What You Need to Know About Bipolar Disorder Medications
Living with bipolar disorder means navigating extreme mood swings - from deep depression to intense mania. Medications don’t cure it, but they can keep those swings from wrecking your life. The two main classes of drugs used are mood stabilizers and antipsychotics. Getting the right mix, at the right dose, with the right monitoring, makes all the difference. But it’s not just about popping pills. It’s about understanding side effects, knowing when to adjust, and recognizing warning signs before they become emergencies.
Mood Stabilizers: The Foundation of Long-Term Control
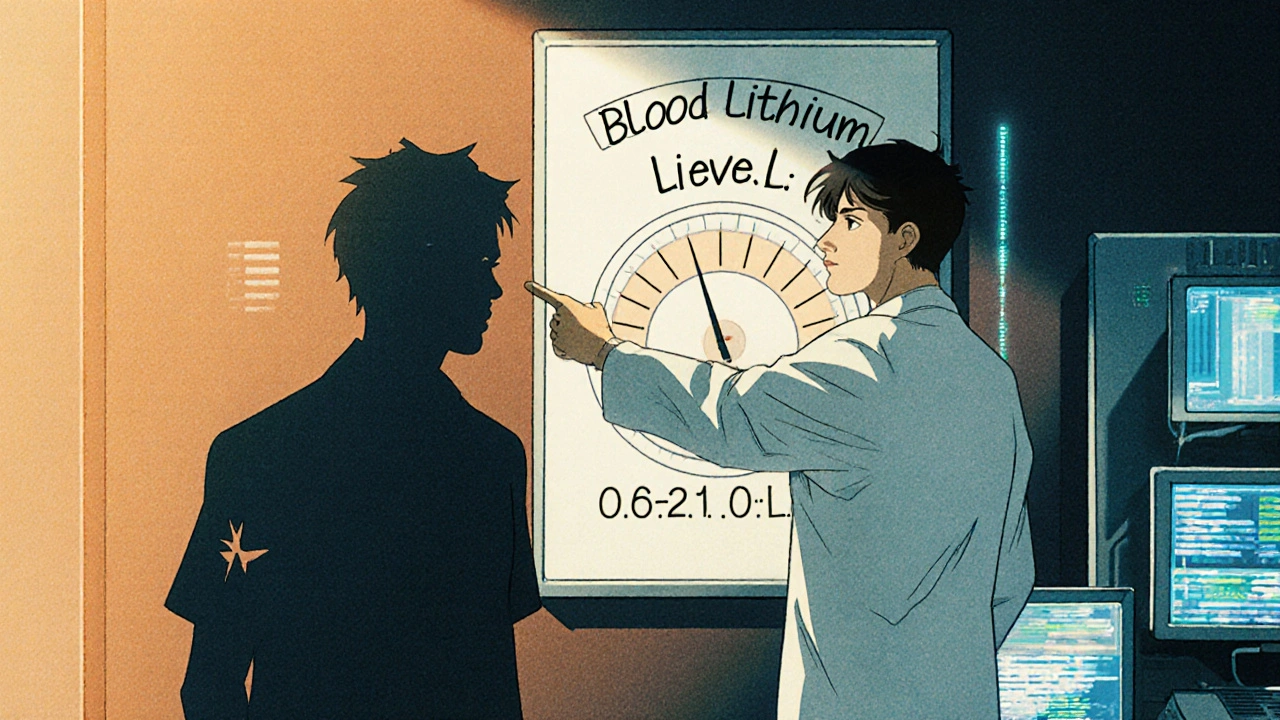
Lithium has been the gold standard since the 1970s. It’s not flashy, but it works. Studies show it cuts suicide risk by 80% compared to no treatment. For many, it’s the only drug that prevents both manic and depressive episodes over years. But it’s not simple. You need regular blood tests - weekly at first, then every 2-3 months once stable. The goal? Keep blood levels between 0.6 and 1.0 mmol/L. Too low, and it doesn’t help. Too high, and you risk toxicity: slurred speech, shaking, even seizures.
Side effects are common. About half of users get hand tremors. Three in ten feel constantly thirsty and pee nonstop. Weight gain is typical - 10 to 15 pounds in the first year. Nausea hits 20-30%. Many people quit because of this. But others say: "I gained weight, but I haven’t had a suicidal episode in three years. It’s worth it."
Other mood stabilizers include valproate, carbamazepine, and lamotrigine. Valproate works fast for mania but carries a black box warning: it can cause severe birth defects. Carbamazepine interacts with dozens of other drugs. Lamotrigine is gentler on weight and metabolism, and it’s one of the best for preventing depression - but it can cause a rare, dangerous skin rash in about 1 in 10 people. That’s why doctors start low and go slow with it.
Antipsychotics: Fast Relief, But Trade-Offs
Atypical antipsychotics like quetiapine, olanzapine, risperidone, and aripiprazole are now used as often as mood stabilizers. Why? They work fast. Quetiapine can start lifting depression in as little as 7 days. Lithium takes two weeks or more. For someone in acute crisis, speed matters.
But the cost is high. Quetiapine causes drowsiness in 60-70% of users. Olanzapine leads to an average 4.6 kg weight gain in just six weeks. It also raises diabetes risk by 20-30%. Risperidone can cause restlessness (akathisia) in up to 20% of people - a feeling so uncomfortable, some say it’s worse than the original symptoms. Aripiprazole is lighter on weight gain but can trigger anxiety or agitation in some.
Patients on PatientsLikeMe rated quetiapine 3.7 out of 5 for effectiveness, but only 2.8 for tolerability. Two-thirds reported weight gain averaging 22 pounds. One Reddit user wrote: "I took olanzapine for six months. I gained 40 pounds. I stopped because I couldn’t look in the mirror anymore."
Combining Medications: More Power, More Problems
When one drug isn’t enough, doctors often combine a mood stabilizer with an antipsychotic. This approach works for about 70% of treatment-resistant cases. But side effects pile up. Weight gain, metabolic issues, sedation - they don’t just add up, they multiply. A person on lithium plus quetiapine might face tremors, constant thirst, drowsiness, and rapid weight gain all at once.
Some patients manage this by adding metformin, a diabetes drug that helps reverse weight gain from antipsychotics. Others split their doses - taking half in the morning, half at night - to reduce daytime drowsiness. Still, 40% of people stop taking their meds within a year because the side effects feel worse than the illness.
What About Antidepressants?
It’s tempting. If you’re in a deep depression, shouldn’t an SSRI like fluoxetine help? Maybe - but not alone. In bipolar disorder, antidepressants can flip you into mania. Studies show this happens in 10-15% of cases. Some experts say the risk is as high as 25%. That’s why guidelines say: never use an antidepressant without a mood stabilizer or antipsychotic in place.
Even then, use is controversial. Some doctors avoid them entirely. Others use them briefly, with close monitoring, for severe depressive episodes. The key is timing and supervision. Don’t self-prescribe. Don’t increase the dose without talking to your psychiatrist.
Monitoring: It’s Not Optional
Managing bipolar meds isn’t a set-it-and-forget-it job. It’s ongoing. Blood tests for lithium. Quarterly checks for blood sugar, cholesterol, and waist size. Weight tracking. Liver function tests if you’re on valproate. These aren’t just routine - they’re life-saving.
For lithium, your doctor should check your kidney and thyroid function every 6-12 months. For antipsychotics, you need to watch for metabolic syndrome: waist over 40 inches for men, 35 for women, plus high blood pressure or fasting glucose above 100 mg/dL. These aren’t just numbers - they’re early signs of heart disease and diabetes.
One patient shared: "I didn’t know my glucose was rising until I passed out at work. My doctor said if I’d come in three months earlier, we could’ve stopped it."
Real People, Real Choices
There’s no one-size-fits-all. One person found peace with lithium after three failed trials. Another switched from quetiapine to lamotrigine - and got insomnia so bad they couldn’t sleep for weeks. A third started on aripiprazole, hated the anxiety, and moved to lurasidone - a newer antipsychotic that causes minimal weight gain.
According to a 2022 NAMI survey of 1,200 people, the top reasons for quitting meds were:
- Weight gain (78%)
- Cognitive fog - feeling slow, spaced out (65%)
- Sexual dysfunction (52%)
But 45% of those who stuck with treatment said their quality of life improved dramatically. One wrote: "I used to cry every night. Now I go to work. I play with my kids. I don’t feel like a burden. That’s worth the tremors."
What’s New in 2025?
The field is changing. In 2023, the FDA approved lumateperone (Caplyta) for bipolar depression - with almost no weight gain. Long-acting injectables like Abilify Maintena mean you only need one shot a month instead of daily pills. That helps with adherence.
Genetic testing is becoming more common. Tests like Genomind’s look at how your body processes meds based on your CYP2D6 and CYP2C19 genes. If you’re a slow metabolizer, you might get sick on standard doses. If you’re fast, you might need more. These tests improve success rates by about 30%.
Next up? Ketamine-like drugs that work in hours, not weeks. Digital tools like reSET-BD, an app that tracks mood and medication, are showing promise in cutting relapse by 22%.
When to Call Your Doctor
Don’t wait for a crisis. Call if you notice:
- Shaking hands that get worse - especially if you’re on lithium
- Drinking way more water than usual, peeing constantly, or feeling dizzy
- Sudden weight gain (5+ pounds in two weeks)
- Confusion, blurred vision, or muscle stiffness
- Any rash - even a small one - especially if you’re on lamotrigine
These aren’t "just side effects." They’re signals. Early action can prevent hospitalization.
Final Thoughts: It’s a Balancing Act
There’s no perfect drug. Every medication has trade-offs. The goal isn’t to feel perfectly normal - it’s to feel stable enough to live. To work. To be with family. To sleep through the night.
Success means finding the lowest dose that works. The fewest side effects you can tolerate. And a doctor who listens. Many people cycle through three or four meds before finding their fit. That’s normal. Don’t give up. But don’t suffer in silence, either. Talk. Track. Test. Adjust. Your brain deserves that effort.
Can mood stabilizers cure bipolar disorder?
No, mood stabilizers don’t cure bipolar disorder. They help manage symptoms by reducing the frequency and severity of manic and depressive episodes. Many people need to stay on them long-term to prevent relapse. Think of them like insulin for diabetes - they control the condition but don’t eliminate it.
Which is better: lithium or quetiapine?
It depends on your needs. Lithium is best for long-term prevention of both mania and depression, especially if suicide risk is high. It’s also cheaper and has been studied for decades. Quetiapine works faster for acute depression and mania and is easier to start, but it causes more weight gain and drowsiness. Many people use both together - lithium for stability, quetiapine for quick relief.
Why do I need blood tests if I feel fine?
Because you can feel fine and still be in danger. Lithium toxicity doesn’t always cause obvious symptoms until it’s too late. Blood levels can creep up due to dehydration, new medications, or even changes in salt intake. A level of 1.2 mmol/L or higher can cause seizures or kidney damage. Regular tests catch this before it becomes an emergency.
Can I stop my meds if I feel better?
Never stop suddenly. Stopping lithium or antipsychotics abruptly can trigger a severe relapse - sometimes worse than before. If you want to change or stop your meds, talk to your doctor first. They’ll help you taper slowly, over weeks or months, to avoid withdrawal and rebound episodes.
Do generics work as well as brand-name drugs?
For mood stabilizers like lithium carbonate and valproate, generics are just as effective and much cheaper - often under $40 a month. For antipsychotics, brand-name versions like Vraylar can cost over $1,200/month, but generics like risperidone or quetiapine are widely available and equally effective. Always check with your pharmacist to make sure the generic is bioequivalent.
What should I do if I gain too much weight?
Talk to your doctor. Weight gain from antipsychotics is common but manageable. Options include switching to a lower-risk drug like lurasidone or aripiprazole, adding metformin (which helps reverse insulin resistance and reduces weight), or working with a dietitian. Don’t assume it’s just "eating too much" - these drugs directly affect metabolism.
Are there non-medication options that help?
Yes, but they’re complements, not replacements. Regular sleep, structured routines, therapy (especially CBT or IPSRT), and avoiding alcohol/drugs are critical. Apps like reSET-BD help track mood and medication adherence. Exercise improves mood stability. But if you’re having frequent episodes, meds are still the most reliable tool for preventing hospitalization and suicide.
Next Steps: What to Do Today
- If you’re on meds: Write down your top two side effects and bring them to your next appointment.
- If you’ve stopped meds: Schedule a follow-up. Don’t wait until you’re in crisis.
- If you’re starting: Ask your doctor about baseline blood tests and a monitoring schedule.
- If you’re unsure: Get a second opinion. Bipolar treatment is personal - you deserve a plan that fits your life.





Alex Harrison - 8 November 2025
I've been on lithium for 5 years. Tremors suck but I'd rather shake than end up in the hospital. Blood tests are a pain but they saved my life when my level spiked after I started taking ibuprofen. Don't ignore the little things.
Jay Wallace - 10 November 2025
This article is laughably naive. In America we have access to the best meds in the world. If you're gaining weight or feeling foggy, you're clearly not trying hard enough. Get off the couch, stop eating carbs, and take your pills like an adult. This isn't 1995 anymore.
Alyssa Fisher - 12 November 2025
It's fascinating how we treat bipolar disorder like a mechanical problem-just swap out the parts until it runs smoothly. But the brain isn't a car. The side effects aren't just inconveniences; they're part of the person's lived experience. When we reduce someone's emotional range to 'stable,' are we healing them-or erasing them?
Alyssa Salazar - 13 November 2025
Lamotrigine is the holy grail for depressive-predominant bipolar if you don't have a history of SJS. The titration is brutal but worth it. Pair it with CBT and you're golden. Also, if you're on olanzapine and gaining 40 lbs, you're not doing it right-your doctor is either lazy or doesn't care. Push back. Your metabolism isn't broken, the drug is.
Beth Banham - 15 November 2025
I just wanted to say thank you for writing this. I've been on three different meds over eight years and I still feel like I'm guessing. This made me feel less alone.
Brierly Davis - 16 November 2025
You got this. I know it feels like you're fighting your own brain every day. But the fact that you're reading this, trying to understand, and still showing up? That's courage. Keep going. And if your doctor doesn't listen, find a new one. You deserve better.
Amber O'Sullivan - 17 November 2025
Lithium works but the thirst is insane I used to drink 5 liters a day and still felt like I was dying of thirst
Jim Oliver - 18 November 2025
Of course people quit. They're weak. If you can't handle a little weight gain or drowsiness, you shouldn't be on medication at all. This isn't a spa day-it's mental health care. Stop making excuses.
William Priest - 19 November 2025
Lumateperone? That's just a fancy name for a drug that hasn't been out long enough to know if it's safe. I've seen this movie before-everyone's hyped about the new miracle drug until the black box warning comes out. Stick with lithium. The old stuff is old for a reason.
Ryan Masuga - 20 November 2025
I was on quetiapine for 2 years. Gained 50 lbs, couldn't get out of bed before noon. Switched to lurasidone and lost 30 in 6 months. My therapist said I'm more present now. I didn't know I'd been living in a fog until I woke up. Don't give up. It takes time but it gets better.
Jennifer Bedrosian - 21 November 2025
I stopped my meds because I felt like a zombie and my husband said I looked like a ghost. We were trying to have a baby and I didn't want to risk it. Now I'm 7 months pregnant and I haven't had an episode since I quit. Maybe the meds weren't the answer. Maybe I just needed love and sleep
Lashonda Rene - 23 November 2025
I think people forget that meds aren't magic. They help but you still have to do the work. I go to therapy every week, I sleep at the same time every night, I don't drink, I walk every day. The meds keep me from falling off a cliff but the daily stuff keeps me from walking right back to the edge. It's not just about the pills, it's about building a life that doesn't need to be saved every day
Andy Slack - 23 November 2025
I just started aripiprazole. I'm still adjusting but I'm hopeful. I'm tracking my mood with an app and it's helping me see patterns. Small wins matter. You're not broken. You're adapting.