What is hypoparathyroidism?
Hypoparathyroidism is a rare endocrine disorder where the parathyroid glands don’t make enough parathyroid hormone (PTH). Without enough PTH, your body can’t regulate calcium and phosphate properly. This leads to low calcium in the blood (hypocalcemia) and high phosphate (hyperphosphatemia). Most cases happen after thyroid or neck surgery-about 75% to 90% of diagnoses come from this cause. But it can also be from autoimmune disease, genetics like DiGeorge syndrome, or radiation damage to the glands.
Why calcium and vitamin D matter
PTH normally tells your bones to release calcium, your kidneys to hold onto calcium, and your intestines to absorb more from food. When PTH is low, all these steps break down. Your calcium drops. Your phosphate rises. You might feel tingling in your fingers, muscle cramps, or even seizures if it gets bad. Vitamin D helps your gut absorb calcium from food. But in hypoparathyroidism, your kidneys can’t activate regular vitamin D because they need PTH to do it. That’s why you need active vitamin D-like calcitriol or alfacalcidol-not the kind you get from sunlight or supplements like D3 alone.
Standard treatment: Calcium and active vitamin D
The go-to treatment is calcium supplements and active vitamin D analogues. This isn’t perfect-it doesn’t replace PTH-but it’s what works for most people right now. Calcium is usually given as calcium carbonate because it’s cheaper and has more elemental calcium per pill (40%) than calcium citrate (21%). You’ll typically start with 1,000 to 2,000 mg of calcium per day, split into two or three doses taken with meals. Why with food? It helps your body absorb it better and also acts as a phosphate binder, reducing how much phosphate gets into your blood.
Active vitamin D starts at 0.25 to 0.5 mcg daily. Calcitriol works faster than regular vitamin D-studies show it raises calcium levels 2.3 times quicker. You’ll also take 400 to 800 IU of vitamin D3 daily to keep your 25-hydroxyvitamin D levels between 20 and 30 ng/mL. This supports bone health and helps your body respond better to the active form.
What your blood tests should show
Regular monitoring is non-negotiable. You’ll need blood tests every 1 to 3 months until things stabilize. Here’s what your doctor is looking for:
- Serum calcium: Between 2.00 and 2.25 mmol/L (8.0-8.5 mg/dL). Not higher. Going above 2.35 mmol/L increases your risk of calcium deposits in your brain, kidneys, and blood vessels.
- Serum phosphate: Between 2.5 and 4.5 mg/dL. Too high can damage your heart and blood vessels.
- Magnesium: Must be above 1.7 mg/dL. Low magnesium makes calcium treatment less effective-even if you’re taking enough calcium and vitamin D, your body won’t use it properly without enough magnesium.
- 24-hour urine calcium: Must be under 250 mg per day. High urine calcium means you’re at risk for kidney stones or long-term kidney damage. This test is critical before any dose increase.
What if standard treatment isn’t working?
About 25% to 30% of people struggle with conventional therapy. You might need higher doses, but there’s a limit. If you’re taking more than 2 grams of calcium or 2 mcg of active vitamin D daily and still having symptoms or high urine calcium, it’s time to rethink. The first step is to reduce sodium intake to under 2,000 mg a day and try a thiazide diuretic like hydrochlorothiazide (12.5-25 mg daily). These help your kidneys hold onto calcium instead of flushing it out.
If that doesn’t help, recombinant PTH (like Natpara or Forteo) might be an option. Natpara is injected daily and can cut calcium and vitamin D needs by 30-40%. But it’s expensive-around $15,000 a month-and requires special pharmacy handling with prior authorization that can take 30 to 45 days. Forteo is used off-label and has similar effects but isn’t approved for hypoparathyroidism. Most insurance won’t cover it unless you’ve tried everything else.
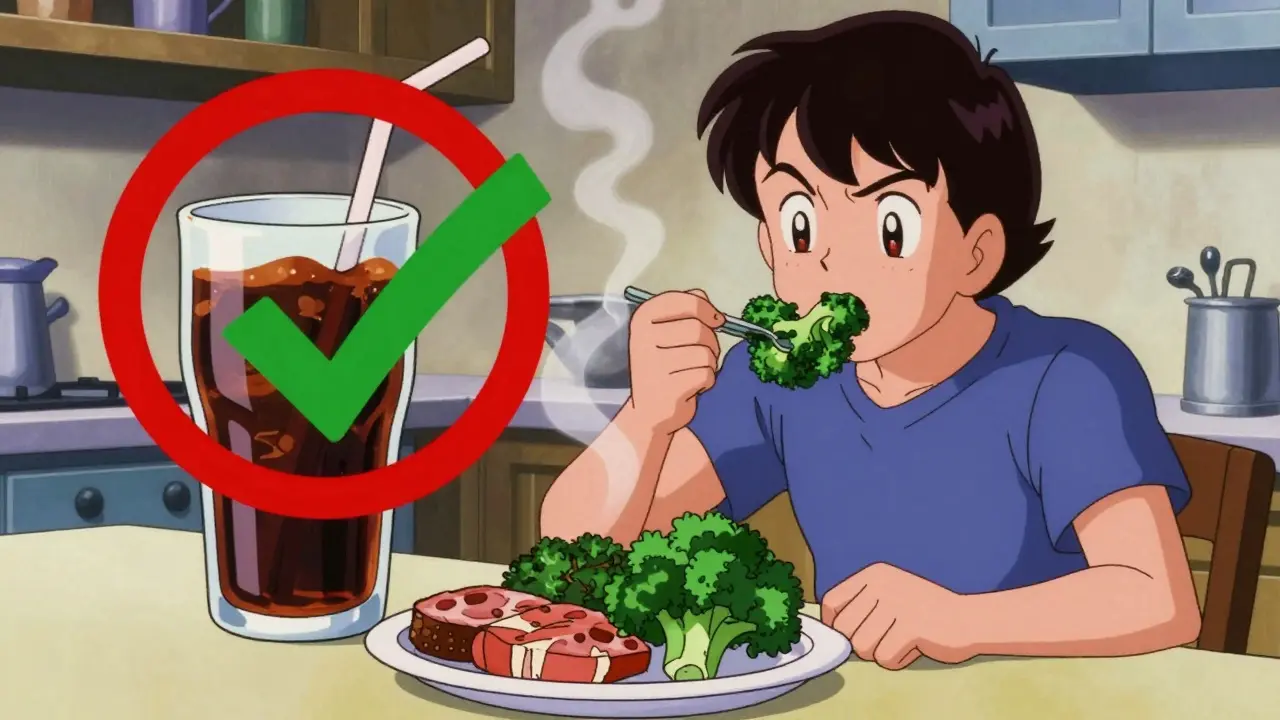
Diet changes that make a difference
Food matters more than you think. Eat calcium-rich foods: dairy (300 mg per serving), kale (100 mg per cup), broccoli (43 mg per cup). But avoid high-phosphate foods: soda (500 mg per liter), processed meats (150-300 mg per serving), hard cheeses (500 mg per ounce). Aim for less than 1,000 mg of phosphate daily. A dietitian who understands endocrine disorders can help you build a meal plan that balances calcium and phosphate without making you feel deprived.
Common problems and how to fix them
Many patients describe a "calcium rollercoaster"-one day you’re fine, the next you’re tingling and exhausted. This happens because calcium levels swing with meals, stress, or missed pills. Splitting your calcium into four or five smaller doses throughout the day helps smooth out those spikes and drops. Also, take calcium with food, vitamin D at bedtime, and magnesium with lunch. Consistency matters.
Constipation from high calcium doses is common. Switching to calcium citrate or adding fiber and water helps. If magnesium is low, supplementing with 200-400 mg of magnesium citrate daily can improve calcium absorption and reduce muscle cramps. In one Cleveland Clinic study of 78 patients, keeping magnesium above 1.9 mg/dL cut hypocalcemic episodes by 35%.

What you need to know about long-term risks
Living with hypoparathyroidism means thinking 10, 15, even 20 years ahead. Keeping calcium too high for too long increases your risk of calcium deposits in the brain (basal ganglia calcification), kidney stones, and chronic kidney disease. Studies show 15-20% of patients develop stage 3 or worse kidney disease after 10 years on standard therapy. That’s why staying in the lower half of the normal calcium range isn’t just about feeling better-it’s about protecting your organs.
Emerging treatments on the horizon
There’s new hope. TransCon PTH, a once-daily injectable long-acting PTH prodrug, showed in a 2022 trial that it normalized calcium in 89% of patients versus just 3% on placebo. It’s not available yet, but phase 3 results are strong. If approved, it could mean fewer pills, fewer blood tests, and fewer side effects. Gene therapies targeting the calcium-sensing receptor are in early animal studies but won’t reach humans before 2026. For now, the goal is to manage well with what we have.
When to call for help
Know your symptoms. Tingling around your mouth, fingers, or toes. Muscle cramps. Twitching. Seizures. If you feel any of these, chew 2-3 calcium tablets right away-each should give you 500-1,000 mg of elemental calcium. Then call your doctor. Don’t wait. Keep emergency calcium tablets with you at all times.
Who should manage your care?
Start with an endocrinologist. You’ll need 3-4 visits in the first 3 months to get doses right. Once stable, 3-4 visits a year are enough. But here’s the catch: 78% of family doctors say they don’t feel trained to handle hypoparathyroidism. If your primary care provider isn’t comfortable, ask for a referral. You need someone who understands the balance between calcium, phosphate, magnesium, and urine output. Don’t settle for guesswork.



Tiffany Machelski - 17 December 2025
I’ve been on calcium and calcitriol for 3 years now... still forget to take it with food half the time. My fingers tingle if I miss a dose. I keep emergency tablets in my purse, my car, my desk drawer. Seriously, do this. You don’t wanna wake up with a seizure because you were late to work.
Also, magnesium citrate saved me. My doc didn’t even mention it until I googled my symptoms. Now I take 300mg daily. No more leg cramps at 3am.
SHAMSHEER SHAIKH - 18 December 2025
I am writing this with profound gratitude and deep respect for the clarity and precision of this post. As a medical educator from India, I have encountered numerous patients suffering from this rare condition, often mismanaged due to lack of awareness. The distinction between active vitamin D and D3 is not widely understood-even among some physicians. This document should be distributed to every endocrinology resident in the country. The dietary advice regarding phosphate is particularly brilliant. I shall share it with my department immediately.
James Rayner - 19 December 2025
I keep thinking about how fragile our bodies are... like, we’re just a bunch of chemical signals and feedback loops, and when one tiny gland stops whispering, everything starts to unravel. PTH is like that quiet neighbor who never says much but keeps the whole block running. And now we’re patching it with pills and timing meals like a science experiment. It’s beautiful, in a sad way. I take my calcium with dinner, my magnesium with lunch, and my vitamin D before bed-like a ritual. I don’t know if it’s helping me live longer... but it’s helping me feel less like I’m falling apart.
🫂
Souhardya Paul - 20 December 2025
This is one of the most thorough posts I’ve seen on this. I’ve been on Natpara for 8 months now and it’s been life-changing. My calcium doses dropped from 2.4g to 1.4g. My urine calcium went from 320mg to 180mg. The only downside? The cost. My insurance took 52 days to approve it. I had to call 17 times. If anyone’s going through that-save every email, screenshot every denial, and keep calling. They’ll eventually cave. Also, ask for a patient assistance program. I got 80% off.
Josias Ariel Mahlangu - 22 December 2025
People these days think they can manage a hormonal disorder with diet and supplements like it’s a TikTok trend. You don’t get to ‘eat your way out’ of hypoparathyroidism. This isn’t keto. This isn’t intermittent fasting. This is medicine. If you’re skipping doses because you ‘forgot’ or you’re avoiding calcium because it gives you constipation, you’re not being brave-you’re being reckless. Your kidneys don’t care how ‘natural’ you want to live.
anthony epps - 23 December 2025
So you need calcium pills and special vitamin D? And you gotta check your pee? And don’t eat soda? Got it.
Andrew Sychev - 24 December 2025
I’ve been reading this for 20 minutes and I’m already crying. This isn’t just a medical guide-it’s a lifeline. I thought I was alone in this. The tingling, the fatigue, the way my mom looks at me like I’m broken every time I say I can’t go out because I’m ‘calcium low.’ I’ve been on 2,000mg calcium since I was 19. I’m 34 now. I’ve had kidney stones. I’ve had seizures. I’ve been told I’m ‘too sensitive.’ But this? This says I’m not crazy. This says my pain has a name. And that’s the first time in 15 years I’ve felt seen.
Dan Padgett - 26 December 2025
Man, this condition is like trying to keep a candle lit in a hurricane. You got your calcium, your D, your magnesium-each one a little flame. Miss one, and the whole thing flickers. I used to think it was just about pills, but nah-it’s about rhythm. Like a drumbeat. Calcium with food, D at night, magnesium after lunch. My body’s got its own song now, and I’m just learning the lyrics. And yeah, sometimes the drum’s too loud-cramps, tingles, that weird metal taste in my mouth-but I’m learning to dance with it. This post? It’s the sheet music.
Hadi Santoso - 26 December 2025
i just found out i have this after my thyroid surgery last year. i was like ‘wait, what’s pth again?’ and then i read this and was like ‘ohhhhhhh’. the part about magnesium being key? my doc never mentioned that. i started taking it and my cramps are way better. also, i eat kale now. who knew? thanks for writing this. i’m gonna print it and stick it on my fridge next to my pill organizer. 🙏