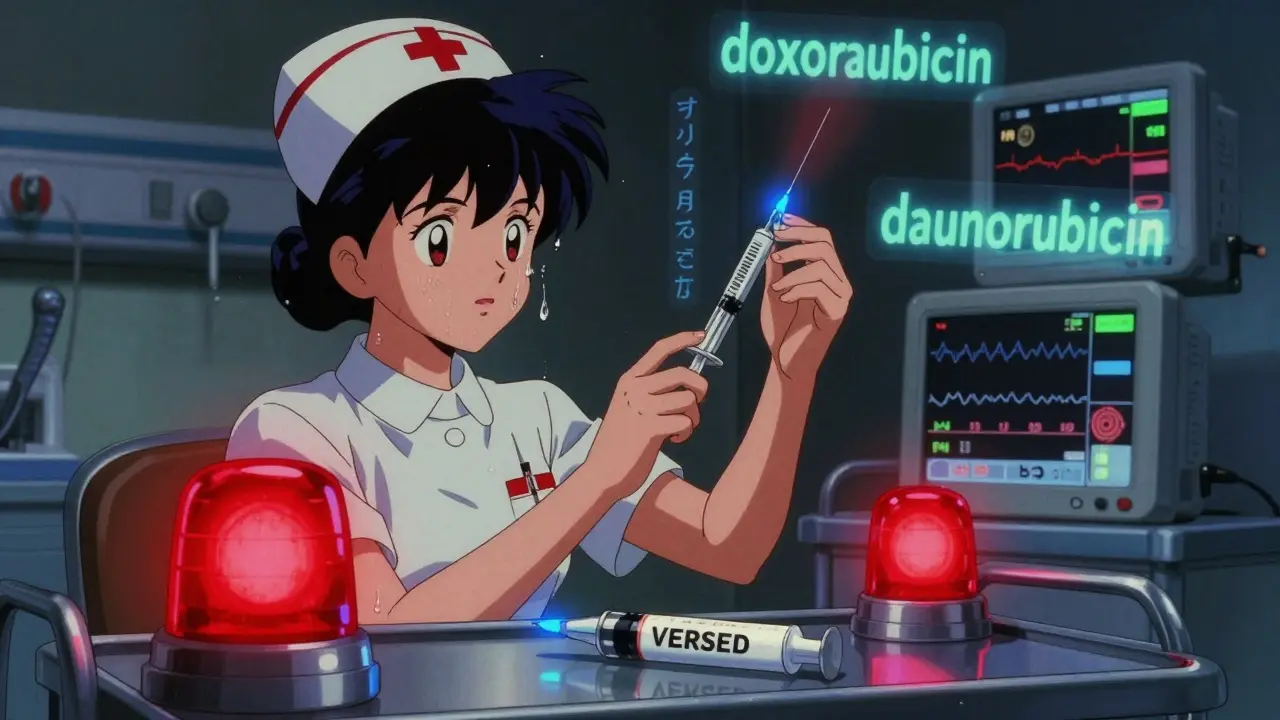
Why Is This Still Happening?
You’d think after 20 years of warnings, this would be fixed. But it’s not. The FDA has been using tall man lettering since 2001. Over 200 drug pairs now have capitalized letters to highlight differences: cisPLATIN vs. caraPLATIN, clonIDINE vs. clonIDINE (yes, even that one). But research shows it’s only marginally effective. Why? Because if staff don’t know why the letters are capitalized-or if they’re used to seeing the names in lowercase-they just glance over them. A 2022 review in the Journal of Pharmacy Practice and Pharmaceutical Sciences called tall man lettering a “quasi-placebo effect.” It gives the illusion of safety without real protection. The real issue? Drug names aren’t designed with safety in mind. When pharmaceutical companies apply for new drug names, they’re focused on branding, trademarks, and marketability-not on how easily they can be confused with existing drugs. The FDA denied 34 new drug names in 2022 because they were too similar to others. That’s up from 22 in 2018. But hundreds more slip through every year. Dr. Michael Cohen of ISMP put it bluntly: “The rate of name-confusion errors might be reduced if new and confusing names were not allowed on the market.”What’s Being Done to Stop It?
Some hospitals are fighting back-with real results. - Custom LASA Lists: The Joint Commission requires hospitals to create their own list of high-risk drug pairs based on what they actually use. No one-size-fits-all list works. A rural clinic won’t use the same chemo drugs as a big city hospital. - Electronic Alerts: Epic and Cerner, two major electronic health record systems, now flag LASA pairs during prescribing. Epic’s SafeMed module cut name-confusion errors by 28.7% in a 12-hospital study. - AI Voice Recognition: The AHRQ is funding a $4.7 million project at Johns Hopkins to test AI that listens to verbal orders and flags potential LASA mix-ups in real time. Early results show 89.3% accuracy. - Staff Training: High-risk departments like oncology and ICUs now require quarterly LASA training. Regular refreshers help. But in under-resourced hospitals, training is often skipped. The WHO and ISMP both say: this isn’t about blaming individuals. It’s about fixing the system. If a drug name is confusing, the system should stop it before it gets to the patient.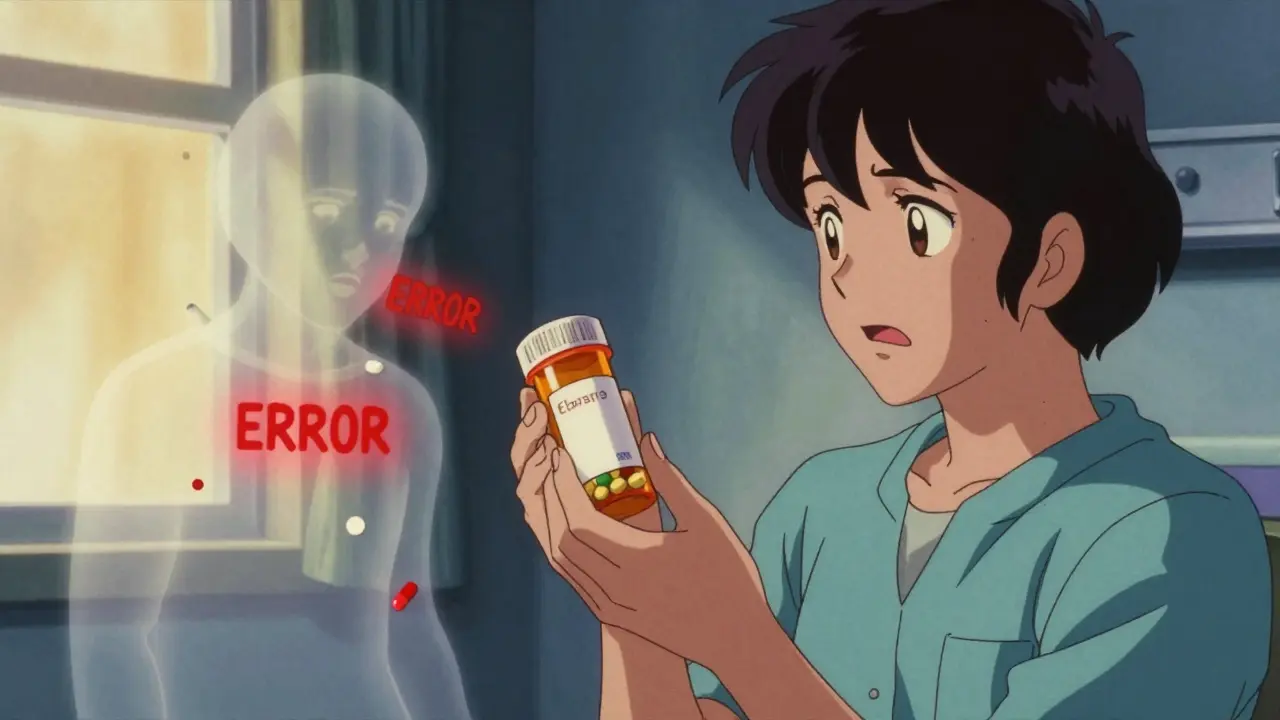
What You Can Do
If you or a loved one is on medication, here’s how to protect yourself:- Always ask: “Is this the generic or brand name?” Don’t assume they’re interchangeable.
- Check the pill: Does it look different from your last prescription? Even a slight color or shape change matters.
- Read the label: Is the strength clearly written? Is it printed or handwritten?
- Speak up: If a nurse says, “I’m giving you your thyroid med,” ask: “Is that levothyroxine or Synthroid?”
- Keep a list: Write down all your meds-name, strength, and why you take them. Bring it to every appointment.
The Bigger Picture
This isn’t just a pharmacy problem. It’s a global public health issue. Between 2018 and 2022, the FDA’s MAUDE database recorded at least 128 deaths linked directly to LASA errors. That’s not a statistic-it’s 128 families who lost someone because two drug names looked too similar. The global market for medication safety tech is expected to hit $6.8 billion by 2027. That’s because hospitals and regulators are finally realizing: you can’t rely on humans to catch what machines should prevent. The International Pharmaceutical Federation is pushing for universal design standards for drug names and packaging by 2030. That means future drugs won’t just be tested for effectiveness-they’ll be tested for safety from the moment they’re named. As Dr. Donald Berwick wrote in the New England Journal of Medicine, “While LASA errors can never be eliminated entirely, a systematic approach combining regulatory oversight, technological solutions, and human-centered design could reduce their incidence by 80% within a decade.” We’re not there yet. But we’re moving in the right direction-if we keep pushing for change.What are some common look-alike, sound-alike drug pairs?
Some of the most dangerous pairs include: HYDROmorphone and hYDROcodone (both opioids), doxorubicin and daunorubicin (chemotherapy drugs), levoTHYroxine and SYNTHROID (thyroid meds), vecuronium and versed (ICU drugs), and melphalan and meloxicam (cancer and pain meds). Even small differences in spelling or pronunciation can lead to deadly mix-ups.
How common are LASA medication errors?
About one in four medication errors in the U.S. is caused by drug name confusion, according to Medscape and the Anesthesia Patient Safety Foundation. A 2022 study found that drug name confusion alone accounted for 64.62% of all LASA errors. These mistakes happen in hospitals, clinics, and even at home when prescriptions are filled.
Does tall man lettering actually prevent errors?
It helps-but not as much as people think. Tall man lettering (like HYDROmorphone vs. hYDROcodone) was introduced by the FDA in 2001. Studies show it only reduces errors slightly. Many healthcare workers don’t notice the capitalization, or they’ve become used to ignoring it. It’s a visual cue, not a solution. Real prevention needs technology, training, and smarter drug naming.
Why don’t drug companies pick safer names?
Drug names are chosen for marketing, not safety. Companies want names that are catchy, easy to remember, and trademarkable. Safety isn’t a priority in the approval process. The FDA has started rejecting names that are too similar to existing ones-34 were denied in 2022-but many confusing names still get approved. Experts say new drugs should be tested for name confusion before they reach the market.
Can patients help prevent these errors?
Absolutely. Always ask: “Is this the brand or generic name?” Check the pill’s color and shape against your last prescription. Don’t let staff assume you know what you’re getting. If you’re told you’re getting “thyroid medicine,” ask for the exact name. Your awareness can be the last line of defense.





Skye Kooyman - 26 January 2026
I work in a pharmacy and this is real. One time I almost gave someone hydromorphone instead of hydrocodone. Thank god I double-checked the script. Scary stuff.
Peter Sharplin - 26 January 2026
Tall man lettering is a band-aid. The real fix is redesigning how drugs are named from the ground up. Pharma companies prioritize branding over safety, and the FDA lets it slide. We need mandatory confusion testing before approval - like crash tests for drugs.
Betty Bomber - 27 January 2026
My aunt got the wrong chemo drug last year. She’s fine now but the hospital never even apologized. Just said 'it happens.'
Mohammed Rizvi - 29 January 2026
So let me get this straight - we let corporations name life-or-death chemicals like they’re selling energy drinks? 'Doxorubicin' sounds like a villain in a Marvel movie. Meanwhile, people are dying because someone misread a word that looks like a typo. This isn’t healthcare. It’s a horror show with a bureaucracy.
eric fert - 30 January 2026
You know what’s really dangerous? People thinking this is a 'systemic issue.' Nah. It’s lazy. Nurses don’t pay attention. Pharmacists don’t care. Doctors dictate too fast. If you’re too busy to read the damn label, maybe you shouldn’t be handling pills. This isn’t rocket science - it’s basic human responsibility. Stop blaming the system and start blaming the people who keep screwing up.
Shawn Raja - 30 January 2026
This is capitalism in action. We don’t design drugs for safety - we design them for profit. A name that sounds like 'victory' or 'zen' sells better than 'HYDROmorphone.' The FDA’s job is to protect us, but they’re too busy kissing pharma’s butt. Until we treat drug names like nuclear codes, not marketing slogans, people will keep dying. And we’ll keep pretending it’s not our fault.
Allie Lehto - 31 January 2026
I’ve been saying this for years!!! People just don’t CARE!! 😔 I mean, if you can’t even read a label right, why are you even in healthcare?? I’m not even mad, I’m just disappointed... 🤦♀️ We need mandatory drug name flashcards for every nurse!! #WakeUp
Nicholas Miter - 1 February 2026
I’ve seen this firsthand in rural ERs. No AI, no alerts, no training. Just a nurse with 3 patients, 2 alarms going off, and a stack of scripts. I’ve watched them grab the wrong vial and not even blink. The tech exists - Epic, Cerner, AI voice tools - but half the hospitals can’t afford it. This isn’t about laziness. It’s about inequality in healthcare infrastructure.
Henry Jenkins - 1 February 2026
I’ve been thinking about this a lot. It’s not just the names - it’s the entire culture of speed over safety. We reward efficiency, not vigilance. A nurse who takes 30 extra seconds to verify a drug gets called 'slow.' A nurse who rushes and messes up gets blamed, but the system that pushed them to rush? Never questioned. We need to flip the script: reward caution, not speed. Maybe then we’ll see real change.
rasna saha - 2 February 2026
My mom is on levothyroxine and I always check the bottle. Even the color changes sometimes and I ask. I know it seems small but it saved her once. You don’t have to be a doctor to make a difference.
Dan Nichols - 2 February 2026
Tall man lettering is a joke. If you can’t tell the difference between doxorubicin and daunorubicin after 10 seconds of looking, you shouldn’t be licensed. This isn’t a design flaw - it’s a competency failure. And no, AI won’t fix stupid. Training will. Fix the people, not the labels.
Suresh Kumar Govindan - 4 February 2026
The root cause is the commodification of human life. Pharmaceutical conglomerates, operating under the guise of innovation, have systematically deprioritized nomenclatural integrity in favor of shareholder value. This is not an error - it is a structural atrocity.