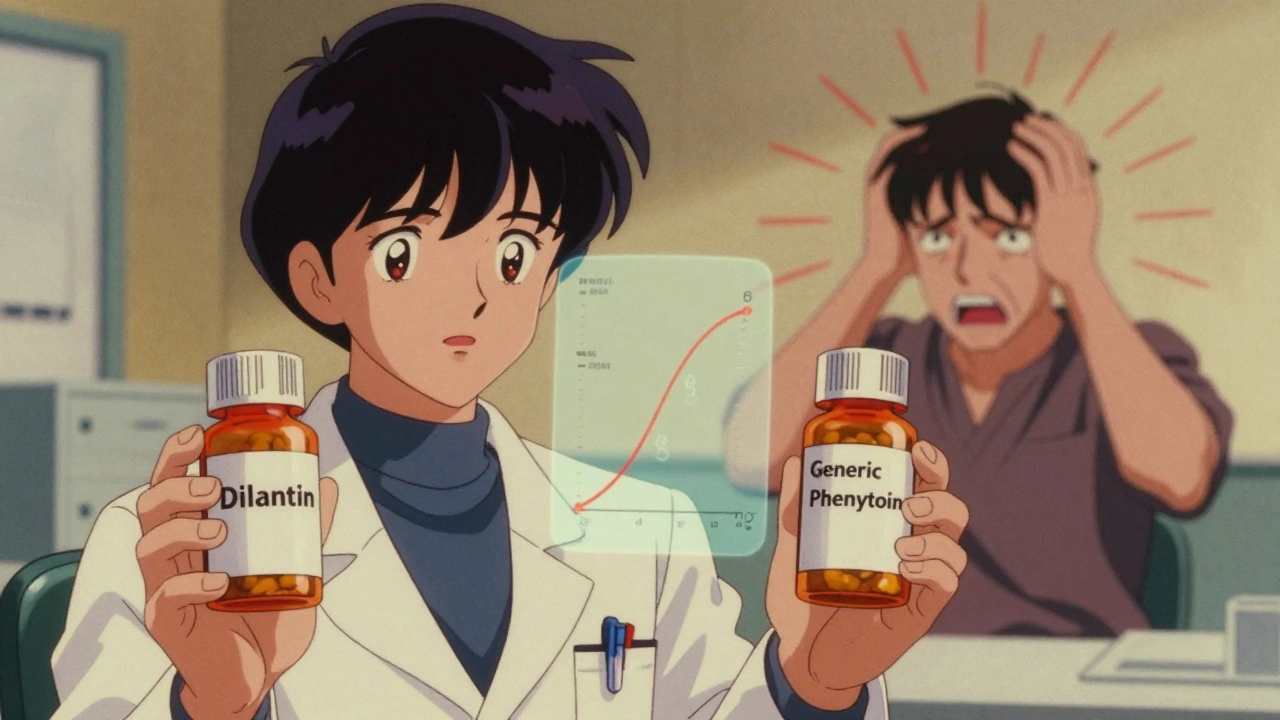
Switching from brand-name Dilantin to a generic version of phenytoin might seem like a simple cost-saving move-but for patients with epilepsy or seizure disorders, it can be anything but. Phenytoin isn’t like most medications. Even tiny changes in how much of the drug enters your bloodstream can mean the difference between controlling seizures and slipping into toxicity. And because generic versions, while legally approved, aren’t identical in how they’re absorbed, therapeutic drug monitoring becomes critical-not optional.
Why Phenytoin Is Different
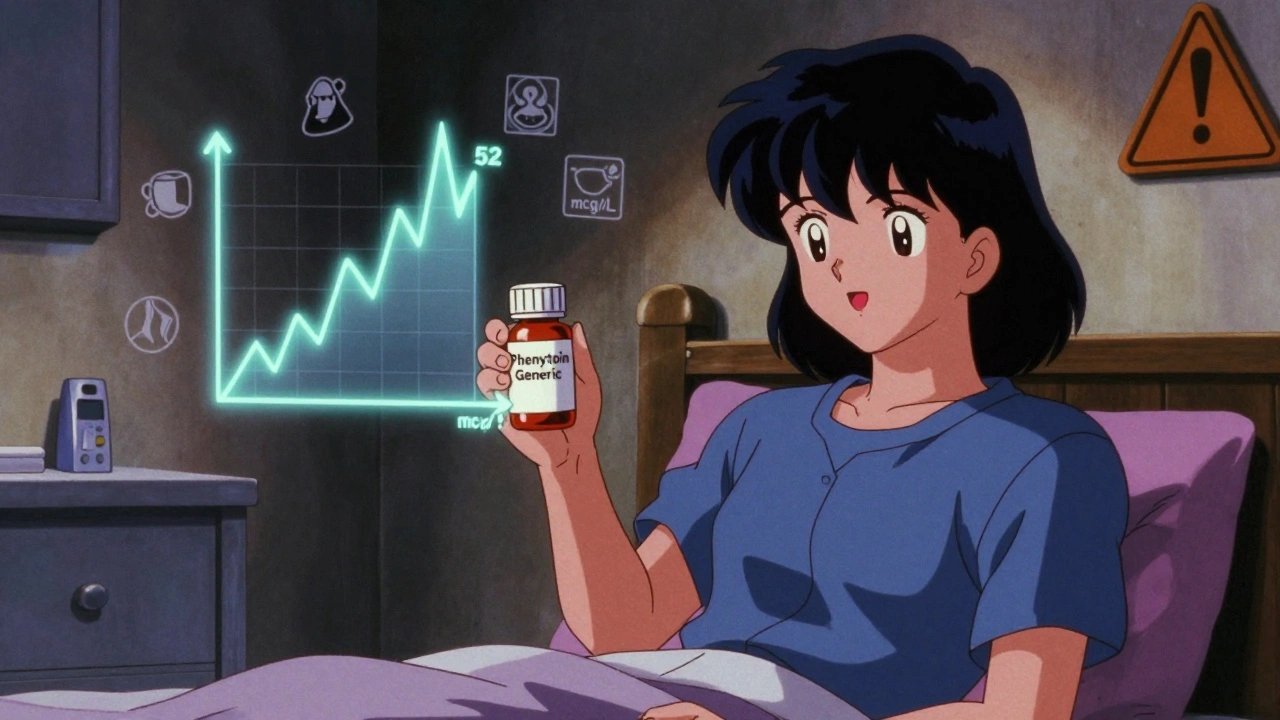
Phenytoin has been used since the 1930s to stop seizures, and it still works. But it’s tricky. It has a very narrow window where it’s effective: 10 to 20 mcg/mL in your blood. Go below 10, and seizures might return. Go above 20, and you risk dizziness, confusion, loss of coordination, or worse. At levels over 50 mcg/mL, it can be fatal. What makes it even more dangerous is how it’s processed. Most drugs follow a straight line: double the dose, double the blood level. Phenytoin doesn’t. Once you hit a certain concentration, your body’s ability to break it down gets overwhelmed. That’s called zero-order kinetics. A small increase-say, 25 to 50 mg more per day-can cause a huge spike in blood levels. One extra pill could push you into toxicity. Add to that: phenytoin is 90-95% bound to proteins in your blood. Only the small unbound portion actually works. If you’re low on albumin (common in older adults, liver disease, or malnutrition), more of the drug floats free-even if your total level looks fine. That’s why a "normal" total level can still mean you’re overdosing.Generic Switches: The Hidden Risk
The FDA says generics must be bioequivalent to the brand name. That means their absorption rates (AUC and Cmax) must fall within 80-125% of the original. Sounds close enough, right? Not for phenytoin. That 20% swing in absorption might be fine for a drug like aspirin. But for phenytoin? A 20% drop could mean your seizure control slips. A 20% rise? You could be headed for toxicity. And here’s the catch: different generic manufacturers use different fillers, binders, and coatings. These don’t change the active ingredient-but they can change how fast or how well your body takes it in. Studies and clinical guidelines agree: switching between brand and generic, or even between two different generic brands, can cause unpredictable shifts in blood levels. The NHS Tayside guideline from 2022 says it plainly: "Therapeutic monitoring may be required when switching formulations."When and How to Monitor
You can’t just check a level once and call it done. Timing matters.- Wait at least 5 days after starting or changing the dose before checking your level. Phenytoin takes that long to reach steady state.
- For IV doses, check 2-4 hours after the infusion.
- For oral doses, wait 12-24 hours.
- Always take the sample right before your next dose-that’s the "trough" level, and it’s the most accurate for dosing decisions.
Special Cases: Who Needs Extra Care
Some patients are at higher risk. Monitoring isn’t just recommended-it’s essential.- People with low albumin: If you’re malnourished, have liver disease, or are critically ill, your protein levels drop. That means more free phenytoin. Always ask for a free phenytoin level, not just the total. The formula to correct total levels (Measured level ÷ [(0.9 × Albumin ÷ 42) + 0.1]) is a rough guide at best. Your symptoms matter more than the number.
- Older adults: Slower metabolism, less protein, more medications-this group is especially vulnerable.
- Patients on other drugs: Many common medications change phenytoin levels. Antibiotics like trimethoprim-sulfamethoxazole, antifungals like fluconazole, and even alcohol can raise levels. Drugs like carbamazepine, rifampin, and theophylline can lower them. If you start or stop any new medicine, get checked.
- People with liver problems: Since phenytoin is processed by the liver, any impairment can slow clearance and increase risk.
Long-Term Monitoring Beyond Blood Levels
Phenytoin doesn’t just affect your brain. Long-term use can cause other problems:- Gingival hyperplasia: Swollen, overgrown gums. Brushing helps, but you’ll need regular dental checks.
- Bone health: Phenytoin interferes with vitamin D metabolism. Over time, this can lead to osteoporosis or fractures. Get your vitamin D, calcium, and alkaline phosphatase checked every 2-5 years.
- Blood counts: Rarely, it can cause low white blood cells or platelets. A simple CBC once a year is wise.
- Neuropathy: Numbness or tingling in hands or feet-report it early.
What to Do If You’re Switching
Here’s a simple action plan:- Before switching, ask your doctor to order a phenytoin level.
- Take the new generic exactly as prescribed-no skipping or doubling doses.
- Watch for new symptoms: dizziness, tremors, confusion, slurred speech, or seizure recurrence.
- After 5-10 days, get another level.
- If levels are outside 10-20 mcg/mL, or if you feel worse, don’t wait. Contact your doctor immediately.
- Keep a list of all your medications, including OTC and supplements, and share it at every visit.
Bottom Line
Generic phenytoin is not interchangeable like ibuprofen or lisinopril. Its narrow therapeutic window, nonlinear metabolism, and high protein binding make it one of the most dangerous drugs to switch without monitoring. The science is clear: when changing formulations, therapeutic drug monitoring isn’t a luxury-it’s a safety net. If you’re on phenytoin and your pharmacy switches your prescription, speak up. Ask for a level. Track your symptoms. Your brain depends on it.Do I need to check my phenytoin level every time I get a refill?
No. Routine monthly monitoring isn’t needed if you’re stable on the same formulation. But you should check your level after any dose change, illness, or switch in brand or generic. Once you’re steady, levels every 6-12 months are usually enough unless something changes.
Can I tell if my phenytoin level is too high just by how I feel?
Sometimes. Early signs include dizziness, unsteadiness, blurred vision, or slurred speech. But many people don’t notice symptoms until levels are dangerously high. That’s why blood tests are critical-you can’t rely on how you feel alone.
Why can’t I just take the cheapest generic?
The cheapest generic isn’t always the safest for phenytoin. Different manufacturers use different inactive ingredients that affect how the drug is absorbed. Even though they’re "bioequivalent," small differences can push your level into the toxic range. Stick with the same brand or generic unless your doctor approves a switch-and always check levels after.
Is free phenytoin testing available everywhere?
Not in every lab, but most hospitals and larger clinical labs offer it. If you have low albumin, kidney disease, or are critically ill, ask your doctor to specifically request a "free phenytoin" test. Relying on corrected total levels can be misleading.
What if I’m on a fixed income and can’t afford frequent blood tests?
This is a real challenge. But one test before and after a switch can prevent costly ER visits or hospitalizations. Ask your pharmacist or clinic if they offer sliding-scale fees or patient assistance programs. Some states have epilepsy foundations that help with monitoring costs. Never skip monitoring entirely-your safety is worth the effort.
Are there any alternatives to phenytoin if switching is too risky?
Yes. Newer antiepileptics like levetiracetam, lacosamide, or lamotrigine have wider therapeutic windows and don’t require routine monitoring. But they’re not always right for everyone. If phenytoin controls your seizures well and you’re stable, switching drugs carries its own risks. Talk to your neurologist about whether staying on phenytoin-with careful monitoring-is safer than switching to something new.
What to Do Next
If you’re currently taking phenytoin:- Check your last blood level. When was it? Was it before or after a switch?
- Look at your prescription bottle. Is the name different from your last refill?
- Write down any new symptoms-dizziness, confusion, tremors, gum swelling.
- Call your doctor or pharmacist. Say: "I’m on phenytoin. I want to make sure my current formulation is safe. Can we check my level?"


Eddy Kimani - 2 December 2025
Phenytoin’s pharmacokinetics are a nightmare-zero-order metabolism, protein binding variability, narrow therapeutic window. It’s not just a drug, it’s a metabolic landmine. Most clinicians treat it like lisinopril, and that’s how people end up in the ICU. Therapeutic drug monitoring isn’t optional-it’s the only thing standing between seizure recurrence and cerebellar toxicity. The FDA’s 80-125% bioequivalence range is a joke for phenytoin. You wouldn’t swap out a carburetor in a jet engine and expect the same performance. Same logic applies here.
Chelsea Moore - 4 December 2025
OH MY GOD. I KNEW IT. I KNEW IT. I switched to generic phenytoin last year because my insurance ‘saved me’ $12 a month-and then I started having these terrifying tremors, like my brain was short-circuiting!!! I thought I was going crazy!!! I went to the ER and they told me my level was 47!!! FOURTY-SEVEN!!! I almost DIED because some pharmacy tech thought ‘generic’ meant ‘identical’!!! THIS IS A MASSACRE!!! PEOPLE ARE DYING BECAUSE OF COST-CUTTING!!!
John Biesecker - 6 December 2025
man. i just read this whole thing and my brain feels like it did a backflip. phenytoin is basically the edgy teenager of antiepileptics-works great but will totally ghost you if you look at it wrong. 🤯 and the fact that a tiny change in filler can mess with your entire nervous system? wild. i’m gonna start asking for my levels like i’m ordering a coffee-‘hey, can i get a trough, extra monitoring, no substitutions?’ ☕🧠
Genesis Rubi - 7 December 2025
generic drugs are a scam. america lets foreign factories make our life-saving meds with who-knows-what in them. the FDA is corrupted. dilantin was made by american scientists with american standards. now some chinese plant slaps ‘phenytoin’ on a pill and calls it bioequivalent? nope. my uncle had a seizure because of this. we need to ban generics for critical meds. america first. health first. not cheap pills from overseas.
Doug Hawk - 7 December 2025
the protein binding point is huge. i’ve seen patients with normal total phenytoin levels but low albumin from liver disease-free fraction was sky high, they were tremoring like they’d had too much caffeine. total level is meaningless without context. and yes, the trough draw matters. draw it 30 min before the next dose or you’re just guessing. also, if you’re on multiple meds? check interactions. fluconazole + phenytoin = bad day. simple as that.
Michael Campbell - 8 December 2025
they’re hiding this on purpose. big pharma wants you dependent on brand name. they know generics are risky but they don’t care. your insurance company doesn’t care. your pharmacist doesn’t care. they just want you to shut up and take the pill. they don’t want you asking questions. they want you to die quietly.
Victoria Graci - 9 December 2025
it’s like comparing two different brands of glue-both say ‘strong hold’ but one dries faster, one leaves a sticky residue, one makes your fingers fall off. phenytoin isn’t a commodity. it’s a delicate dance between your liver, your proteins, and your neurons. one misstep and the music stops. i think we treat it like a commodity because we’ve forgotten what medicine used to be: a sacred trust between patient and practitioner. now it’s a spreadsheet.
Saravanan Sathyanandha - 10 December 2025
in india, we have similar issues with antiepileptics-especially in rural areas where access to monitoring is limited. but the real tragedy is not just the science-it’s the lack of awareness. patients assume ‘same pill, same effect.’ we’ve started community education programs in clinics: ‘Check your level after switch, even if you feel fine.’ It’s not just about toxicity-it’s about dignity. Seizure control means independence. That’s worth more than a few rupees saved.
alaa ismail - 12 December 2025
so basically… don’t switch unless you’re ready to be a detective. and maybe keep a notebook. and ask for the test. and don’t ignore the gum swelling. also… maybe don’t drink whiskey while on this. got it.