What Are Arrhythmias?
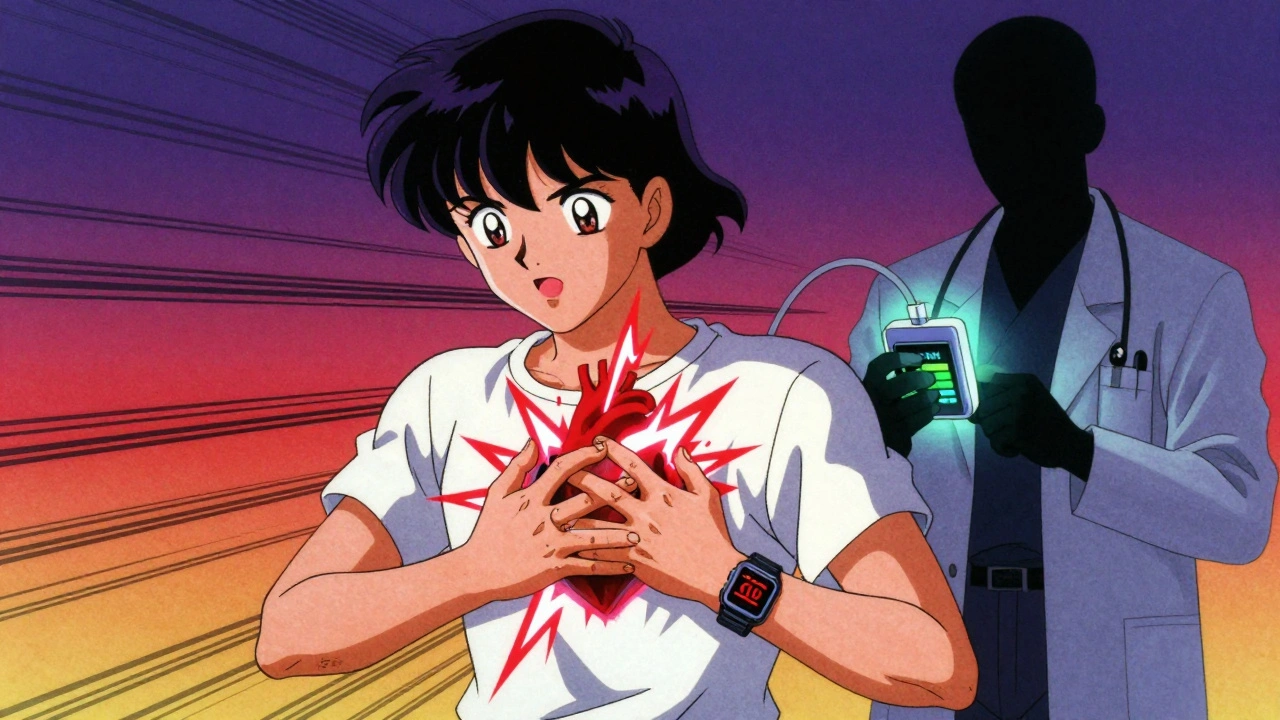
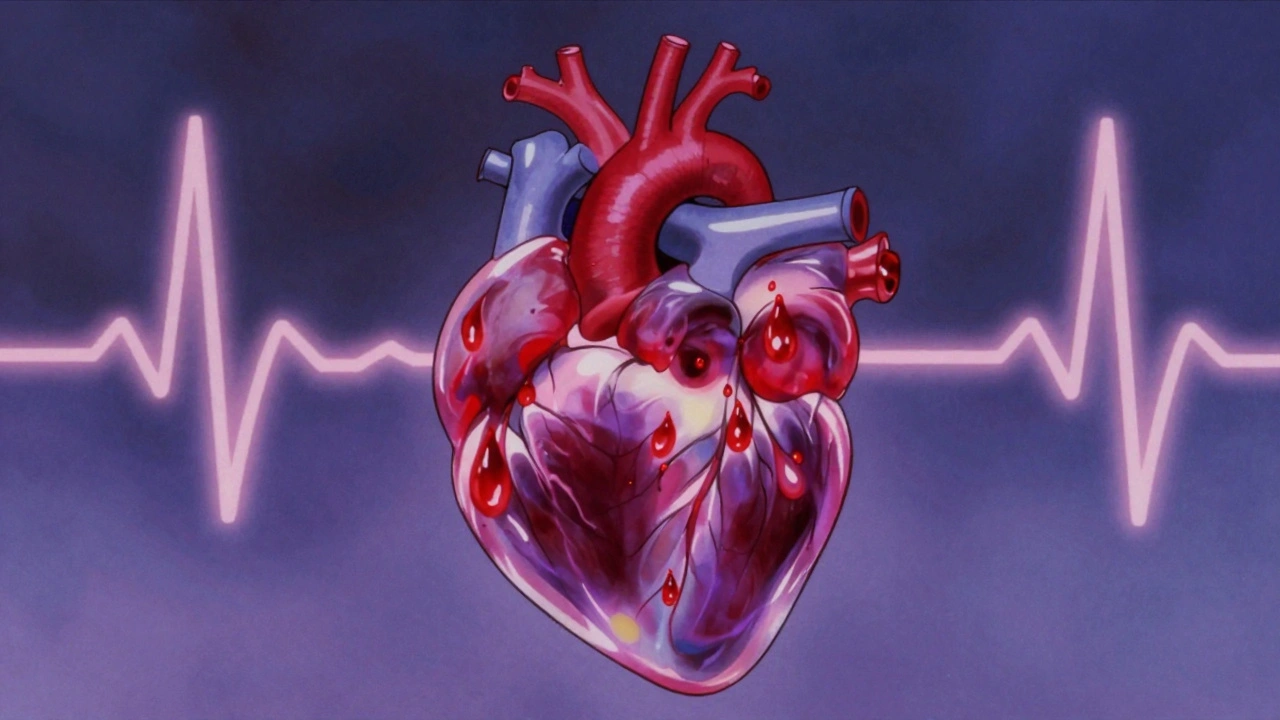
Your heart doesn’t just beat-it beats in rhythm. That rhythm keeps blood flowing to your brain, muscles, and organs. When that rhythm gets off track, you have an arrhythmia. It’s not always dangerous, but it can be a warning sign. The three most common types you’ll hear about are atrial fibrillation, bradycardia, and tachycardia. Each affects your heart differently, and knowing the difference matters.
Atrial Fibrillation: When Your Heart’s Upper Chambers Chaotic
Atrial fibrillation, or AFib, is the most common serious heart rhythm problem. Instead of beating in a steady pattern, the upper chambers of your heart (the atria) quiver or fibrillate. This means blood doesn’t pump out properly. It can pool, form clots, and lead to stroke. That’s why AFib increases stroke risk by five times, according to the American Heart Association.
Symptoms aren’t always obvious. Some people feel their heart fluttering, racing, or skipping beats. Others get tired easily, short of breath, or dizzy. But many have no symptoms at all-until they have a stroke. That’s why checking your pulse regularly is important. If it feels irregular, like a skipped beat followed by a thump, see your doctor.
Diagnosis starts with a simple ECG. It catches the chaotic pattern in real time. If episodes come and go, you might wear a portable monitor for 24 hours or longer. An echocardiogram checks if your heart structure is damaged. Blood tests look for thyroid issues or electrolyte imbalances that can trigger AFib.
Treatment isn’t one-size-fits-all. For most, the goal is to control the heart rate, not necessarily restore a normal rhythm. Medications like beta-blockers or calcium channel blockers slow the heart down. Blood thinners like warfarin or newer options like apixaban prevent clots. If meds don’t work or symptoms are bad, cardioversion-using electric shocks or drugs-can reset the rhythm. For recurring cases, cardiac ablation is an option. Newer techniques like pulsed field ablation use electrical pulses instead of heat or cold, reducing damage to nearby tissues.
Bradycardia: When Your Heart Beats Too Slow
Bradycardia means your heart beats slower than 60 times per minute. Sounds bad? Not always. Athletes often have slow resting hearts because their hearts are strong and efficient. But for others, it’s a problem.
If your heart beats too slowly, it can’t pump enough blood to your body. You might feel dizzy, faint, fatigued, or have trouble breathing during light activity. In severe cases, you could pass out or even go into heart failure.
Causes vary. It can come from aging, heart disease, or damage from a heart attack. Medications like beta-blockers can cause it too. Sometimes, the heart’s natural pacemaker-the sinoatrial node-just doesn’t fire right. Or signals from the upper chambers don’t reach the lower ones (called heart block).
Diagnosis is straightforward. A standard ECG will show the slow rhythm. If it’s intermittent, you might need a Holter monitor. Blood tests check for thyroid problems or high potassium. An exercise stress test can reveal if your heart can keep up when you’re active.
Treatment depends on the cause. If a medication is to blame, your doctor might adjust the dose. If it’s due to an underactive thyroid, treating that can fix the heart rate. But if the problem is in the heart’s wiring, you may need a pacemaker. Modern pacemakers are tiny, implanted under the skin, and adjust your heart rate based on your activity. They’re reliable, safe, and often life-changing.
Tachycardia: When Your Heart Races Out of Control
Tachycardia is when your heart beats faster than 100 beats per minute at rest. It’s not always a problem. Exercise, stress, or caffeine can make your heart race temporarily. But when it happens without reason-or lasts too long-it’s dangerous.
There are different types. Supraventricular tachycardia (SVT) starts in the upper chambers. Ventricular tachycardia (VT) starts in the lower chambers and is more serious. VT can lead to sudden cardiac arrest if not treated.
Symptoms include palpitations, chest pain, shortness of breath, lightheadedness, and fainting. In kids, parents might notice they’re unusually tired or avoid playing. In older adults, it can mimic a heart attack.
Diagnosis starts with an ECG. If the episode isn’t happening during the test, you’ll need a wearable monitor. An echocardiogram checks for structural problems. Blood tests look for anemia, infection, or thyroid issues.
Treatment varies. For SVT, simple maneuvers like the Valsalva maneuver (holding your breath and bearing down) can reset the rhythm. Medications like adenosine or beta-blockers can help. For recurring SVT, ablation is often curative. For VT, especially if you’ve had a heart attack, an implantable cardioverter-defibrillator (ICD) may be needed. It watches your heart and shocks it back to normal if it goes too fast.
What Triggers These Arrhythmias?
Many factors can set off an arrhythmia. High blood pressure is a big one-it strains the heart over time. Obesity increases the risk of AFib by up to 50%. Diabetes, sleep apnea, and excessive alcohol use are also major triggers. Even too much caffeine or energy drinks can cause temporary tachycardia.
Lifestyle changes aren’t just helpful-they’re essential. Losing even 10% of your body weight can reduce AFib episodes. Cutting back on alcohol helps. Quitting smoking lowers your risk of all arrhythmias. Regular, moderate exercise strengthens your heart without overloading it. Managing stress through breathing exercises or mindfulness can also calm erratic rhythms.
When to Worry
Not every skipped beat means trouble. Occasional palpitations are common. But if you notice:
- Heart racing without reason, lasting more than a few minutes
- Dizziness or fainting with a fast or slow pulse
- Chest pain or pressure along with an irregular heartbeat
- Shortness of breath that doesn’t go away
-then get checked. Don’t wait. Early detection saves lives. A simple ECG can catch what you can’t feel.
Living With an Arrhythmia
Having an arrhythmia doesn’t mean you can’t live fully. Millions do. With the right treatment, most people return to normal activity. You might need to take meds daily. You might have a device implanted. But you can still walk, swim, work, and enjoy life.
Keep track of symptoms. Note when they happen, what you were doing, and how long they lasted. Bring that log to your doctor. It helps them choose the best treatment. Stay up to date on checkups. Blood tests, ECGs, and device checks are routine but vital.
Know your medications. Understand why you’re taking each one and what side effects to watch for. Don’t stop them without talking to your doctor-even if you feel fine.
What’s New in Treatment?
Technology is improving fast. Pulsed field ablation (PFA) is replacing older thermal methods in many centers. It’s faster, safer, and less likely to damage surrounding tissue. Newer pacemakers can communicate wirelessly with your phone, sending data to your doctor without office visits. Smartwatches now detect irregular rhythms and can alert you to possible AFib.
Research is also focusing on personalized treatment. Instead of trial-and-error, doctors are using genetic markers and heart imaging to predict who will respond best to which drug or procedure. This means better outcomes and fewer side effects.
Final Thoughts
Atrial fibrillation, bradycardia, and tachycardia aren’t the same. But they all point to one thing: your heart’s electrical system is out of balance. The good news? We know how to fix it. Whether it’s medication, a device, or a simple lifestyle change, help is available.
Don’t ignore your body. If something feels off, get it checked. You don’t need to wait for a crisis. A 10-minute ECG today could prevent a hospital visit tomorrow.
Can stress cause arrhythmias?
Yes. Stress triggers adrenaline, which can speed up your heart or make it beat irregularly. Chronic stress is linked to higher rates of atrial fibrillation and tachycardia. Managing stress through sleep, exercise, or therapy can reduce episodes.
Can I exercise if I have an arrhythmia?
Usually yes-but it depends on the type and severity. Most people with well-controlled AFib or bradycardia can do moderate exercise like walking, swimming, or cycling. Avoid intense bursts if you have ventricular tachycardia. Always check with your doctor before starting a new routine.
Is atrial fibrillation curable?
It can be managed effectively, and in some cases, cured. Ablation has a 70-80% success rate for paroxysmal AFib. For persistent cases, success drops but is still possible. Even if it doesn’t go away completely, controlling the rhythm and preventing stroke makes a huge difference in quality of life.
Do all arrhythmias need medication?
No. Some people with mild bradycardia or occasional SVT don’t need drugs. Lifestyle changes or simple maneuvers can be enough. Medication is used when symptoms are frequent, risky, or when the heart can’t pump well on its own.
Can a smartwatch diagnose arrhythmias?
Some smartwatches can detect irregular rhythms and flag possible AFib. They’re useful for spotting patterns, but they’re not medical devices. A confirmed diagnosis always requires a clinical ECG. Use them as a tool-not a replacement-for professional care.




Inna Borovik - 7 December 2025
AFib isn't just some buzzword for old folks. I've seen it in my mom-silent until she coded. The stats are real, but nobody talks about how insurance denies ablation unless you're practically dead. Why do we wait for collapse before we act?
Rashmi Gupta - 7 December 2025
Interesting how this article treats tech like magic. Smartwatches? Please. I work in cardiology in Mumbai-we don’t have access to half this stuff. You think a farmer in Bihar is checking his pulse on an Apple Watch?
Andrew Frazier - 9 December 2025
USA still leads in cardiac tech but the rest of the world is just copying. Why? Because we don’t let the FDA slow us down like Europe. Pulsed field ablation? We’ve been doing it since 2020. Other countries are still stuck on pacemakers from the 90s. #AmericanExcellence
Gwyneth Agnes - 10 December 2025
Stop taking beta blockers. They make you fat. Just eat less sugar. Done.
Katie O'Connell - 11 December 2025
It is, perhaps, worth noting that the prevailing clinical paradigm for arrhythmic management remains anchored in a biomedical model that privileges pharmacological and procedural intervention over holistic, psychosocial determinants of cardiac health. One must question the epistemological hegemony of ECG-centric diagnostics when lifestyle factors-dietary inflammation, circadian disruption, and chronic psychological stress-are demonstrably upstream etiologies.
Brooke Evers - 12 December 2025
I just want to say how proud I am of you for sharing this. So many people suffer in silence because they think it’s just ‘normal aging’ or ‘stress’. But you’re right-checking your pulse is one of the most powerful things you can do. I used to ignore my palpitations until I passed out at the grocery store. Now I track everything. It’s scary, but knowing your body saves your life. You’re not alone. I’ve been there too.
Saketh Sai Rachapudi - 13 December 2025
Smartwatches detect AFib? LOL. In India we dont even have proper hospitals. This is all western propaganda to sell gadgets. Real doctors dont need watches to know your heart is messed up. You need a stethoscope and guts. Not a phone app.
Nigel ntini - 15 December 2025
I love how this post balances technical detail with real human advice. The part about lifestyle changes? That’s the real win. I had SVT for years. Tried meds. Didn’t help. Then I started yoga, cut caffeine, and slept 8 hours. No more episodes. No device. Just simple changes. It’s not sexy, but it works. Don’t underestimate the power of calm.
pallavi khushwani - 15 December 2025
you know what’s wild? we all think of the heart like a machine. but it’s more like a song. sometimes it’s off-key because the singer is tired. not broken. maybe we treat it too hard. what if we stopped trying to ‘fix’ it and started listening to it instead?
Dan Cole - 16 December 2025
Let me break this down for the masses who think a pacemaker is a cure. It’s not. It’s a Band-Aid on a leaking dam. The real problem is systemic inflammation from processed food, EMF exposure, and government-enforced sedentary lifestyles. They’re selling you devices while the root cause-corporate food, fluoride, and 9-to-5 slavery-goes unchallenged. Wake up. The system wants you dependent.
Jackie Petersen - 18 December 2025
Who funded this? Medtronic? Abbott? They own the FDA. Pulsed field ablation? That’s just a new way to charge $50k. Meanwhile, people in rural Texas can’t afford insulin. This isn’t medicine-it’s a cash grab dressed in science.
Geraldine Trainer-Cooper - 19 December 2025
Stress causes arrhythmias? No duh. We live in a world that rewards burnout. Sleep is a luxury. Coffee is oxygen. We’re not surprised when our hearts rebel. The real question is why we keep punishing ourselves and call it productivity.
Kenny Pakade - 20 December 2025
This whole thing is a scam. Bradycardia in athletes? Yeah right. They’re all on steroids. Your heart slows down because your body’s poisoned with synthetic junk. Real humans don’t have 40 BPM hearts. That’s not strength-that’s toxicity. Wake up sheeple.