Why High Triglycerides Are More Dangerous Than You Think
Most people know high cholesterol is bad for the heart. But few realize that high triglycerides can be just as dangerous - and in some cases, even more immediate. While cholesterol builds up in arteries over years, triglycerides can trigger a sudden, life-threatening attack on your pancreas. And if left unchecked, they’re also quietly increasing your risk of heart attack and stroke.
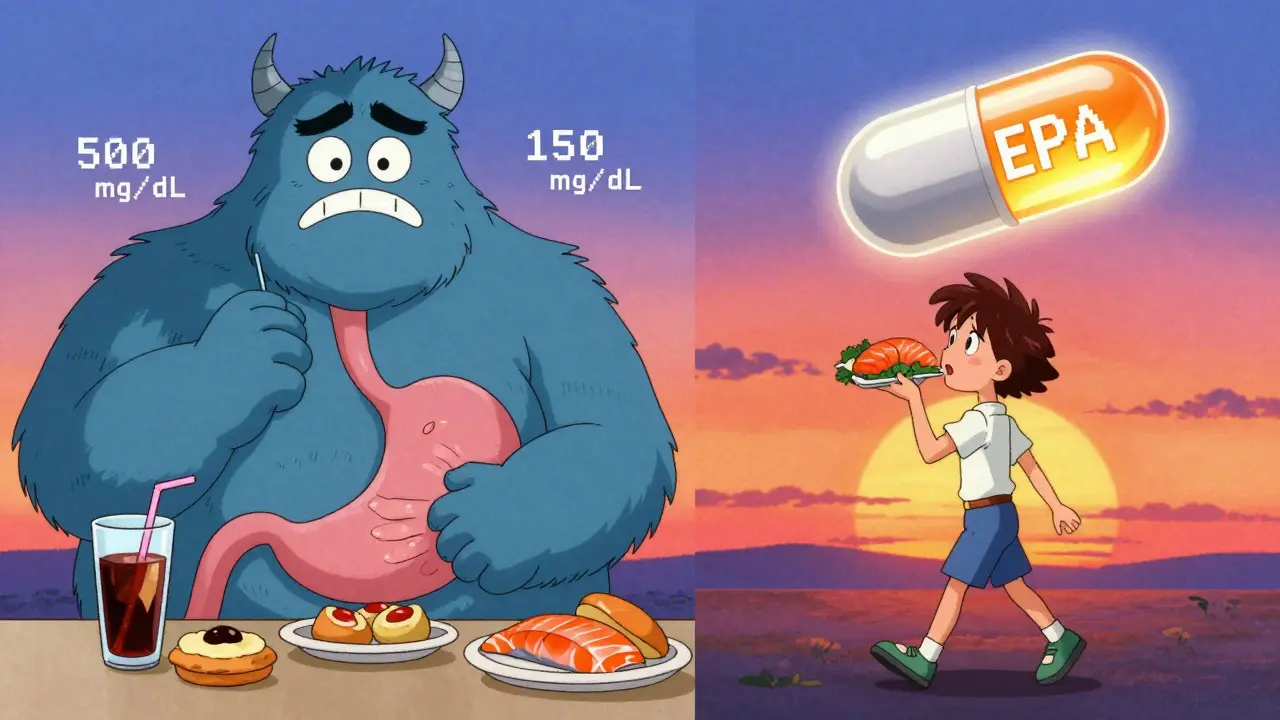
Triglycerides are the most common type of fat in your blood. When you eat more calories than your body needs right away, it turns the extra into triglycerides and stores them in fat cells. That’s normal. But when levels climb above 150 mg/dL, you’re in the danger zone. At 500 mg/dL and above, your risk of acute pancreatitis jumps dramatically. At 1,000 mg/dL or higher, one in ten people will develop it. And if your levels hit 2,000 mg/dL or more, that risk doubles.
What makes this so scary is that you might feel fine until you don’t. No chest pain. No warning signs. Just sudden, severe abdominal pain, nausea, vomiting - and a hospital trip. And for many, this isn’t a one-time event. Recurrent pancreatitis can permanently damage your pancreas, leading to diabetes or digestive failure.
The Link Between Triglycerides and Pancreatitis: It’s Not What You Think
Triglycerides themselves don’t hurt your pancreas. It’s what happens when your body tries to break them down.
When triglyceride levels spike, your blood fills with large fat particles called chylomicrons. These are too big to pass easily through the tiny capillaries in your pancreas. They clog the flow, causing oxygen starvation in the tissue. At the same time, enzymes in the pancreas start breaking down these fat particles into free fatty acids - and those acids are toxic. They burn through cell membranes, trigger inflammation, and activate clotting systems that can shut down blood flow entirely.
Studies show that even mild elevations - like 177 mg/dL - raise your risk of pancreatitis over time. But the real danger kicks in above 500 mg/dL. At that point, your pancreas is under constant stress. And if you have other risk factors - like uncontrolled diabetes, heavy alcohol use, or certain medications - your levels can skyrocket overnight.
Some people with triglycerides over 10,000 mg/dL never get pancreatitis. Others have an episode at 400 mg/dL. Why? Genetics, metabolism, and how fast your body clears fat from the blood all play a role. That’s why blanket rules don’t always work. You need to know your personal risk profile.
Heart Protection: Lowering Triglycerides Saves Lives
While pancreatitis is the emergency, heart disease is the silent killer. People with persistently high triglycerides have a 70% higher chance of dying from cardiovascular causes than those with normal levels.
High triglycerides often come with other problems: low HDL (good cholesterol), small dense LDL particles, and insulin resistance. Together, they create a perfect storm for artery damage. That’s why reducing triglycerides isn’t just about avoiding pancreatitis - it’s about preventing heart attacks and strokes years down the line.
Recent research confirms this. The REDUCE-IT trial showed that taking 4 grams of pure EPA (a type of omega-3 fatty acid) daily cut heart attacks, strokes, and cardiovascular deaths by 25% in high-risk patients. But not all omega-3s work the same. Combination formulas (EPA + DHA) didn’t show the same benefit. Precision matters.
Statins help lower LDL, but they only reduce triglycerides by 20-30%. For people with levels above 500 mg/dL, that’s not enough. Fibrates - like fenofibrate - are more targeted. They can slash triglycerides by 40-50%. And when combined with omega-3s, the effect is even stronger.
When to Act: The Real Triggers and Thresholds
There’s no single number that fits everyone. But here’s what the experts agree on:
- 150-199 mg/dL: Borderline high. Focus on diet and exercise.
- 200-499 mg/dL: High. Add a statin if you have other heart risks (like high blood pressure or smoking).
- 500-999 mg/dL: Very high. Start fibrate therapy. Avoid alcohol and sugar. Monitor closely.
- 1,000+ mg/dL: Severe. This is a medical emergency. You need medication now to prevent pancreatitis.
But here’s the twist: many doctors still rely on fasting triglyceride tests. New guidelines from the European Society of Cardiology say nonfasting levels above 177 mg/dL are enough to trigger action. Why? Because most people eat before their blood is drawn. A nonfasting test reflects real-life conditions better.
If you’re diabetic, overweight, or take estrogen pills or certain antivirals, your triglycerides can spike even if you eat well. That’s why checking your levels regularly - especially if you have a family history - isn’t optional. It’s essential.
What Actually Works: Lifestyle Changes That Move the Needle
Medication helps, but lifestyle changes are the foundation. And they work faster than most people think.
Eliminate added sugar and refined carbs. A single can of soda can raise triglycerides by 30% in hours. Cut out sugary drinks, white bread, pastries, and processed snacks. Replace them with whole grains, vegetables, legumes, and lean proteins.
Go low-fat - but not zero-fat. You need healthy fats. But saturated and trans fats (fried foods, butter, processed meats) make triglycerides worse. Swap them for olive oil, avocados, nuts, and fatty fish like salmon or mackerel. Aim for 2-3 servings of fish per week.
Exercise daily. Just 30 minutes of brisk walking five times a week can lower triglycerides by 20-30%. You don’t need to run a marathon. Consistency beats intensity.
Stop drinking alcohol. Alcohol is one of the fastest ways to spike triglycerides. Even moderate drinking - two drinks a day - can raise levels by 200-400%. If your triglycerides are above 500 mg/dL, cut it out completely.
Lose 5-10% of your body weight. That’s not even a dramatic loss. For someone who weighs 200 pounds, that’s 10-20 pounds. It can reduce triglycerides by up to 50%.
These changes take 6-8 weeks to show full effect. That’s why doctors often prescribe medication while you’re making lifestyle changes - to bridge the gap and protect you immediately.
Medications That Actually Work (And Which Ones to Avoid)
Not all triglyceride-lowering drugs are created equal.
- Fibrates (fenofibrate, gemfibrozil): First-line for levels over 500 mg/dL. Reduce triglycerides by 40-50%. Safe for most people, but can interact with statins. Monitor liver and kidney function.
- Pure EPA omega-3 (icosapent ethyl): Only FDA-approved for cardiovascular risk reduction in high-triglyceride patients. Dose: 4 grams daily. Reduces heart events by 25%. Avoid fish oil supplements - they’re not the same.
- Statins (atorvastatin, rosuvastatin): Best for lowering LDL, but help triglycerides too. Use them if you have high cholesterol or heart disease risk.
- Pemafibrate (K-877): Newer drug, approved in 2023. More effective than fenofibrate in some studies. Not yet widely available.
- Volanesorsen: For rare genetic disorder (familial chylomicronemia syndrome). Reduces triglycerides by 80%. Costs over $450,000 a year. Insurance rarely covers it.
Don’t waste money on over-the-counter omega-3 fish oil pills. Most contain EPA and DHA in low doses. They don’t lower triglycerides enough to matter - and they can increase bleeding risk at high doses. Stick to prescription-grade EPA only.

What Doesn’t Work - And Why So Many People Fail
Here’s the hard truth: most people with high triglycerides don’t get better - not because they’re lazy, but because the advice they get is wrong.
Many are told to eat a “low-fat diet.” But if that means swapping butter for low-fat cookies and cereal, you’re just replacing fat with sugar. And sugar turns directly into triglycerides.
Others try to cut fat completely. That backfires. Your body needs fat to absorb vitamins and make hormones. Too little fat can cause your liver to overproduce triglycerides.
And then there’s the myth that “natural remedies” work. Garlic, flaxseed, apple cider vinegar - none have proven effect on triglycerides above 500 mg/dL. They might help a little if your levels are borderline. But if you’re at risk for pancreatitis, you need science-backed treatment.
Even worse: 32% of primary care doctors say they’re not confident managing severe hypertriglyceridemia. That means patients get delayed care, misdiagnosed as having alcohol-related pancreatitis, or told to “just eat less.”
If your triglycerides are above 500 mg/dL, you need a specialist - a lipidologist or endocrinologist. Don’t wait for your primary care doctor to figure it out. Ask for a referral.
Real Stories: What Patients Actually Experience
One woman in Melbourne, 54, had her first pancreatitis attack after a weekend of holiday feasting. Her triglycerides were 3,200 mg/dL. She’d been told her cholesterol was fine, so she never checked triglycerides. She spent a week in ICU. Now she’s on fenofibrate and strict diet. She says the hardest part isn’t the food - it’s the loneliness. “No one understands why I can’t have a glass of wine or a slice of cake at family dinners.”
A man in his 40s with type 2 diabetes had triglycerides of 2,100 mg/dL. He was told to “cut carbs.” He did - but kept eating rice, pasta, and fruit juice. His levels didn’t budge. Only when he eliminated all added sugar and started walking daily did his numbers drop by 60% in 10 weeks.
Another patient, diagnosed with familial chylomicronemia syndrome, tried everything - diet, statins, fibrates. Nothing worked. His triglycerides stayed above 10,000 mg/dL. He was on the verge of another pancreatitis episode when he got access to volanesorsen. Within six months, his levels dropped to 457 mg/dL. He hasn’t had another attack.
These aren’t rare cases. They’re the rule.
What You Should Do Right Now
If you’ve never checked your triglycerides - get a lipid panel done. Ask for fasting and nonfasting results. Don’t assume your cholesterol test covers it.
If your triglycerides are above 150 mg/dL:
- Stop sugary drinks and processed carbs.
- Replace saturated fats with olive oil, nuts, and fatty fish.
- Walk 30 minutes every day.
- Avoid alcohol completely.
- Get your HbA1c tested if you’re overweight or have prediabetes.
If your triglycerides are above 500 mg/dL:
- See a lipid specialist immediately.
- Start fibrate therapy as directed.
- Use prescription EPA omega-3 (not fish oil).
- Check your levels every 2-4 weeks until stable.
- Get a referral to a dietitian who understands metabolic health.
This isn’t about perfection. It’s about control. High triglycerides are one of the most treatable risk factors in medicine. With the right plan, you can avoid pancreatitis, protect your heart, and live a full, active life.
Can high triglycerides cause heart attacks?
Yes. High triglycerides are linked to a 70% higher risk of dying from heart disease. They contribute to plaque buildup, inflammation, and blood clotting - all key drivers of heart attacks and strokes. Lowering them reduces that risk significantly.
How long does it take to lower triglycerides naturally?
You can see a 20-30% drop in 2-4 weeks with strict diet and exercise. A 50% reduction usually takes 8-12 weeks. Medication can speed this up - especially if levels are above 500 mg/dL.
Is it safe to take omega-3 supplements for high triglycerides?
Only prescription-grade pure EPA (icosapent ethyl) is proven to reduce heart risk. Over-the-counter fish oil supplements don’t lower triglycerides enough and can increase bleeding risk at high doses. Don’t substitute them for medical treatment.
Can I drink alcohol if my triglycerides are high?
No. Alcohol raises triglycerides by 200-400% within hours. Even one drink can trigger a spike. If your levels are above 500 mg/dL, alcohol is a direct threat to your pancreas. Complete avoidance is the only safe option.
Do I need to fast before a triglyceride test?
Traditionally, yes - 9-12 hours without food. But newer guidelines accept nonfasting levels above 177 mg/dL as a risk signal. If your doctor only checks fasting levels, ask for a nonfasting test too. It gives a more realistic picture of your daily risk.
What’s the difference between triglycerides and cholesterol?
Cholesterol is used to build cells and hormones. Triglycerides store excess energy. High cholesterol leads to clogged arteries over time. High triglycerides can cause sudden pancreatitis and also increase heart disease risk. Both matter - but triglycerides are often ignored.
Are there genetic causes of high triglycerides?
Yes. Familial chylomicronemia syndrome (FCS) is a rare genetic disorder that causes triglycerides to soar above 10,000 mg/dL. People with FCS are at extreme risk for pancreatitis and need specialized treatment like volanesorsen. But most cases are caused by diet, obesity, diabetes, or alcohol - not genes.
Can stress raise triglycerides?
Not directly. But chronic stress leads to poor sleep, emotional eating, and higher cortisol - which increases fat storage and insulin resistance. All of that pushes triglycerides up. Managing stress through sleep, movement, and mindfulness helps - but it’s not a substitute for diet and medication.
What foods should I avoid with high triglycerides?
Avoid sugar (soda, candy, baked goods), refined carbs (white bread, pasta, rice), fried foods, processed meats, and alcohol. Also limit saturated fats like butter, cream, and coconut oil. Focus on vegetables, legumes, whole grains, lean proteins, and healthy fats like olive oil and avocado.
Is there a cure for high triglycerides?
There’s no permanent cure - but there’s excellent control. With diet, exercise, and medication when needed, most people can bring triglycerides down to safe levels and stay there for life. The key is consistency, not perfection.




Christina Bischof - 15 December 2025
I had no idea triglycerides could do this much damage. My doc never mentioned it when I got my cholesterol test. I just thought "low fat" meant no butter and I was good to go. Turns out my daily smoothie with honey and banana was basically a triglyceride bomb. Changed my habits last month and my numbers dropped 40%. Still can’t believe I didn’t know this sooner
Jocelyn Lachapelle - 15 December 2025
This is such an important post 🙌 I’ve seen so many people think "if I don’t have chest pain I’m fine" - but this? This is silent sabotage. My aunt had her first pancreatitis attack at 52 and thought it was just food poisoning. Turns out her triglycerides were 4,200. She’s on meds now and lives differently. No more wine, no more pastries. It’s hard but worth it
Mike Nordby - 17 December 2025
The REDUCE-IT trial data is robust and consistently replicated. The distinction between prescription-grade icosapent ethyl and over-the-counter omega-3 supplements is clinically significant. The FDA approval was based on hard endpoints: myocardial infarction, stroke, cardiovascular death. Non-prescription fish oil lacks the dose, purity, and pharmacokinetic profile to achieve therapeutic efficacy. Misinformation on this point is pervasive and dangerous.
John Samuel - 19 December 2025
Let’s be real - triglycerides are the silent ninja of cardiovascular doom 🥷💥. You’re out here eating "healthy" granola bars loaded with agave syrup, sipping oat milk lattes with three pumps of caramel, and wondering why your blood looks like oil paint. Meanwhile, your pancreas is throwing a silent rave with free fatty acids and chylomicrons. Prescription EPA isn’t a luxury - it’s your body’s emergency brake. Stop gambling with your organs.
Sai Nguyen - 20 December 2025
Americans eat too much sugar and call it diet. In India we know real food - rice, lentils, vegetables. No soda, no cake. If you get sick, it’s your fault for eating garbage. Stop blaming doctors. Fix your plate.
Michelle M - 21 December 2025
It’s funny how medicine treats symptoms like puzzles to solve, but never asks why the body is screaming in the first place. High triglycerides aren’t just a lab number - they’re a message. Your body’s saying: I’m drowning in energy I can’t use. You’re not broken. You’re overloaded. The real cure isn’t a pill - it’s learning to live slower, eat cleaner, and stop treating food like entertainment. That’s the hard part.
Lisa Davies - 21 December 2025
I’m so glad someone finally broke this down without jargon 💪❤️ I was terrified after my numbers hit 800 - felt like I was walking around with a ticking bomb. Started walking with my mom every morning, swapped soda for sparkling water with lemon, and took my EPA prescription like clockwork. 12 weeks later? 210. I cried. Not because I lost weight - because I finally felt like I was taking back my health. You got this. One step at a time 🌱
Nupur Vimal - 22 December 2025
Everyone talks about sugar but no one mentions insulin resistance. That’s the real root. If you’re insulin resistant, even healthy fats will spike triglycerides. You need metformin not just diet. I’ve seen 50 people with high triglycerides - all had prediabetes. Doctors miss this every time. Just saying