When your child is sick and needs antibiotics, getting the dose right is only half the battle. The other half? Storing it properly. Many parents don’t realize that how they keep their child’s liquid antibiotic can make the difference between a quick recovery and a treatment that fails - or worse, leads to antibiotic resistance.
Antibiotic suspensions are liquid forms of medicine designed for kids who can’t swallow pills. They come as powder you mix with water, and once mixed, they don’t last forever. If stored wrong, they lose strength. That means your child might not get the full dose they need, and the infection could come back - stronger.
Why Storage Matters More Than You Think
Improper storage is a silent problem. A 2022 CDC study found that 15% of pediatric antibiotic treatment failures were linked to wrong storage. That’s not just a small number - it’s one in every seven kids who don’t get better because the medicine wasn’t kept right.
Think about it: if you leave a bottle of amoxicillin in a hot bathroom or keep it in the fridge when it shouldn’t be there, you’re not just messing up the taste. You’re changing how well the medicine works. Some antibiotics break down fast at room temperature. Others get too thick to swallow if chilled. And if you keep it past its discard date? You’re giving your child a weak or even useless dose.
Amoxicillin: The Most Common, But Not Simple
Amoxicillin is the #1 antibiotic prescribed for kids. It’s used for ear infections, strep throat, and pneumonia. But here’s the twist: you can store it two different ways - and both are okay.
- Refrigerated (2-8°C / 36-46°F): Keeps it stable and improves taste. Many kids prefer it cold.
- Room temperature (20-25°C / 68-77°F): Also safe. The medicine stays effective for the full 14 days.
It doesn’t matter which you pick - as long as you stick to it. Don’t switch back and forth. Moving it between fridge and counter can cause changes in how the medicine stays mixed. And remember: no matter where you store it, throw it out after 14 days. Even if it looks fine.
Some pharmacies put a sticker on the bottle that says “Refrigerate.” Others say “Store at room temperature.” If there’s a conflict, trust the pharmacy label - not what you heard from a friend or online forum.
Amoxicillin/Clavulanate (Augmentin): Must Stay Cold
This one’s different. Augmentin combines amoxicillin with clavulanate to fight tougher bacteria. But clavulanate is fragile. It breaks down fast if left at room temperature.
- Always refrigerate - between 2°C and 8°C.
- Discard after 10 days - even if it looks clear and smells fine.
Research shows that after day 10, the clavulanate loses over 12% of its strength. That means the medicine can’t fight the bacteria it’s supposed to. In fact, studies show it starts losing effectiveness as early as day 5 if kept at 27°C or higher - which is common in many homes during summer.
Don’t be fooled by the smell or color. If it’s been out too long, it won’t look spoiled. That’s why the discard date is non-negotiable.
Azithromycin (Zithromax): Keep It at Room Temperature
Azithromycin is another common choice, especially for kids who can’t take penicillin. But here’s the catch: do not refrigerate it.
When chilled, azithromycin thickens up. It becomes sticky, hard to pour, and tough for kids to swallow. A 2023 taste study found that 37% of children refused to take it when cold. That’s why the manufacturer recommends storing it at room temperature - between 20°C and 25°C.
It’s stable for 10 days at room temp. After that, potency drops. Discard it on day 11, no exceptions.
Other Antibiotics That Shouldn’t Be Refrigerated
Not all liquid antibiotics are the same. Here’s a quick list of ones that should stay at room temperature:
- Azithromycin (Zithromax)
- Clarithromycin
- Clindamycin
- Sulfamethoxazole/Trimethoprim (Bactrim)
- Cefdinir
If you’re unsure, check the label. If it says “Do not refrigerate,” don’t. Even if your other meds are in the fridge.
How to Tell If It’s Gone Bad
Medicine doesn’t always look spoiled. But here are signs to watch for:
- Discoloration - turning yellow, brown, or cloudy when it was clear before.
- Strange taste - if it tastes sour, metallic, or bitter, even if it didn’t before.
- Too thick or too watery - if it’s clumpy or separates into layers that won’t mix back.
- Odd smell - if it smells like vinegar or rotten eggs.
If you see any of these, throw it out. Don’t guess. Don’t try to shake it back together. Just discard it.
Best Practices for Storage
Here’s what actually works in real homes:
- Check the label - Every bottle has a storage instruction. If it says “Refrigerate,” do it. If it says “Store at room temperature,” leave it out.
- Use a discard date sticker - Many pharmacies give you one. If they don’t, write the date on the bottle with a permanent marker. Write “Discard: [Date]” in big letters.
- Keep it out of reach - Store all medicines up and away - not on counters, in nightstands, or in bathroom cabinets. The American Association of Poison Control Centers reports over 60,000 accidental poisonings in kids under 5 each year.
- Don’t store near heat - Avoid windowsills, ovens, or radiators. Room temperature means 20-25°C. Many homes hit 27°C or higher in summer.
- Use a mini-fridge if needed - If you have multiple refrigerated meds, a small, dedicated fridge (like a mini-bar) helps avoid temperature swings from opening the main fridge.
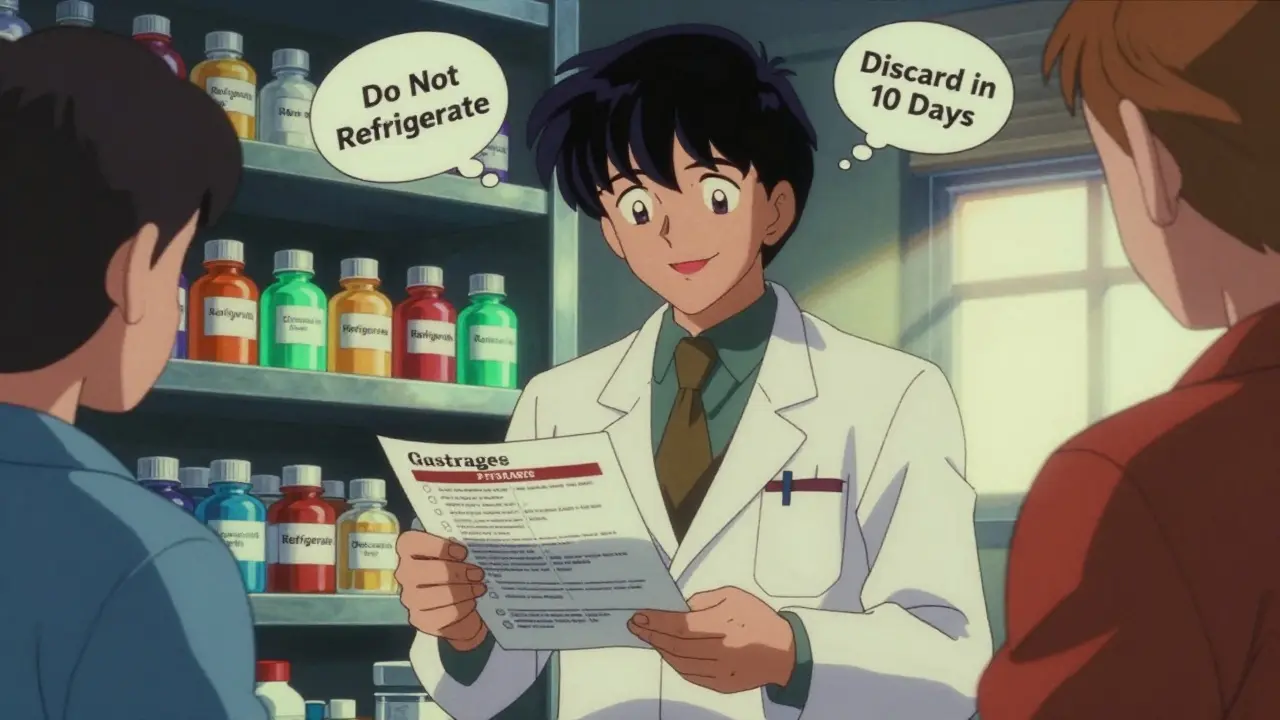
What to Do If You’re Confused
Parents often get mixed messages. One pharmacist says refrigerate. The label says room temp. Your friend says her kid’s medicine was fine after 16 days.
Here’s the rule: When in doubt, call the pharmacy. Pharmacists are trained to know the exact storage rules for each brand and batch. They can check the manufacturer’s data and tell you exactly what to do.
Also, ask for a written instruction sheet. Most pharmacies will print one if you ask. It’s not extra work - it’s part of their job.
What Happens If You Use Expired Medicine?
Using medicine past its discard date doesn’t make your child sick. But it doesn’t work right.
The antibiotic might be too weak to kill the bacteria. The infection lingers. Then you go back to the doctor. They prescribe another round. Maybe a stronger one. Maybe even an IV. All because the first one didn’t work - not because the infection was tough, but because the medicine had gone bad.
And here’s the bigger risk: when antibiotics don’t fully kill bacteria, the survivors learn to fight back. That’s how antibiotic resistance starts. It’s not just your child’s problem - it’s everyone’s.
Tools That Help
Some parents use apps to track discard dates. The CDC’s MedSafe app sends phone reminders when your child’s medicine is due to be thrown out. It’s free, simple, and works offline.
Another trick: set a calendar alert the day you mix the medicine. Mark it for 10 or 14 days later - whichever applies. Put a sticky note on the fridge. Tape the discard date to the bottle. Whatever works for you.
Final Reminder: Don’t Guess. Don’t Risk It.
Antibiotics are powerful. They save lives. But they’re not like juice or syrup. They’re medicine - and medicine has rules.
Follow the label. Use the discard date. Store it right. And if you’re ever unsure? Ask your pharmacist. It’s why they’re there.
Your child’s health depends on it - not on guesswork, not on old advice, not on what worked last time. It depends on the medicine being strong, clean, and ready to work. And that starts with how you store it.