Anticholinergic Burden Calculator
Anticholinergic medications block acetylcholine, a brain chemical crucial for memory. Long-term use is linked to a 49% higher dementia risk. Check your medications' impact using the Anticholinergic Cognitive Burden (ACB) scale.
Your Medication List
No medications added yet
Your Anticholinergic Burden Score
Current Score
0 (Low Risk)
Low Risk
Score: 0-1
Minimal dementia risk
Safer Alternatives
Consider these alternatives:
- For sleep: Melatonin or CBT-I instead of diphenhydramine
- For allergies: Loratadine or cetirizine instead of Benadryl
- For bladder control: Mirabegron instead of oxybutynin
- For depression: SSRIs like sertraline instead of amitriptyline
Talk to your doctor about deprescribing options.
For millions of older adults, taking a daily pill for sleep, allergies, bladder control, or depression seems harmless-until memory starts slipping. What many don’t realize is that some of these common medications may be quietly speeding up cognitive decline. Anticholinergic drugs, which block a brain chemical called acetylcholine, are linked to a higher risk of dementia, especially with long-term use. This isn’t theoretical. Real studies show people who take these meds for years have measurable brain changes, worse memory, and a nearly 50% higher chance of developing dementia.
What Are Anticholinergic Medications?
Anticholinergic medications work by blocking acetylcholine, a neurotransmitter that helps with memory, learning, muscle control, and even bladder function. These drugs were developed decades ago to treat conditions like Parkinson’s, motion sickness, and stomach cramps. Today, they’re still widely used-but not always for the right reasons.
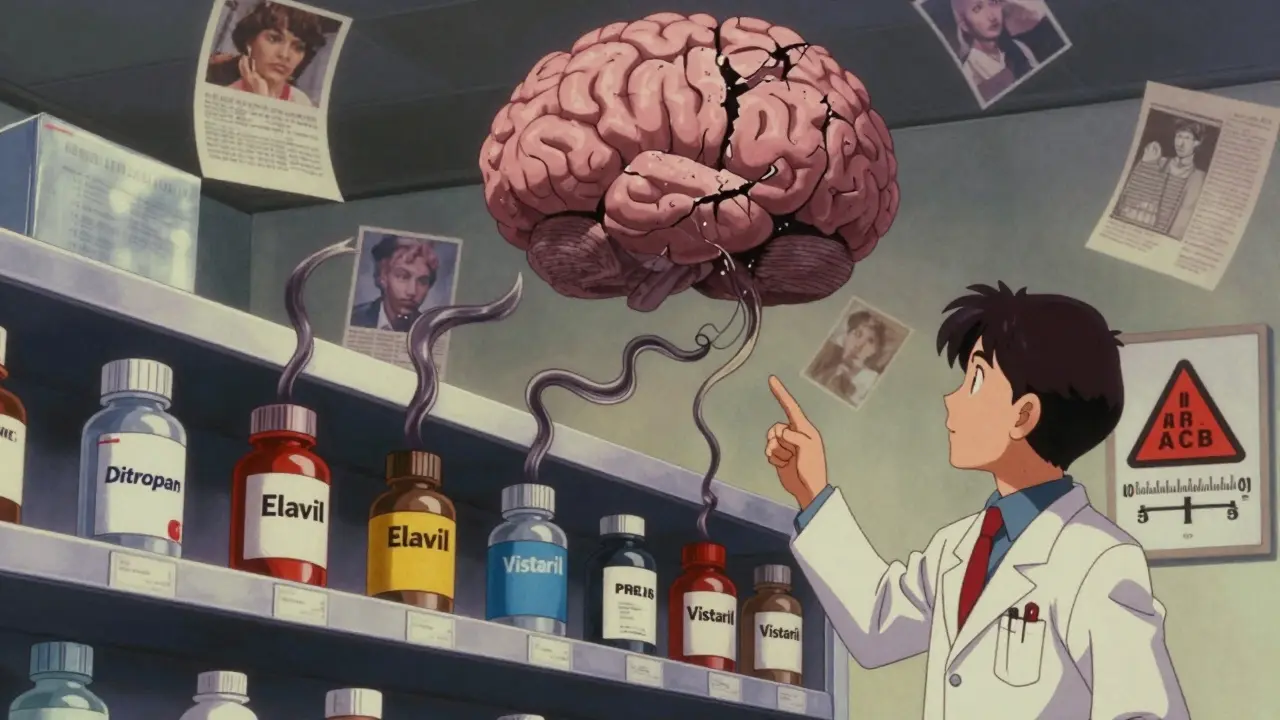
Over 100 medications fall into this category. Common ones include:
- Diphenhydramine (Benadryl) - for allergies and sleep
- Oxybutynin (Ditropan) - for overactive bladder
- Amitriptyline (Elavil) - for depression and nerve pain
- Hydroxyzine (Vistaril) - for anxiety and itching
- Chlorpheniramine - in many cold and flu mixes
What makes these drugs dangerous over time is their ability to cross the blood-brain barrier. Tertiary amines like amitriptyline and diphenhydramine easily enter the brain, while others, like glycopyrrolate, mostly stay in the body. That’s why some anticholinergics wreck cognitive function while others barely touch it.
The Link Between Anticholinergics and Dementia
It’s not just a theory-it’s backed by brain scans, long-term data, and real-world outcomes. A 2019 study using data from over 3,400 older adults found that those taking medications with strong anticholinergic effects had a 49% higher risk of dementia compared to those who didn’t take any. That risk didn’t pop up overnight. It built up slowly, like a leaky faucet filling a bucket.
Researchers measured exposure using something called cumulative defined daily doses (cDDD). People who took the equivalent of more than 1,095 daily doses over a few years saw the biggest jump in risk. That’s about three years of daily use. Even lower exposure-like 1 to 90 doses-still carried a 6% increased risk.
Brain imaging showed something even more alarming. People on these drugs had 0.5% to 1.2% more annual brain volume loss in areas like the hippocampus and amygdala-the same regions that shrink in Alzheimer’s disease. Glucose metabolism dropped by 4% to 8% in key brain zones, meaning those areas were literally running out of fuel.
Not All Anticholinergics Are Created Equal
Here’s the thing: not every anticholinergic drug carries the same risk. Some are far more dangerous than others.
According to a 2019 JAMA Internal Medicine study:
- Antidepressants (like amitriptyline): 29% higher dementia risk
- Antipsychotics: 20% higher risk
- Bladder drugs (oxybutynin, solifenacin): 13-20% higher risk
- Parkinson’s meds: 10% higher risk
But here’s the twist: not all bladder meds are the same. Oxybutynin and solifenacin increased dementia risk, but trospium-another bladder drug-showed no significant link. Why? Trospium doesn’t cross the blood-brain barrier as easily. That’s why switching to non-anticholinergic alternatives can make a real difference.
Same goes for sleep aids. Diphenhydramine (Benadryl) is a big culprit. But melatonin or cognitive behavioral therapy for insomnia? Those don’t touch acetylcholine.
Who’s Most at Risk?
Older adults, especially those over 65, are the most vulnerable. But it’s not just age. People with a family history of Alzheimer’s, those carrying the APOE-ε4 gene, or anyone already showing mild memory issues are at even higher risk.
And here’s something most people don’t realize: you don’t have to be taking one strong anticholinergic to be in danger. Many people take two or three mild ones-like an allergy pill, a sleep aid, and a stomach med. Add them up, and the total anticholinergic burden can be just as harmful as one strong drug.
The Anticholinergic Cognitive Burden (ACB) scale rates drugs from 1 (mild) to 3 (strong). A score of 3 or higher over time is linked to significant cognitive decline. Many seniors have cumulative ACB scores of 4, 5, or even higher-without ever knowing it.
What You Can Do: Deprescribing and Alternatives
The good news? This risk is mostly preventable. Stopping these drugs doesn’t always mean losing symptom control-it just means switching to safer options.
Here are proven alternatives:
- For depression: Switch from amitriptyline to an SSRI like sertraline or escitalopram. These have zero anticholinergic effect.
- For overactive bladder: Try mirabegron (Myrbetriq) instead of oxybutynin. It works differently and doesn’t affect the brain.
- For insomnia: Use sleep hygiene, CBT-I, or melatonin instead of diphenhydramine.
- For allergies: Choose non-sedating antihistamines like loratadine (Claritin) or cetirizine (Zyrtec).
Deprescribing isn’t about quitting cold turkey. It’s a slow, supervised process. The Canadian Deprescribing Guidelines recommend tapering over 4 to 8 weeks to avoid withdrawal symptoms like rebound anxiety, sweating, or nausea.
Some doctors still don’t screen for anticholinergic burden. A 2021 survey found only 37% of primary care doctors routinely check for it in patients over 65-even though 89% say they know it’s risky. That gap is dangerous.
What’s Being Done to Fix This?
Change is happening, but slowly.
The American Geriatrics Society updated its Beers Criteria® in 2019 to strongly advise against using strong anticholinergics in older adults. The FDA added stronger warning labels to 14 of these drugs in 2020. The European Medicines Agency restricted seven bladder drugs for elderly use in 2021.
Some health systems are taking action. Epic Systems, one of the biggest electronic health record platforms, now includes an anticholinergic burden calculator that flags high-risk prescriptions. The American Geriatrics Society launched the Anticholinergic Risk Reduction Initiative in 2022, aiming to cut inappropriate prescribing by 50% by 2027.
Meanwhile, drug companies are developing new medications designed to avoid the brain entirely. As of 2023, seven new bladder treatments and three new antidepressants are in late-stage trials-all with minimal CNS penetration.
Real Stories, Real Consequences
Behind the numbers are real people.
One Reddit user shared that her mother took amitriptyline for eight years for nerve pain. Her MMSE score-a standard memory test-dropped from 28 (normal) to 22 (mild cognitive impairment). After stopping the drug, her score stabilized-but never returned to what it was.
Another woman in the Alzheimer’s Association forum switched from oxybutynin to mirabegron. Within three months, she noticed she could remember names again. She hadn’t realized how foggy her mind had become until the fog lifted.
But here’s the problem: most patients don’t connect their meds to their memory. On Drugs.com, 68% of oxybutynin users rated it as “excellent” for bladder control. Only 22% mentioned brain fog. Why? Because doctors rarely warn them. And because the side effects creep in slowly-you don’t wake up one day forgetting your keys. You just slowly forget more and more.
What Should You Do Now?
If you or someone you love is taking any of these medications:
- Check the list. Look up every medication you take-prescription and over-the-counter. Use the Anticholinergic Cognitive Burden (ACB) scale to find the rating.
- Add up the score. If the total is 3 or higher, talk to your doctor. Don’t stop cold turkey.
- Ask about alternatives. Is there a non-anticholinergic option? Can you try a lower dose? Can you use a non-drug approach?
- Ask for a cognitive baseline. If you’re over 65 and on these meds, get a simple memory test now. It’s the only way to track changes.
This isn’t about fear. It’s about awareness. Many of these drugs are still necessary for some people. But for millions, they’re a quiet, slow-burning risk-and one we can actually do something about.
The science is clear: reducing anticholinergic exposure could prevent up to 15% of dementia cases each year. That’s over half a million people worldwide. You don’t need a miracle drug to protect your brain. You just need to ask the right questions.
Can anticholinergic medications cause dementia, or just make memory worse temporarily?
Long-term use of anticholinergic medications is linked to actual structural brain changes and a higher risk of dementia, not just temporary memory lapses. Studies using brain scans show increased volume loss in areas like the hippocampus and reduced glucose metabolism-patterns seen in early Alzheimer’s. The risk builds over time, with exposure over three years or more showing the strongest association.
Are over-the-counter antihistamines like Benadryl dangerous for older adults?
Yes. Diphenhydramine (Benadryl) is a strong anticholinergic with high brain penetration. It’s one of the most common sources of anticholinergic exposure in seniors, especially when used for sleep. Studies show it increases dementia risk significantly with long-term use. Non-sedating alternatives like loratadine or cetirizine are much safer.
If I stop taking an anticholinergic drug, will my memory improve?
Some people do notice improvement after stopping, especially if they’ve been on the drug for less than a few years. But if brain changes have already occurred, recovery may be partial. The earlier you stop, the better the chance of preserving cognitive function. Stabilization is common-even full recovery is possible in some cases, but it’s not guaranteed.
What’s the safest medication for overactive bladder in older adults?
Mirabegron (Myrbetriq) is the top non-anticholinergic alternative. It works by relaxing the bladder muscle without affecting acetylcholine. Studies show it’s just as effective as oxybutynin but carries no increased dementia risk. Other options include pelvic floor therapy, timed voiding, or Botox injections for severe cases.
How can I find out if my medication has anticholinergic effects?
You can check the Anticholinergic Cognitive Burden (ACB) scale online or ask your pharmacist. Many drugs list anticholinergic effects in their patient information leaflets, though many don’t. The best approach is to bring your full medication list to your doctor and ask: “Which of these have anticholinergic properties, and what’s the total burden?”
Is it safe to take anticholinergics for a short time, like a few weeks?
Short-term use (under one year) shows little to no increased dementia risk in recent studies. The danger comes from long-term, cumulative exposure. A single course of diphenhydramine for a bad cold is unlikely to cause harm. But using it nightly for months or years? That’s where the risk builds.




Molly McLane - 6 January 2026
I’ve been telling my mom for years to stop taking Benadryl for sleep. She swears it’s harmless because it’s ‘over-the-counter.’ Then last month she forgot my birthday. Not because she was tired-because her brain was foggy from years of anticholinergics. I printed out the ACB scale and sat her down. She cried. But she switched to melatonin last week. Her memory’s already clearer. It’s not magic-it’s just stopping something that was slowly stealing her mind.
Doctors don’t warn us. Pharmacists don’t flag it. We just assume if it’s sold beside cough syrup, it’s safe. It’s not.
Thank you for writing this. Someone needed to say it out loud.
Gabrielle Panchev - 8 January 2026
Let me just say-this entire article is a classic case of medical overreach dressed up as ‘awareness.’ You’re acting like every single anticholinergic is a slow-acting poison, but let’s not forget: these drugs exist because they WORK. People with severe overactive bladder don’t get to choose between ‘cognitive safety’ and ‘wearing diapers.’ And yes, amitriptyline helps with chronic pain that no SSRIs touch. You’re not offering alternatives-you’re offering fear. And fear doesn’t heal people. Practical, individualized care does. Also, the ‘49% higher risk’ statistic? That’s relative risk. Absolute risk? Maybe 1.5% vs. 1%. That’s not a crisis-it’s a nuanced trade-off. Stop scaremongering.
Also-why is it always older people who get blamed for their own cognitive decline? What about diet? Sleep? Screen time? Alcohol? Why is it always the meds?
And no, I’m not taking anything. But I know someone who is. And I’m tired of being guilted into thinking their medication is the villain.
Harshit Kansal - 8 January 2026
Bro my grandma was on oxybutynin for like 5 years and she started forgetting where she put her dentures. Then she switched to mirabegron and suddenly she remembered her own name. No joke. She started telling stories from the 70s again. I think the doc just didn’t know better. But now she’s like a new person. Just sayin’.
Also-Benadryl is the worst. Don’t let your auntie take it for sleep. She’ll forget where she put the TV remote and then blame the dog.
Saylor Frye - 10 January 2026
It’s fascinating how the medical establishment has now decided that pharmacology is a moral failing. The real issue isn’t anticholinergics-it’s the commodification of aging. We’ve created a society where cognitive decline is treated like a bug to be patched, not a natural process to be understood. The fact that we’re now pathologizing decades-old medications while ignoring systemic neglect-poor nutrition, social isolation, lack of physical activity-is telling. You want to prevent dementia? Fix the culture. Not just the prescription pad.
Also, ‘anticholinergic burden’ sounds like something a pharmaceutical rep coined to sell a new drug. Just sayin’.
Katie Schoen - 11 January 2026
So let me get this straight: you’re telling me that the same damn diphenhydramine I used to take to knock out after a 12-hour shift is now a dementia bomb? And nobody told me? I’ve been popping those like candy since 2015. I thought I was just tired, not brain-dead.
Also-my sister’s doctor just prescribed her amitriptyline for fibromyalgia. She’s 68. I just sent her this article. She’s gonna have a meltdown. But honestly? I’m glad someone finally said it. We’re all just guessing what’s safe. This should be on every pharmacy shelf. Like ‘Caution: May cause slow brain rot.’
Jeane Hendrix - 12 January 2026
Interesting that the ACB scale is not standardized across all electronic health records. I’ve seen it flagged inconsistently even within the same health system. Also, many patients don’t realize that OTC meds count-especially when they’re taking multiple low-dose anticholinergics. The cumulative effect is real, but the documentation is fragmented. There’s a gap between clinical knowledge and real-world prescribing. We need automated alerts at the point of dispensing, not just ‘awareness campaigns.’ And honestly? Most geriatricians still don’t use the scale. It’s a systemic failure, not just a patient education issue.
Also-trospium is underutilized. Why? Because it’s more expensive. And insurance won’t cover it unless you’ve failed three anticholinergics first. That’s not patient care. That’s cost containment masquerading as clinical caution.
Katelyn Slack - 12 January 2026
my doctor never told me any of this. i took oxybutynin for 3 years and i thought i was just getting forgetful. now i feel so dumb for not asking. i switched to mirabegron last month and my brain feels… lighter? like the fog lifted. i wish i’d known sooner. please share this with your parents. they’ll thank you later.
Melanie Clark - 12 January 2026
They’re hiding the truth. The pharmaceutical companies know. They’ve known for decades. That’s why they’re pushing these ‘new’ non-anticholinergic drugs now-because they’re making billions off the old ones. They don’t want you to stop. They want you to keep taking them until your brain turns to mush, then sell you expensive memory pills. The FDA warnings? Too little, too late. This is all a money game. And your grandma’s dementia? It’s on their balance sheet.
They’re also pushing this ‘natural alternatives’ nonsense to distract you. Melatonin doesn’t cure anything. It’s just a placebo with a label. The real solution? Ban all anticholinergics for seniors. Now.
And don’t trust your doctor. They’re paid by the system. Read the studies yourself. The data is buried-but it’s there.
Vinayak Naik - 13 January 2026
Yo from India here-my uncle was on amitriptyline for 10 years for nerve pain. He was a walking zombie. Forgot his own wedding anniversary. Then his son switched him to duloxetine. Boom. He started recognizing his grandkids again. No drama. No hype. Just science. Also, in India, most docs still prescribe diphenhydramine for sleep like it’s tea. People have no clue. This needs to go viral here. We need to stop treating brain fog like normal aging. It’s not. It’s preventable. And yeah-trospium is a gem. Why isn’t it in every pharmacy? Because nobody’s screaming about it.
Shoutout to the author. This is the kind of post that saves lives. Not just brains. Lives.