Why Your Eczema Won’t Go Away
Most people think eczema is just dry, itchy skin. But if you’ve had it for months or years, you know it’s more than that. It’s the sleepless nights from scratching. The red, cracked patches that won’t heal. The frustration when your favorite lotion stops working. The truth? Chronic eczema isn’t just a rash-it’s a broken skin barrier. And until you fix that, nothing else will stick.
Research from 2025 shows that over 15% of kids and 2% of adults live with this condition, and the numbers are climbing. But here’s what most doctors don’t tell you: the inflammation and itching? They’re symptoms. The real problem is the barrier-the outer layer of your skin-that’s been damaged for months, maybe years. When that barrier cracks, water escapes, germs get in, and your immune system goes into overdrive. That’s when the itching starts. And once the itch-scratch cycle begins, it’s hard to break.
How Your Skin Barrier Actually Works
Your skin isn’t just a surface. It’s a layered fortress. Think of it like a brick wall: the bricks are dead skin cells (corneocytes), and the mortar is made of lipids-ceramides, cholesterol, and fatty acids. These lipids hold everything together and keep moisture in. In healthy skin, this layer is tight and smooth. In chronic eczema? It’s full of holes.
Studies show people with moderate to severe eczema have 30-50% less ceramide than normal skin. Ceramide 1, the most important one, is often missing entirely. That’s why your skin feels tight, flaky, and burns when you apply anything. On top of that, the skin’s natural pH-usually around 5-is often raised to 7 or higher. That throws off enzymes that should be repairing the barrier. And then there’s the microbiome. Healthy skin hosts good bacteria. Eczema skin? It’s overrun by Staphylococcus aureus, a germ that makes inflammation worse.
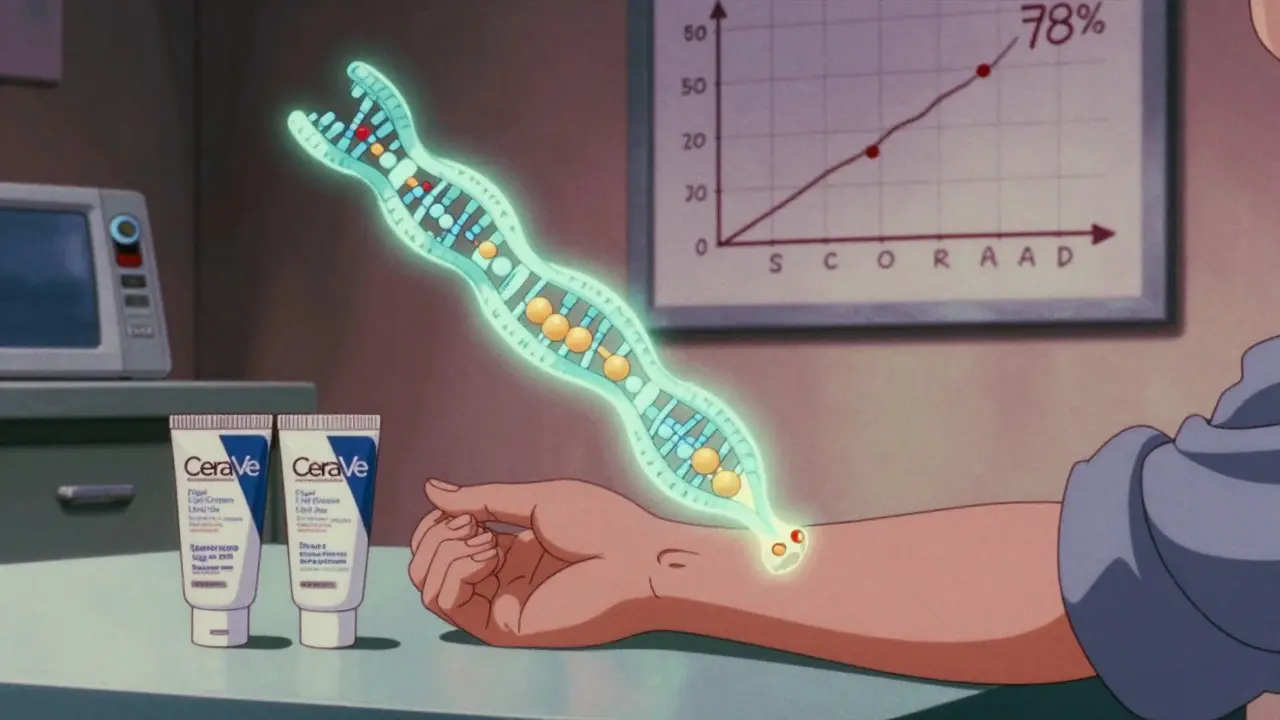
This isn’t random. Half of all severe eczema cases are linked to mutations in the FLG gene, which controls filaggrin-a protein that helps form the skin’s natural barrier. If you have this mutation, your skin just doesn’t make enough of the right lipids. That’s why moisturizers with just petrolatum or glycerin often fail. They hydrate, but they don’t rebuild.
Barrier Repair: The Only Treatment That Works Long-Term
Forget steroids for a second. The most powerful tool you have is barrier repair. Not just any moisturizer-specifically formulated products with the right mix of lipids: ceramides, cholesterol, and free fatty acids in a 1:1:1 ratio. That’s the exact blend your skin naturally makes. When you apply it, you’re not just adding moisture-you’re replacing what’s missing.
Double-blind trials show these products reduce water loss from skin (TEWL) by 40-50% in just two weeks. That’s not a guess. That’s measurable. One study found 87% of users saw real barrier improvement with this formula, compared to only 52% with regular lotions. In another, patients using ceramide-rich creams saw a 78% drop in their SCORAD score (a standard eczema severity measure) after four weeks. Those using basic moisturizers? Only 45% improvement.
Brands like CeraVe, EpiCeram, and Vanicream have these ratios built in. You’ll see them labeled as “ceramide-dominant” or “physiologic lipid therapy.” Avoid anything that just says “hydrating” or “for dry skin.” Those are marketing terms. Look for ceramides, cholesterol, and fatty acids on the ingredient list. If they’re not in the top five, it’s probably not strong enough.
And here’s the kicker: barrier repair reduces Staph colonization by 65-75%. That means fewer infections, less redness, and less itching. It’s not magic. It’s science.

What Triggers Your Flares (And How to Avoid Them)
Even with perfect barrier repair, triggers can still set off a flare. The worst ones? Sweat, harsh soaps, stress, and dry air. But here’s what most people miss: your laundry detergent. Fragrance, dyes, and optical brighteners in detergent can linger on clothes and irritate sensitive skin. Switch to fragrance-free, dye-free detergents like All Free & Clear or Tide Free & Gentle. Wash new clothes before wearing them.
Hot showers are another silent trigger. Heat strips away natural oils and dries out the skin. Keep showers under 10 minutes, and use lukewarm water-not hot. Skip the loofah. Use your hands to gently cleanse with a soap-free cleanser like Cetaphil Gentle Cleanser or Vanicream Cleansing Bar. Pat dry, don’t rub.
Environmental triggers matter too. Cold, dry winter air is brutal. Indoor heating dries things out even more. Use a humidifier in your bedroom. Keep it at 40-50% humidity. If you live in a dry climate, consider a whole-house humidifier.
And yes, stress plays a role. When you’re stressed, your body releases cortisol, which weakens the skin barrier and boosts inflammation. You don’t need to eliminate stress. Just manage it. Ten minutes of deep breathing, a walk outside, or even listening to music can help. It’s not just mental-it’s physical.
How to Stop the Itch Without Scratching
The itch is the worst part. It’s not just annoying-it’s exhausting. And scratching makes everything worse. It tears the barrier even more, opens the door to infection, and rewires your brain to crave more scratching. It becomes a habit.
Here’s what actually works:
- Apply cold immediately. Keep a damp washcloth or ice pack wrapped in a towel in the fridge. When the itch hits, press it on the area for 30 seconds. Cold blocks the itch signal to your brain.
- Tap, don’t scratch. Use your fingertips to gently tap the area. It distracts your nervous system without damaging skin.
- Wear cotton gloves at night. If you scratch in your sleep, this is non-negotiable. Keep them clean and change them daily.
- Use topical pramoxine. This is a non-steroidal itch relief ingredient found in products like Sarna Sensitive. It numbs the nerve endings locally without affecting your skin’s barrier.
- Try wet wrap therapy. After applying your barrier cream, dampen cotton pajamas or sleeves, then put them on over the cream. Cover with dry cotton. Leave on for 2-4 hours or overnight. This traps moisture and calms inflammation. Studies show it reduces itch by up to 70%.
Some people swear by antihistamines like cetirizine or loratadine for nighttime itch. But the science is mixed. They help with allergy-related itching, but not always eczema-related. Talk to your doctor before using them long-term.
When Barrier Repair Isn’t Enough
Here’s the hard truth: 30-40% of people with severe eczema don’t get full relief from barrier repair alone. That’s not your fault. If you have a strong FLG mutation, your skin might never make enough ceramides, no matter how much you apply. In those cases, you need help from your immune system.
Topical calcineurin inhibitors like pimecrolimus (Elidel) or tacrolimus (Protopic) are steroid-free options that calm inflammation without thinning the skin. They take longer to work-about 2-4 weeks-but they’re safe for long-term use. For moderate to severe cases, newer options like crisaborole (Eucrisa) or JAK inhibitors like ruxolitinib cream (Opzelura) can be game-changers. They target the immune pathways that drive inflammation directly.
And if your eczema is really bad-covering large areas, disrupting sleep, or not responding to anything-systemic treatments like dupilumab (Dupixent) or tralokinumab (Adbry) may be options. These are injectables that block key inflammatory signals. They’re not a cure, but they can reduce flares by 70-80% in many patients.
Don’t wait until you’re desperate. Talk to a dermatologist who specializes in eczema. Ask about your filaggrin status. Ask about barrier repair compliance. Ask about next steps. You’re not failing. You just need a better plan.
How to Use Barrier Creams the Right Way
Applying moisturizer wrong is why most people give up. You don’t need more product. You need better technique.
Here’s the protocol:
- Apply within 3 minutes of bathing. Your skin is still damp. That’s when it absorbs moisture best. Waiting even 10 minutes cuts effectiveness by 35%.
- Use the right amount. For each arm, use about 5 grams-roughly the size of a golf ball or two fingertip units (the amount from the first joint to the tip of your finger). For the whole body, use 1-2 ounces per application.
- Apply twice daily. Morning and night. Don’t skip.
- Wait 15 minutes before applying steroids. If you’re using a prescription cream, apply your barrier repair first, wait 15 minutes, then apply the steroid. Applying them together reduces the steroid’s absorption.
- Don’t wash your hands after applying. Unless you’re going to touch your face or eyes. Your hands are now part of the treatment.
It takes time. Most people see improvement in 2-4 weeks. Full results take 6-8 weeks. If you stop after 10 days, you’re not giving it a chance. And if your cream stings at first? That’s normal. It’s not burning-it’s your skin reacting to the pH. That usually fades in 3-5 days.
Cost, Compliance, and Real-World Challenges
Let’s be honest: good barrier creams cost more. A 200g tube of CeraVe or EpiCeram runs $25-$30. Basic petroleum jelly? $10. But here’s the math: if you’re using steroids every week because your barrier isn’t fixed, you’re spending more in doctor visits, missed work, and side effects. Barrier repair reduces flare frequency by 40-60%. That’s fewer prescriptions, fewer ER visits, fewer sleepless nights.
Insurance often covers prescription barrier products like EpiCeram. Over-the-counter ones? Not so much. But some HSA/FSA plans let you use pre-tax dollars to buy them. Check with your provider.
And yes, texture is an issue. These creams are thicker. They feel greasy. But that’s the point. You’re not trying to make your skin feel “light.” You’re trying to rebuild it. If you hate the feel, try a lighter version like CeraVe Moisturizing Cream (not lotion) or Vanicream Lite. Or use a pump bottle to avoid contamination.
And don’t believe the myth that you can’t use these with steroids. You can. Just space them out by 15 minutes. That’s all.
What’s Next for Eczema Treatment
The future is personal. Companies are starting to test your DNA for FLG mutations and match you to the right barrier cream. One 2024 study showed AI could predict the best product for your skin with 85% accuracy. Imagine getting a recommendation based on your genetics, not your Instagram ad.
There’s also microbiome therapy-applying good bacteria to the skin to crowd out Staph. And platelet-rich plasma (PRP), which uses your own blood to stimulate healing. These are still in trials, but they’re coming.
One thing’s clear: barrier repair is no longer optional. The American Academy of Dermatology says it’s essential. The European Academy says it’s Level 1A evidence-the highest standard. And patients? They’re reporting 70% less nighttime scratching and flares dropping from weekly to monthly.
If you’ve been fighting eczema for years, you’re not alone. And you’re not broken. You just need the right tools. Start with barrier repair. Do it right. Give it time. And if it’s not enough? That’s not failure. That’s just the next step.




Emma ######### - 19 January 2026
Been dealing with this for 12 years. The ceramide-cholesterol-fatty acid 1:1:1 ratio was the only thing that finally stopped the nightly scratching. I used to go through three jars of cheap lotion a month. Now I use CeraVe once a day and my skin doesn’t feel like sandpaper anymore. It’s not glamorous, but it works.
Also, wet wraps at night changed my life. I know it sounds ridiculous, but I put on the cream, then damp cotton sleeves, then dry ones. I sleep like a baby now. No more red arms. No more guilt.
Don’t give up. It’s a grind, but it’s worth it.
christian Espinola - 19 January 2026
So you’re telling me the entire dermatology industry has been lying to us for decades? That the $200 billion skincare market is just selling water with a fancy label? And we’re supposed to believe that a $30 cream with three ingredients is the ‘only’ solution? Where’s the peer-reviewed meta-analysis on this? I’ve seen studies that contradict this exact claim.
Also, ‘physiologic lipid therapy’? That’s not a real term. It’s marketing jargon dressed up like science. I’m not buying it.
Nishant Sonuley - 20 January 2026
Man, I love how this post doesn’t just throw out ‘use moisturizer’ and call it a day. Most people think eczema is ‘just dry skin’ and go buy a $12 bottle of Aveeno. But this? This is the real deal. You’re not just hydrating-you’re rebuilding. Like fixing a crumbling brick wall with the exact same mortar it was built with.
And the part about laundry detergent? Holy crap. I didn’t realize my ‘fresh scent’ detergent was basically chemical warfare on my skin. Switched to Free & Clear last year. No more flare-ups after doing laundry. Who knew?
Also, the cold compress trick? Genius. I use an ice pack wrapped in a dish towel. It doesn’t kill the itch, but it makes it feel like someone else’s problem for a few minutes. That’s enough to break the cycle.
And yes, the creams feel greasy. So what? My skin isn’t a runway model. It’s a battlefield. Grease is armor.
Praseetha Pn - 22 January 2026
Okay but have you heard about the government’s secret plan to keep us all itchy? I read on a forum that the FDA allows Big Pharma to suppress ceramide research because steroid creams make more money. They don’t want you to heal. They want you to keep coming back. That’s why your insurance won’t cover EpiCeram but will pay for steroids every month.
And don’t even get me started on the 5G towers. I swear, my flare-ups get worse when I’m near cell towers. I live in a rural area now, no Wi-Fi, no smart meter. My skin hasn’t been this calm since 2018.
Also, I stopped using water. Just coconut oil and sunlight. Works better than anything. The dermatologists hate that I’m not taking their pills.
Robert Davis - 23 January 2026
I appreciate the science, but let’s be real-this is just another ‘miracle cure’ post from someone who hasn’t lived with this for 20 years. I’ve tried every ceramide cream on the market. I’ve done wet wraps, cold therapy, even tried putting Vaseline on my face at night. Nothing lasts. The FLG mutation? Yeah, I have it. My skin doesn’t care what ratio you mix. It just breaks.
And don’t tell me to ‘give it time.’ I’ve given it 15 years. The only thing that works is prednisone. And I’m not proud of it. But I’m not going to sit here and pretend a $30 cream is going to fix a genetic defect.
You’re not helping. You’re just selling hope.
Robert Cassidy - 25 January 2026
America is weak. We’ve been dumbed down by skincare influencers and ‘wellness culture.’ You think a cream fixes your skin? No. Your skin is weak because your lifestyle is weak. You sit inside all day, eat processed food, watch TikTok, and then blame your skin for being ‘broken.’
Go outside. Walk barefoot. Eat real food. Stop moisturizing like a baby. Your skin was made to handle dirt, sweat, and sun. Not this overpriced lab lotion nonsense.
My grandfather had eczema. He never used a cream. He used lard and salt. And he lived to 92. We’ve lost our way.
Kristin Dailey - 26 January 2026
Wet wraps work. Done.
Andrew McLarren - 26 January 2026
While I appreciate the empirical rigor of the data presented, I must respectfully note that the assertion regarding the 1:1:1 lipid ratio as a universal therapeutic standard may benefit from further contextualization. Individual phenotypic variance, particularly in patients with comorbid atopic dermatitis and immunoglobulin E dysregulation, may necessitate a more personalized approach to lipid supplementation. Furthermore, the economic accessibility of ceramide-dominant formulations remains a significant barrier for a substantial subset of the population. A holistic framework-encompassing environmental, behavioral, and pharmacological interventions-would be more clinically sustainable.
Chuck Dickson - 28 January 2026
Look. I was skeptical too. I thought this was just another ‘skin guru’ post. But I tried it. I used CeraVe every day, no skipping. I did the cold towel trick when I felt the itch. I switched detergents. I stopped hot showers.
Two months later? I went to the beach in shorts for the first time in 8 years. No red legs. No scratching. No shame.
This isn’t magic. It’s medicine. And it’s not easy. But if you do the work? It changes your life. You’re not broken. You just needed the right tools. Keep going. You got this.
Eric Gebeke - 30 January 2026
Everyone’s so obsessed with ‘barrier repair’ like it’s the holy grail. But what about the real cause? The mold in your walls. The glyphosate in your food. The EMF radiation from your phone. Your skin is screaming because your environment is poisoned. You’re treating the symptom, not the source.
I’ve seen people get better after they moved out of their apartment, switched to organic food, and started grounding. None of that is in this post. Because the pharmaceutical-industrial complex doesn’t want you to know that.