When you’re facing cancer surgery, one of the most confusing decisions isn’t about the operation itself-it’s about when to give the drugs. Should treatment come before surgery to shrink the tumor? Or after, to clean up what’s left? This isn’t just a medical detail-it’s a turning point in your care. And the answer isn’t the same for everyone.
What Neoadjuvant Therapy Really Means
Neoadjuvant therapy means giving chemotherapy, immunotherapy, or both before surgery. It’s not about delaying the operation-it’s about using that time to your advantage. The goal? Shrink the tumor so it’s easier to remove, kill hidden cancer cells early, and see how your body responds before cutting into you.This approach really took off in the last decade, especially for lung and breast cancers. In non-small cell lung cancer (NSCLC), the CheckMate 816 trial showed that adding the immunotherapy drug nivolumab to chemotherapy before surgery led to a pathologic complete response (pCR)-meaning no live cancer cells were found in the removed tissue-in 24% of patients. That’s up from just 2.2% with chemo alone. And those who achieved pCR had a 37% lower risk of their cancer coming back within two years.
For triple-negative breast cancer, neoadjuvant chemo works similarly. About 30-40% of patients achieve pCR, and those patients are far more likely to live longer than those whose tumors don’t shrink. That’s why doctors now use response to neoadjuvant treatment as a real-time guide. If the tumor vanishes, you might need less after surgery. If it doesn’t budge, you know you’re dealing with a tougher cancer-and can switch tactics faster.
What Adjuvant Therapy Is For
Adjuvant therapy happens after surgery. It’s the cleanup crew. Even if the surgeon removes every visible tumor, there could still be stray cancer cells hiding in your body. Adjuvant treatment aims to kill those before they grow into new tumors.This has been the standard for decades, especially in breast cancer. For years, patients got chemo or hormone therapy after surgery, hoping to prevent recurrence. The logic was simple: remove the tumor, then hit the rest with drugs.
But here’s the catch: you never know if the drugs are working. You can’t see the cancer cells dying. You just wait-and worry. A patient might go through six months of chemo, only to find out later the cancer came back. There’s no feedback loop. No way to adjust.
Why Timing Matters More Than You Think
The big question isn’t just “before or after?” It’s “when does it matter most?”For NSCLC, the latest data from a 2024 meta-analysis of over 3,200 patients shows something surprising: giving immunotherapy only before surgery (neoadjuvant-only) works just as well as giving it before AND after (neoadjuvant-adjuvant). But the side effects? Much worse with two rounds. Nearly 30% of patients on the two-phase approach had serious reactions like lung inflammation or liver damage. With neoadjuvant-only? Around 18%.
That’s not a small difference. It’s the difference between spending recovery in the hospital and being home with your family. Dr. Mark Awad from Dana-Farber put it bluntly: “The adjuvant phase may be unnecessary.”
In breast cancer, the picture is more mixed. Studies show survival rates are similar whether you get chemo before or after surgery. But neoadjuvant therapy gives you something adjuvant can’t: information. If your tumor responds well, you know you’re on the right track. If it doesn’t, your oncologist can change your plan before it’s too late.
One patient in Melbourne told her oncologist she chose neoadjuvant therapy because she wanted to know “if the drugs would work before they cut me open.” She got a 90% tumor kill. That gave her peace of mind. Her surgery was less invasive. She didn’t need radiation. And she avoided months of post-op chemo.
Who Gets Which Approach?
It’s not random. Doctors use clear guidelines to decide.For NSCLC, the National Comprehensive Cancer Network (NCCN) recommends neoadjuvant chemoimmunotherapy for stage IB (tumors 4 cm or larger) through stage IIIA. You need to be healthy enough to handle chemo and immunotherapy before surgery. If you’re older or have heart or lung problems, adjuvant might be safer.
In breast cancer, neoadjuvant therapy is standard for:
- Triple-negative subtype
- HER2-positive tumors
- Large hormone-receptor-positive tumors where shrinking the mass helps avoid mastectomy
For smaller, low-risk tumors, adjuvant therapy is still common. But even there, the trend is shifting. More centers are offering neoadjuvant options because of the insight it provides.
And it’s not just about cancer type. Your PD-L1 status matters. If your tumor expresses PD-L1 at 1% or higher, immunotherapy is more likely to help. That’s tested before treatment starts. No guesswork.
The Real Trade-Offs
No treatment is perfect. Both approaches have risks.With neoadjuvant therapy, you might wait 9-12 weeks before surgery. During that time, your cancer could grow. About 5-10% of NSCLC patients see progression. Some need emergency surgery because the tumor spreads. And if you develop serious side effects-like colitis or pneumonia-you might have to delay surgery. That adds stress.
Adjuvant therapy avoids that delay. But it’s a gamble. You’ve already been cut open. You’re recovering. And now you’re hit with chemo or immunotherapy, which can slow healing, cause fatigue, or trigger long-term issues like nerve damage or heart problems. And again-you don’t know if it’s working.
One 2023 survey found 62% of NSCLC patients on neoadjuvant therapy felt anxious about waiting. But 78% said knowing their tumor responded made them feel more in control.
What’s Changing Right Now
This field is moving fast. In 2022, the FDA approved nivolumab with chemo for neoadjuvant use in NSCLC. Then it approved nivolumab again as adjuvant therapy. But new data is already challenging that two-step approach.Trials like KEYNOTE-867 are now comparing neoadjuvant-only vs. neoadjuvant + adjuvant head-to-head. Preliminary results suggest the second round might not add benefit-it just adds risk.
Another breakthrough? Circulating tumor DNA (ctDNA). This blood test can detect leftover cancer cells after surgery. If ctDNA is still present, you get more treatment. If it’s gone? You might skip adjuvant therapy entirely. Twelve trials are testing this right now. Within five years, it could become standard.
For EGFR-mutant lung cancer, the NeoADAURA trial is testing osimertinib before surgery. Early data suggests it could cut recurrence risk by more than half. That’s a game-changer for a group that used to have few options.
What You Should Ask Your Doctor
If you’re facing surgery, here’s what to ask:- Is neoadjuvant therapy an option for my cancer type and stage?
- What’s my PD-L1 status? Does that change my choices?
- What’s the chance I’ll get a pathologic complete response?
- What are the risks of waiting for surgery? What if the tumor grows?
- Will we test for ctDNA after surgery? Could that guide my next steps?
- Are you following NCCN or ASCO guidelines on sequencing?
Don’t assume your oncologist has a preference. Ask why they’re recommending one path over another. The answer might surprise you.
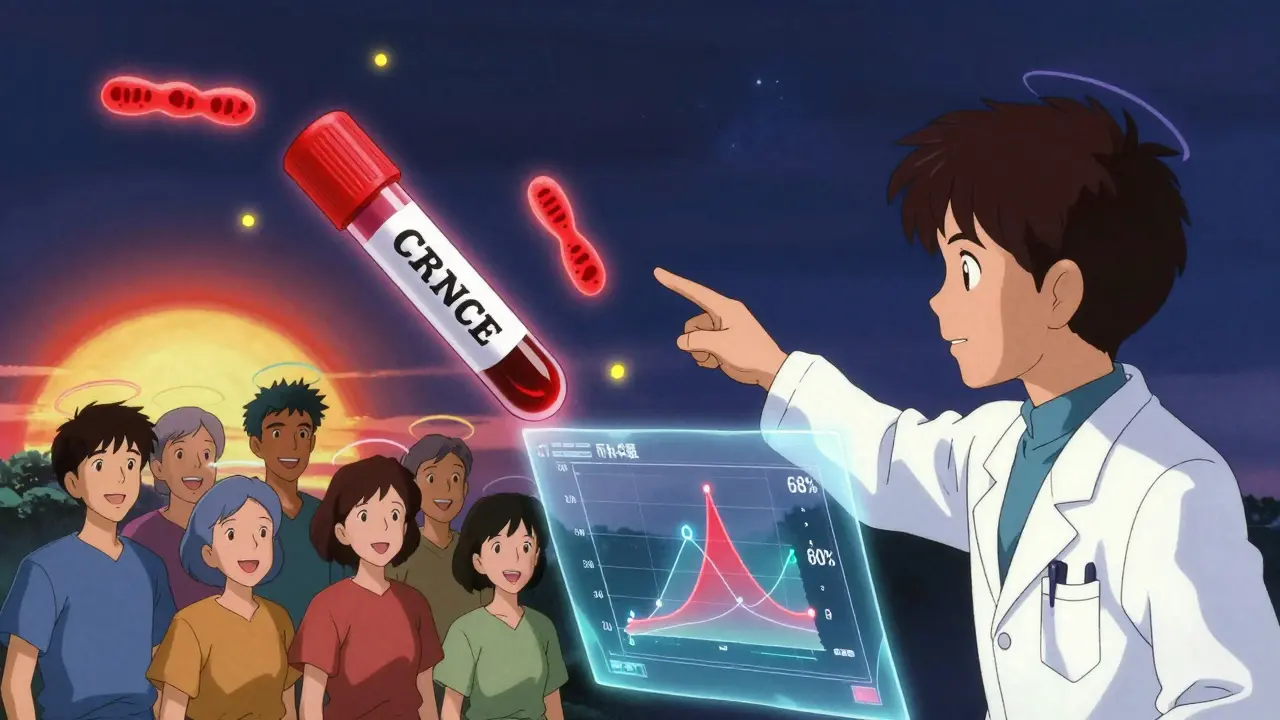
What This Means for the Future
The future of cancer treatment isn’t just about stronger drugs. It’s about smarter sequencing.Neoadjuvant therapy isn’t replacing adjuvant therapy-it’s redefining it. Instead of giving drugs blindly after surgery, we’re using the pre-surgery window to test, learn, and personalize. That’s powerful.
By 2030, experts predict optimized sequencing could boost 5-year survival for early-stage lung cancer from 68% to 80%. That’s 15,000-20,000 more lives saved every year in the U.S. alone.
It’s not magic. It’s science. And it’s happening right now-in Melbourne, in Sydney, in Boston, in London. The question isn’t whether you’ll hear about it. It’s whether you’ll ask the right questions before your next appointment.
Is neoadjuvant therapy better than adjuvant therapy?
Neither is universally better. Neoadjuvant therapy gives you early insight into how your tumor responds and can shrink tumors for easier surgery. Adjuvant therapy cleans up leftover cells after surgery. For many cancers-especially NSCLC and triple-negative breast cancer-neoadjuvant therapy now matches or improves survival while offering more personalization. But for smaller, low-risk tumors, adjuvant therapy remains effective and avoids treatment delays.
Can I skip surgery if neoadjuvant therapy works?
No. Even if your tumor disappears on scans or shows a pathologic complete response (pCR), surgery is still the standard. Cancer cells can hide in places imaging can’t see. Removing the tumor bed ensures no living cells remain. However, researchers are studying whether some patients with near-total response and negative ctDNA might avoid surgery in the future.
How long does neoadjuvant therapy last before surgery?
Typically 3 to 4 cycles over 9 to 12 weeks. For lung cancer, this often means three weeks of chemo and immunotherapy, followed by a one-week break, repeated three or four times. Surgery is scheduled 3 to 6 weeks after the last dose to let your body recover from side effects.
Does adjuvant therapy work better if started right after surgery?
Yes. Starting adjuvant therapy within 8 weeks after surgery gives the best chance to target lingering cancer cells before they spread. Delays beyond 12 weeks reduce effectiveness. That’s why timing matters-whether you’re doing neoadjuvant or adjuvant, coordination between your surgical and oncology teams is critical.
Why is immunotherapy used before surgery for lung cancer?
Immunotherapy helps your immune system recognize and attack cancer. Giving it before surgery exposes your immune system to the full tumor, making it more active and better prepared to fight remaining cells. The CheckMate 816 trial showed this approach doubled the rate of complete tumor disappearance compared to chemo alone-and cut the risk of recurrence by 37%.
What if I don’t respond to neoadjuvant therapy?
If your tumor doesn’t shrink or shows signs of resistance, your oncologist may change your plan. You might switch drugs before surgery, add radiation, or prepare for a more extensive operation. In some cases, you’ll still get adjuvant therapy after surgery, but it will be tailored to your tumor’s behavior. The key is that neoadjuvant therapy gives you this information-adjuvant therapy alone does not.
Next Steps If You’re Considering Treatment Options
If you’re facing cancer surgery, here’s what to do next:- Ask for a multidisciplinary tumor board review-this includes surgeons, oncologists, and radiologists who specialize in your cancer type.
- Request PD-L1 testing and, if available, ctDNA analysis before treatment starts.
- Ask if your hospital follows NCCN guidelines for sequencing.
- Find out if your center participates in clinical trials for neoadjuvant or ctDNA-guided therapy.
- Don’t rush. Take time to understand your options. This isn’t a decision you make in one appointment.
The goal isn’t just to survive cancer. It’s to survive it with less treatment, less toxicity, and more control. Neoadjuvant therapy isn’t the only path-but for many, it’s the smartest one yet.


Nilesh Khedekar - 16 January 2026
So let me get this straight-we’re now giving people chemo and immunotherapy BEFORE cutting them open, just so we can watch if the tumor cries? And we call this medicine? In India, we still believe in letting the body fight first, then hitting it with the big guns. But hey, if you wanna turn your chest into a science experiment, go ahead. I’ll be over here, sipping chai and praying for your immune system.
RUTH DE OLIVEIRA ALVES - 16 January 2026
It is imperative to recognize that the clinical data supporting neoadjuvant therapy, particularly in non-small cell lung cancer, demonstrates statistically significant improvements in pathologic complete response rates, as evidenced by the CheckMate 816 trial. Moreover, the reduction in recurrence risk by 37% is not merely an anecdotal observation but a reproducible outcome validated across multiple centers. The adoption of such protocols must be guided by evidence-based guidelines, including those issued by the National Comprehensive Cancer Network.
Crystel Ann - 17 January 2026
I had a friend go through neoadjuvant therapy for triple-negative breast cancer. She got the pCR, and honestly? It changed everything. She didn’t need radiation, her surgery was smaller, and she didn’t spend months feeling like garbage after. It gave her back some control. I know it’s not magic, but for some people? It’s the first real hope they’ve had since diagnosis.
Jan Hess - 19 January 2026
This is the future right here. We’re not just throwing drugs at cancer anymore-we’re listening to it. If the tumor shrinks? Great. If it doesn’t? We pivot. No more guessing after surgery. This isn’t just smarter-it’s kinder. More people are going home faster, with less damage. Let’s stop treating patients like lab rats and start treating them like humans who deserve to know what’s working
Iona Jane - 20 January 2026
They say neoadjuvant therapy is about personalization but what they’re really doing is turning cancer into a corporate profit model. Who pays for all these fancy ctDNA tests? Who gets rich off the two-year waiting game? The hospitals. The pharma giants. The oncologists on commission. Meanwhile, you’re the one lying awake wondering if the drugs are killing you faster than the cancer
Jaspreet Kaur Chana - 21 January 2026
Bro, in India we’ve been doing this for years without all the fancy jargon. My cousin got chemo before surgery for lung cancer, and the doc said if it works, you get less cut, less pain, less time in bed. If it doesn’t, we switch fast. No waiting till after you’re stitched up to find out you wasted six months. This isn’t rocket science, it’s common sense. Why are Americans making it sound like a breakthrough when it’s just good medicine? Also, nivolumab costs more than a car here but we still do it because we don’t have a choice. You guys just need to stop overcomplicating things
Ayush Pareek - 23 January 2026
If you’re facing this decision, don’t rush. Ask for the tumor board. Push for PD-L1 and ctDNA testing. And if your doctor says, ‘It’s standard,’ ask why. There’s no one-size-fits-all here. Your body, your cancer, your timeline. You deserve to know the data behind the plan. This isn’t just treatment-it’s strategy. And you’re not a patient, you’re the captain of your own ship.
Amy Ehinger - 23 January 2026
I read this whole thing while waiting for my mom’s oncology appointment. She’s got stage IIA breast cancer and they’re talking adjuvant. I showed her the part about neoadjuvant giving you feedback before surgery. She started crying-not from fear, but because she finally felt like someone was listening. We asked for a second opinion. They agreed to try neoadjuvant. I don’t know if it’ll work, but for the first time, we feel like we’re part of the plan, not just along for the ride.
Nat Young - 24 January 2026
Let’s be real-neoadjuvant therapy is just the latest placebo wrapped in a clinical trial. The 37% recurrence reduction? Probably because they excluded the patients who got worse. And ctDNA? That’s still experimental. If it were reliable, we wouldn’t need surgery at all. This whole thing feels like pharma’s way of selling more drugs under the guise of innovation. Wake up. Surgery is still the cure. Everything else is just noise.
Haley Graves - 24 January 2026
My oncologist told me if I didn’t respond to neoadjuvant, we’d adjust before surgery. That’s the power here-you’re not stuck. You’re not praying after the knife. You’re adapting while you still have time. I had a 95% tumor kill. My surgery was a walk in the park. I didn’t need radiation. I’m back at work. This isn’t theoretical. It’s real. And if your doctor isn’t offering this, ask why. You’re worth the extra effort.
Diane Hendriks - 25 January 2026
Neoadjuvant therapy is a globalist scam. America used to be the leader in cancer care. Now we’re letting the WHO and Big Pharma dictate how we treat our own people. Why are we giving foreign drugs before surgery? Why not just cut it out and let the body heal? We used to be strong. Now we’re test subjects for international protocols that benefit no one but the elites. Wake up, Americans. This isn’t medicine-it’s control.
Sohan Jindal - 26 January 2026
They say surgery is still needed even if the tumor is gone. But what if the doctors are lying? What if they just want to keep cutting? I heard a guy on YouTube say the whole thing is a money scheme. They cut you open to make you pay more. I’m not doing it. I’m going natural. Turmeric. Fasting. Prayer. If God wants me to live, I’ll live. No scalpel. No chemo. No lies.