Steroid-Induced Hyperglycemia Risk Calculator
This calculator estimates your risk of developing steroid-induced hyperglycemia based on factors discussed in the article. It helps you understand whether you should be monitoring your blood sugar while taking corticosteroids.
When you take corticosteroids like prednisone or dexamethasone for asthma, arthritis, or an autoimmune flare-up, your body doesn’t just fight inflammation-it also starts spiking your blood sugar. For many people, this isn’t just a side effect. It’s a full-blown metabolic crisis that can happen within days of starting treatment. Even if you’ve never had diabetes before, high-dose steroids can push your blood glucose into dangerous territory. And most patients don’t see it coming.
Why Corticosteroids Raise Blood Sugar
Corticosteroids don’t just cause high blood sugar-they actively rewire how your body handles glucose. It’s not a simple case of eating too much sugar. These drugs trigger a cascade of changes in your liver, muscles, fat, and pancreas that work together to flood your bloodstream with glucose.
In your liver, corticosteroids turn on the glucose factory. They ramp up gluconeogenesis-the process of making new glucose from scratch-by 35-40%. That means your liver is pumping out extra sugar even when you haven’t eaten. At the same time, they boost the effect of other stress hormones like glucagon and epinephrine, which also tell your liver to release more glucose.
In your muscles, insulin loses its grip. Normally, insulin opens the door for glucose to enter muscle cells for energy. But corticosteroids block that signal by interfering with GLUT4 transporters. Studies show this cuts glucose uptake by around 30%. Your muscles become insulin resistant, meaning they can’t soak up sugar like they used to.
Your fat tissue isn’t helping either. Corticosteroids increase lipolysis-the breakdown of fat-by 25-30%. This floods your blood with free fatty acids, which further block insulin signaling and make your cells even more resistant. The result? More sugar in your blood, less sugar getting used.
And then there’s your pancreas. Corticosteroids directly reduce insulin production by 20-35%. They lower the expression of GLUT2 and glucokinase, two key proteins your beta cells need to sense glucose and release insulin. At the same time, the extra fatty acids from fat breakdown poison the beta cells, leading to long-term damage. So you’re stuck with rising blood sugar and falling insulin-a double hit.
Who’s Most at Risk?
Not everyone on steroids gets high blood sugar. But some people are far more likely to. The biggest red flags:
- Dose matters: Taking 7.5 mg or more of prednisone daily increases your risk 3.2 times. Every extra 5 mg raises risk by 18%.
- Drug potency: Dexamethasone is 6-8 times more likely to cause hyperglycemia than prednisone at the same anti-inflammatory dose.
- Duration: Risk climbs 12% per week after the first two weeks of treatment.
- Age: Over 50? Your risk jumps 3.1 times.
- Weight: BMI over 25? That’s a 2.5-fold increase.
- History: Previous gestational diabetes? Your risk skyrockets to 4.3 times higher.
- Kidney function: If your eGFR is below 60, your risk is nearly 4 times higher.
People with a family history of type 2 diabetes or those already prediabetic are especially vulnerable. But even healthy, young patients on high-dose steroids can develop steroid-induced diabetes. It’s not about being "unhealthy"-it’s about biology being overwhelmed.
What Does It Feel Like?
Many patients don’t realize their blood sugar is soaring until they’re hospitalized. About 40% of cases show no symptoms at all. But when signs do appear, they’re easy to miss because they look like regular steroid side effects.
- Thirst and frequent urination: 65% and 72% of symptomatic patients report these-classic signs of high glucose pulling water out of your body.
- Extreme fatigue: 81% of patients feel unusually tired, even after rest.
- Blurred vision: High sugar swells the lens of your eye, making focus hard. Happens in 32% of cases.
- Increased hunger: 85% of steroid users report this-but it’s not hunger for food. It’s your body screaming for energy because cells can’t use glucose.
- Mood swings: 67% report irritability or anxiety. This isn’t just stress-it’s your brain reacting to unstable glucose levels.
And here’s the cruel twist: weight gain from steroids (2.5-4 kg in the first month) gets mistaken for just another side effect. But it’s often visceral fat building up because of insulin resistance. Your body is storing fat instead of burning fuel.
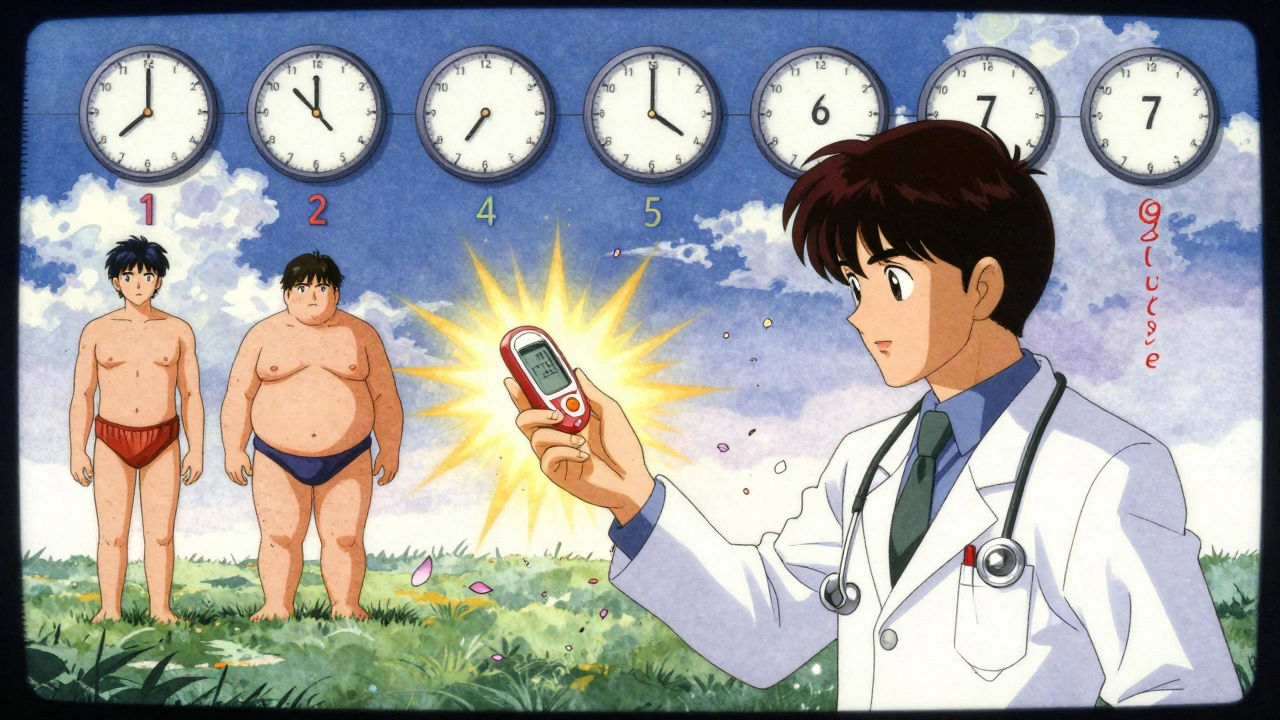
How Doctors Monitor and Diagnose It
There’s no single test for steroid-induced diabetes. Diagnosis relies on timing, dose, and glucose readings. The NIH recommends checking blood sugar at least twice daily for anyone on prednisone 20 mg or higher. For dexamethasone or other potent steroids, monitoring should start immediately.
Doctors look for:
- Fasting glucose over 140 mg/dL (7.8 mmol/L)
- Random glucose over 180 mg/dL (10.0 mmol/L)
- HbA1c rising rapidly during treatment (even if it was normal before)
But here’s the problem: most primary care providers don’t screen unless symptoms appear. A 2022 audit found that 35% of patients on long-term steroids never got their blood sugar checked. That’s dangerous. Hyperglycemia can escalate fast-leading to hyperosmolar hyperglycemic state (HHS) in 4-8% of severe cases, with a 15-20% mortality rate.
Patients who report delayed diagnosis often wait 9.3 days from first symptoms to confirmation. By then, they’re already in crisis.
How to Manage Steroid-Induced Hyperglycemia
Management isn’t about diet and exercise alone. You need targeted medical intervention.
Insulin is the gold standard. Unlike oral meds, insulin works regardless of insulin resistance. The UCSF protocol recommends:
- Basal insulin: Increase by 20% for every 10 mg above 20 mg of prednisone daily.
- Mealtime insulin: Use a 1 unit per 5-10g carb ratio.
For example, someone on 40 mg prednisone would need about 40% more basal insulin than their usual dose. Timing matters too-steroids peak 4-8 hours after ingestion, so glucose should be checked 6 hours after the morning dose.
Oral meds? Proceed with caution. Sulfonylureas like glipizide can help by forcing the pancreas to release more insulin. But they’re risky. When steroids are tapered, insulin production doesn’t bounce back immediately. That creates a dangerous mismatch-medication still active, but less sugar to clear. This leads to hypoglycemia in 37% of cases if not adjusted.
GLP-1 receptor agonists (like semaglutide) are being studied in the NIH’s GLUCO-STER trial. Early results show 28% lower hypoglycemia risk compared to insulin. But they’re not yet standard for short-term use.
For patients with pre-existing type 2 diabetes, insulin needs often jump 50-100% during steroid treatment. Many don’t realize this until they’re in the ER.
What Happens When You Stop Steroids?
Good news: steroid-induced diabetes is usually temporary. Blood sugar typically normalizes within 3-5 days after stopping the drug. But here’s where things go wrong:
- Many patients keep taking diabetes meds out of habit.
- Doctors don’t always tell them to stop.
- Some patients are told they "have diabetes now"-even if it was only steroid-triggered.
One Reddit user, who took prednisone for a lupus flare, said her doctor prescribed metformin and never followed up. Three months later, she was still on it. Her blood sugar was normal. She had no symptoms. But she was taking a drug she didn’t need.
That’s why education matters. Patients need clear instructions: "When you finish your steroids, check your blood sugar daily for a week. If it’s under 100 mg/dL fasting and under 140 mg/dL after meals, you likely don’t need meds anymore. Call your doctor to confirm."
The Bigger Picture
Corticosteroids are essential. Millions rely on them. But their metabolic cost is underrecognized. About 1-2% of the population takes systemic steroids each year. For those over 65, it’s 8-10%. That’s millions of people at risk.
Hospitalized patients on high-dose steroids have a 45-60% chance of needing glucose control. That adds 2.3 extra days in the hospital and $2,800-$4,200 in costs per admission. Primary care is failing to catch cases early. The FDA has required hyperglycemia warnings on labels since 2018, but that doesn’t change practice.
Emerging therapies are making this worse. CAR-T cancer treatments now commonly include steroids, and 75-85% of those patients develop hyperglycemia. New autoimmune treatments are increasing steroid use. The Endocrine Society predicts steroid-induced diabetes will be the third most common cause of secondary diabetes by 2030.
But there’s hope. The European Association for the Study of Diabetes launched the STEROID-Glucose app in 2023. It gives real-time insulin dose suggestions based on steroid type and glucose readings. Pilot studies showed a 32% drop in high-blood-sugar events.
And researchers are developing new steroids-tissue-selective glucocorticoid receptor modulators-that fight inflammation without wrecking glucose control. Compound XG-201, in phase II trials, reduced hyperglycemia by 65% compared to prednisone at the same dose.
Until those drugs are available, the best defense is awareness. If you’re on steroids, ask: "Will this affect my blood sugar? Should I be checking it? What should I do if it goes high?" Don’t wait for symptoms. Don’t assume it’s just fatigue or hunger. Ask for a glucose monitor. It could save your life.
Can corticosteroids cause diabetes in someone who never had it before?
Yes. Corticosteroids can trigger steroid-induced diabetes in people with no prior history. This happens in 10-30% of patients on high-dose therapy. It’s not true type 2 diabetes-it’s a temporary metabolic disruption caused by the drug’s effect on insulin resistance, liver glucose production, and pancreatic function. Blood sugar usually returns to normal within days of stopping the steroid, but it can be dangerous if untreated.
How long does it take for steroids to raise blood sugar?
Blood sugar can rise within 24-48 hours of starting high-dose corticosteroids. The peak effect typically occurs 4-8 hours after the morning dose, especially with prednisone. For longer-acting steroids like dexamethasone, the rise may be slower but more sustained. Monitoring should begin immediately when starting therapy, not after symptoms appear.
Is insulin the only treatment for steroid-induced hyperglycemia?
Insulin is the most effective and safest option, especially for moderate to severe cases. Oral medications like sulfonylureas can be used but carry a high risk of hypoglycemia when steroids are tapered. GLP-1 agonists are being studied and show promise for lower hypoglycemia risk, but they’re not yet standard. Diet and exercise alone won’t reverse steroid-induced insulin resistance-it requires medical intervention.
Will I need to take diabetes medication forever if I develop high blood sugar from steroids?
No. Steroid-induced hyperglycemia is usually temporary. Blood sugar levels typically return to normal within 3-5 days after stopping the steroid. Many patients are mistakenly kept on diabetes meds long after the steroid is gone. Always check your blood sugar after finishing steroids and consult your doctor before continuing any diabetes medication.
What’s the difference between steroid-induced diabetes and type 2 diabetes?
Steroid-induced diabetes is caused by a drug’s direct interference with glucose metabolism-it’s not due to long-term insulin resistance from obesity or genetics. It often develops quickly, reverses after stopping the drug, and doesn’t always involve weight gain or metabolic syndrome. Type 2 diabetes is chronic and progressive. While steroid-induced diabetes can unmask underlying prediabetes, it’s a distinct condition requiring different management and follow-up.
How can I prevent high blood sugar while taking steroids?
Ask your doctor for a glucometer before starting steroids, especially if you’re on 7.5 mg or more of prednisone daily. Monitor fasting and post-meal glucose twice daily. Avoid high-carb meals during peak steroid action (4-8 hours after your dose). Stay hydrated. Don’t assume fatigue or thirst is just a side effect-check your numbers. Early detection prevents complications like HHS or DKA.



iswarya bala - 8 December 2025
omg i just started prednisone last week and thought i was going crazy with all the thirst and tiredness 😭 turns out my body was just screaming for help. got a glucometer today and my sugar was 210 after breakfast. i feel seen.
om guru - 10 December 2025
Proper monitoring of blood glucose is essential during corticosteroid therapy. Failure to implement routine screening protocols increases the risk of hyperosmolar hyperglycemic state. Clinical guidelines are clear. Adherence is non-negotiable.
Jennifer Blandford - 11 December 2025
YOOOO I JUST HAD THE SAME THING HAPPEN TO ME LAST YEAR WHEN I WAS ON DEXAMETHASONE FOR MY LUPUS FLARE 🤯 I thought I was just "being lazy" but nooo my body was in full rebellion. I started checking my sugars like a maniac and my doc was like "oh wow you're lucky you caught it before you ended up in the hospital." Now I carry glucose strips everywhere like my life depends on it... because it kinda does. Also I bought a cute little phone case that holds my meter and now I feel like a diabetes ninja. 💪🩸
Iris Carmen - 13 December 2025
i thought my blurry vision was just from staring at screens too long… turns out it was my blood sugar trying to kill me. got tested and it was 198. i cried in the parking lot. now i check it every morning. thank you for writing this.
Delaine Kiara - 14 December 2025
Let’s be real - this whole thing is a scam. Big Pharma doesn’t want you to know that sugar is the real villain, not steroids. You take steroids, your body gets confused, so you blame the drug? Nah. It’s the carbs. It’s always the carbs. If you just ate less bread and more kale, none of this would happen. Also, insulin? Please. That’s just a crutch for people who can’t discipline themselves. I’ve been on prednisone for six months and I’m fine because I do intermittent fasting and only drink water with lemon. #NoSugarNoProblem
Katherine Rodgers - 14 December 2025
Oh sweet jesus another post about how steroids "make you diabetic" like this is news. You mean the same drugs that cause moon face, buffalo hump, and insomnia also make your blood sugar go full volcano? Shocking. And yet, doctors still hand these out like candy. I’ve seen patients on 60mg of prednisone for years and nobody checks their glucose until they’re in the ER with a glucose level of 800. Congrats, you just got diagnosed with diabetes… by accident. Thanks for the life-threatening negligence, healthcare system.
Darcie Streeter-Oxland - 15 December 2025
It is regrettable that the clinical management of steroid-induced hyperglycaemia remains inconsistent across primary care settings. The absence of standardized monitoring protocols constitutes a systemic failure in preventive medicine. Further research is warranted, but immediate action requires institutional policy change.
Mona Schmidt - 16 December 2025
This is such an important post - thank you for breaking it down so clearly. I work with older patients on long-term steroids and so many don’t realize their fatigue and thirst aren’t just "aging" or "side effects." I now hand out glucometers on the first visit if they’re on more than 7.5mg prednisone. One woman, 72, said she thought her constant urination was just "getting old." She didn’t know her kidneys were trying to flush out sugar. We caught her early. She’s doing great now. Small changes save lives.
Guylaine Lapointe - 17 December 2025
It’s infuriating that this isn’t common knowledge. People are dying from this and no one talks about it. My cousin was prescribed prednisone for a rash - one week later, she was in the ICU with HHS. They told her she had type 2 diabetes. She’s still on metformin. Her sugars are normal now. She’s been told to stop meds, but her doctor never followed up. This isn’t just medical negligence - it’s criminal. Someone needs to sue someone.
Courtney Black - 18 December 2025
Think about it: steroids are synthetic stress hormones. Your body was never meant to live in a constant state of fight-or-flight. When you flood your system with cortisol analogs, you’re not just raising blood sugar - you’re hijacking your entire metabolic identity. The liver becomes a sugar factory, the muscles turn into locked vaults, the pancreas is silenced. It’s not diabetes. It’s a biological mutiny. And the real tragedy? We treat the symptom - glucose - instead of asking why we’re forcing the body into this unnatural state in the first place. Maybe the question isn’t how to manage the sugar… but why we’re giving the drug at all. Is the inflammation worth this cost? That’s the real diagnosis.