By 2026, nearly 40% of all chronic disease management plans will include digital therapeutics alongside traditional medications. This isn’t science fiction-it’s happening right now. Patients with diabetes, anxiety, asthma, and opioid use disorder are using apps that don’t just remind them to take their pills-they adjust treatment in real time, track behavior, and even communicate directly with their doctors. But here’s the problem: what happens when these apps interact with your pills? Could an app make your blood thinner less effective? Could it worsen side effects from your antidepressant? These aren’t theoretical concerns. They’re real, documented risks that clinicians and patients are only beginning to understand.
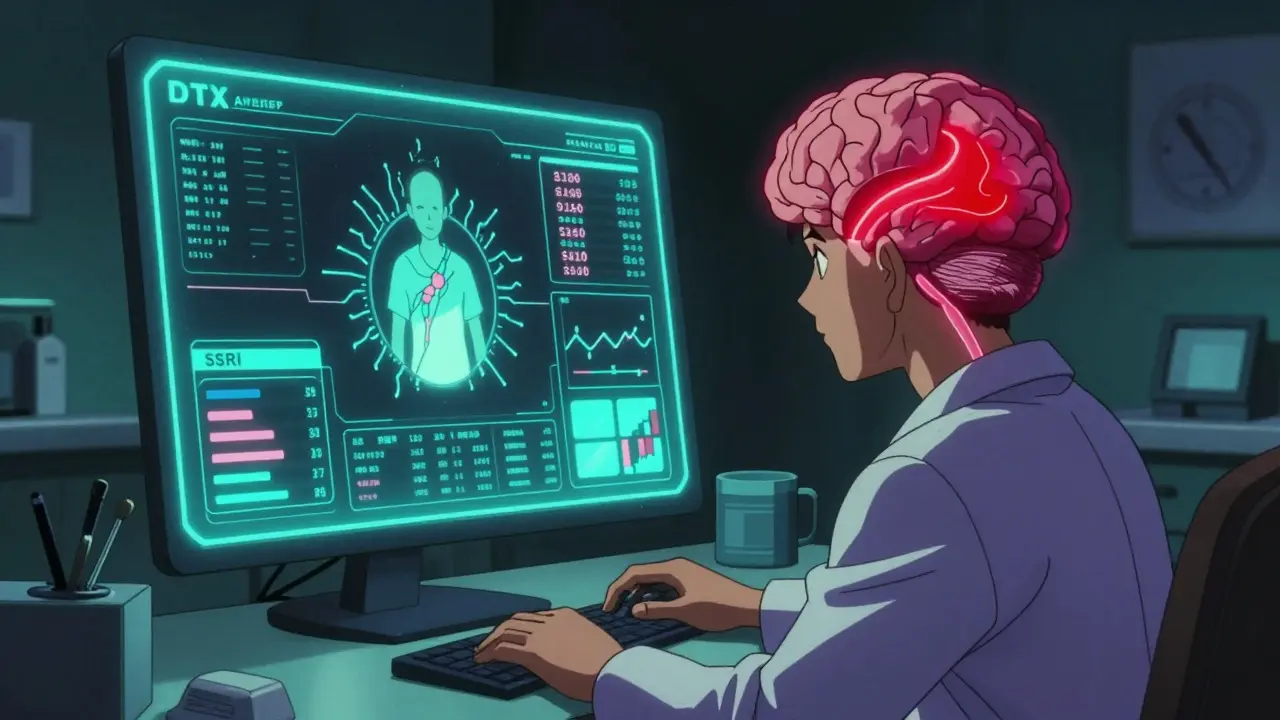
What Exactly Are Digital Therapeutics?
Digital therapeutics (DTx) are software-based treatments approved by regulators like the FDA to treat, manage, or prevent medical conditions. Unlike fitness apps or meditation tools, DTx are medical interventions. They’re prescribed. They’re covered by insurance. And they’re backed by clinical trials.
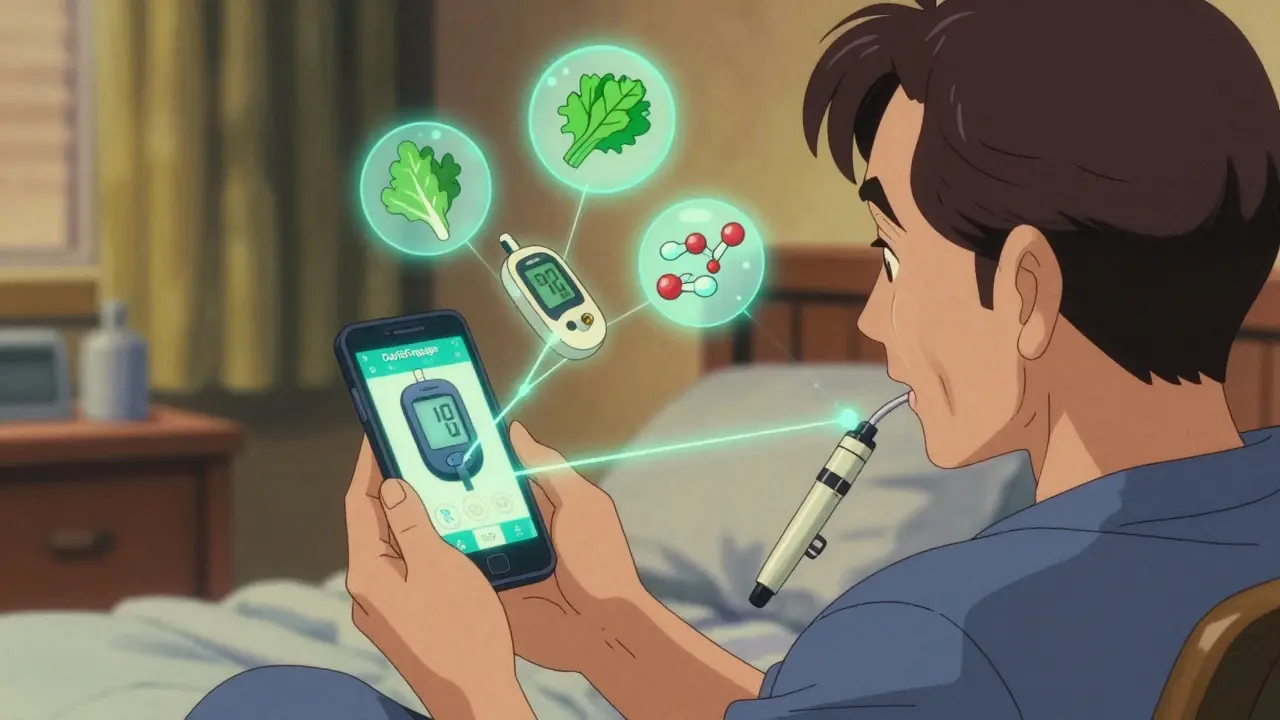
Take DaylightRx, cleared by the FDA in September 2024. It’s not a mindfulness app. It’s a 90-day, clinically validated cognitive behavioral therapy (CBT) program for generalized anxiety disorder. It’s designed to replace or reduce the need for benzodiazepines or SSRIs in some patients. Then there’s DarioEngage, used by over 2.3 million people globally to manage diabetes. It doesn’t just log blood sugar-it gives real-time insulin dose suggestions based on food intake, activity, and glucose trends.
These aren’t passive tools. They’re active treatments. And like any drug, they can interact with other treatments-even if they don’t contain chemicals.
How DTx Interact With Medications: The Hidden Risks
Most people assume digital therapeutics are harmless because they’re not pills. But that’s a dangerous assumption.
Consider this: a patient on warfarin (a blood thinner) uses a DTx app that tracks their diet and activity. The app notices they’ve started eating more leafy greens-a known source of vitamin K, which counteracts warfarin. The app adjusts its recommendations and alerts their doctor. That’s a win.
But what if the same app uses AI to personalize CBT modules for depression, and the patient is also taking an SSRI? The app might push intense exposure exercises during a period when the medication hasn’t yet stabilized their mood. Result? Increased anxiety, insomnia, or even emotional breakdowns. In clinical trials for EndeavorRx (an ADHD treatment), 7% of users reported headaches, dizziness, or emotional distress-side effects that could easily be mistaken for medication reactions.
There’s also the issue of adherence. DTx apps like Medisafe have been shown to boost medication adherence by up to 25% in chronic conditions. That sounds great-until you realize: if the app fails to remind someone to take their antiretroviral, they risk developing drug resistance. If it over-reminds, they might start skipping doses out of frustration. The app isn’t just a tool-it’s part of the treatment equation.
Real-World Examples: When DTx Helps-and When It Hurts
On Reddit’s r/diabetes, users report dramatic improvements. One patient wrote: “DarioEngage helped me drop my HbA1c from 9.8 to 7.6 in six months. My endocrinologist adjusted my insulin based on the app’s data. I haven’t had a low since.” That’s DTx working as intended: enhancing medication effectiveness through data.
But on r/mentalhealth, the story is different. A user shared: “DaylightRx felt robotic. It didn’t account for the nausea I got from my SSRIs. I stopped using it after two weeks.” That’s a failure of personalization. The app delivered a generic CBT protocol without adjusting for medication side effects.
Another case: a 72-year-old patient with COPD was prescribed a DTx app that connects to a smart inhaler. The app tracks usage and sends alerts to their pulmonologist. But the patient couldn’t figure out how to sync the device. Within 30 days, they stopped using it. Their inhaler use dropped back to pre-app levels. Their ER visits increased. Without in-person onboarding, the DTx didn’t just fail-it created a gap in care.
Who’s Responsible When Something Goes Wrong?
Who do you call if a DTx app causes a bad reaction? The doctor? The app developer? The pharmacy?
Right now, it’s a gray zone. The FDA regulates DTx as medical devices, but the rules are still evolving. Prescription DTx need 510(k) clearance or De Novo classification. But there’s no standardized way to report adverse events tied to software interactions. Unlike a drug, where the manufacturer must report side effects, DTx developers often don’t have clear pathways to report “software-related” harm.
And it’s not just safety-it’s liability. If a DTx app recommends a dose adjustment that leads to a hospitalization, who’s at fault? The algorithm? The clinician who approved the app? The patient who didn’t understand the warning?
Regulators are scrambling to catch up. The FDA plans to release new guidance on DTx clinical evidence in Q2 2025-specifically focused on how these tools interact with medications. Until then, the burden falls on clinicians to understand what’s in the apps they’re prescribing.
Why DTx Works Best With Certain Medications
Not all medications benefit equally from digital support. DTx shines where behavior is the biggest barrier to success.
- Anticoagulants (warfarin): DTx helps track diet, alcohol, and other drugs that affect blood thinning. Real-time alerts reduce dangerous INR fluctuations.
- Insulin: Apps like DarioEngage correlate glucose readings with meals, activity, and insulin doses-leading to better titration and fewer lows.
- Antiretrovirals: Studies show DTx adjuncts increase adherence by 16% in HIV patients, reducing viral rebound risk.
- Psychiatric meds: DTx can monitor mood, sleep, and medication side effects, helping doctors adjust doses faster. But only if the app is tailored to the patient’s specific drug profile.
On the flip side, DTx struggles with acute conditions (like infections or heart attacks) or patients with low digital literacy. A 2024 JMCP study found 45% of patients over 65 stopped using DTx within a month without in-person support. That’s not a tech problem-it’s a care design problem.
What Clinicians and Patients Need to Do Now
If you’re a patient prescribed a DTx:
- Ask: “Is this FDA-cleared as a medical device?” Not all health apps are DTx. Only those with regulatory clearance are proven to treat conditions.
- Ask: “How does this interact with my current meds?” Don’t assume it’s safe just because it’s digital.
- Ask: “Will someone help me set this up?” If you’re over 65 or not tech-savvy, demand onboarding support.
If you’re a clinician:
- Review the DTx’s clinical trial data-especially studies that tested it alongside medications.
- Don’t just hand out an app link. Schedule a 15-minute onboarding session.
- Integrate DTx data into your EHR. If the app can’t talk to your system, you’re missing critical insights.
- Track discontinuation rates. If more than 20% of patients stop using it in 30 days, the app isn’t right for your population.
Health systems that assign “DTx navigators”-staff trained to help patients troubleshoot apps-see a 33% drop in discontinuation rates. That’s not a luxury. It’s a necessity.
The Future: DTx as Part of the Medication Ecosystem
By 2027, 65% of specialty pharmacy prescriptions will require a digital companion to qualify for insurance coverage. That means DTx won’t be optional-it’ll be standard.
The next frontier? DTx that adjust medication doses automatically. Imagine an app that detects a patient’s rising anxiety from voice patterns and sleep data, then alerts their psychiatrist to reduce their SSRI dose before side effects worsen. Or an insulin app that uses real-time glucose and activity data to suggest a 10% dose reduction before a workout.
This isn’t far off. The technology exists. The data is there. What’s missing is the framework to make it safe.
Right now, we’re treating digital therapeutics like apps. We need to start treating them like drugs. Because in practice-they are.
Are digital therapeutics the same as health apps?
No. Health apps like meditation or step trackers are wellness tools. Digital therapeutics (DTx) are FDA-cleared medical devices designed to treat, manage, or prevent specific diseases. They require clinical evidence, are prescribed by doctors, and are often covered by insurance. Examples include DaylightRx for anxiety and DarioEngage for diabetes. If it’s not cleared by the FDA as a medical device, it’s not a DTx.
Can digital therapeutics replace medications?
Sometimes. Some DTx, like DaylightRx for generalized anxiety, are approved as standalone treatments. Others, like DarioEngage for diabetes, are designed to enhance medication effectiveness-not replace it. The goal isn’t always to eliminate pills, but to make them work better. Always consult your doctor before stopping or changing any medication, even if a DTx app suggests it.
Do digital therapeutics have side effects?
Yes. While they don’t cause chemical side effects like nausea or drowsiness, DTx can cause emotional, cognitive, or physical stress. Clinical trials for EndeavorRx showed 7% of users experienced headaches, dizziness, frustration, or emotional reactions. Poorly designed apps can increase anxiety, cause burnout from constant reminders, or lead to disengagement. These aren’t minor issues-they’re treatment-related adverse events that need to be monitored.
How do I know if a DTx is safe to use with my meds?
Ask for the clinical study data. Specifically, look for trials that tested the DTx alongside your current medications. Ask your doctor or pharmacist: “Has this app been studied with [your medication name]?” If the manufacturer can’t provide this, proceed with caution. Also check if the app integrates with your pharmacy or EHR-this helps your care team spot potential conflicts.
Why do some patients stop using digital therapeutics?
Four main reasons: 1) No onboarding-patients are given an app link and left to figure it out. 2) Poor integration with their pharmacy or EHR, leading to refill issues. 3) The app doesn’t adapt to their medication side effects. 4) They’re over 65 and struggle with tech. Studies show patients over 70 are 38% more likely to quit within 30 days without hands-on support. DTx works best when paired with human guidance.



Matthew Miller - 11 January 2026
This is why we can't have nice things. Apps that 'adjust treatment in real time' are just glorified guesswork with a FDA stamp. You think a 90-day CBT algorithm knows more about your serotonin levels than your psychiatrist? Please. The moment you let software manage your meds, you're one buggy update away from a hospital bed.
Vincent Clarizio - 12 January 2026
Let me tell you something profound-this isn't about apps or algorithms. It's about the erosion of human agency in medicine. We've outsourced our bodies to code, and now we're surprised when the code doesn't understand grief, or fatigue, or the quiet despair of a 72-year-old staring at a smartphone they can't figure out. The real crisis isn't drug interactions-it's the delusion that technology can heal what we've stopped being willing to feel. We're not treating diseases anymore. We're optimizing patients like faulty IoT devices. And the worst part? We're proud of it.
Priya Patel - 13 January 2026
As someone from India where digital literacy is still growing, I’ve seen both sides-people who thrive with these apps and others who feel abandoned by them. The key isn’t the tech-it’s the support. A simple 15-minute call from a nurse or community health worker can make all the difference. We need more human touch, not more code.
Jason Shriner - 15 January 2026
so like... the app is gonna tell me to stop taking my antidepressant because i cried during a netflix show? cool. ill just delete it and go back to my therapist who actually remembers my name. also why does everything have to be a fucking app now? i miss the days when doctors just talked to you.
Jennifer Littler - 17 January 2026
From a clinical informatics perspective, the real bottleneck isn't the DTx itself-it's the lack of interoperability with EHRs. If the app's data can't auto-populate into the EMR, clinicians are forced to manually cross-reference data, which defeats the purpose. We need FHIR-based integration standards, not just marketing buzzwords. Also, the 7% adverse event rate in EndeavorRx? That's clinically significant. We're not talking about 'user frustration'-we're talking about treatment-emergent adverse events that require pharmacovigilance protocols.
Priscilla Kraft - 18 January 2026
I love how this post highlights both the potential and the pitfalls. I've seen patients who went from HbA1c 10.2 to 6.8 with DarioEngage-life-changing. But I've also seen elderly patients get overwhelmed and stop using them. The solution? Pair DTx with a digital navigator. Not a tech support line-someone who sits with them, helps them sync, and checks in weekly. Tech is a tool. Humans are the cure.
Alfred Schmidt - 18 January 2026
THEY’RE NOT APPS. THEY’RE MEDICATIONS. I SAID IT. THEY’RE MEDICATIONS. IF YOU’RE PRESCRIBING A DTX, YOU’RE PRESCRIBING A DRUG. YOU NEED TO DOCUMENT INTERACTIONS. YOU NEED TO MONITOR SIDE EFFECTS. YOU NEED TO REPORT ADVERSE EVENTS. AND IF YOU’RE NOT DOING THAT, YOU’RE COMMITTING MEDICAL NEGLIGENCE. STOP TREATING DIGITAL THERAPEUTICS LIKE A SPOTIFY PLAYLIST.
Sean Feng - 19 January 2026
40% of chronic care plans using DTx by 2026? Cool. I'll believe it when I see a single study showing it reduces hospitalizations. Until then, it's just another Silicon Valley fantasy wrapped in clinical jargon. People don't need more apps. They need more time with their doctors.
Alex Smith - 21 January 2026
What's funny is that the same people pushing DTx as the future of care are the ones who never bother to ask if patients can actually use them. I've watched grandmas try to sync inhalers while their grandkids are on Zoom. The tech works-if you're 25 and tech-savvy. For everyone else? It's a barrier. We need universal design, not just FDA clearance. And maybe-just maybe-stop assuming everyone wants to be managed by an algorithm.
Sam Davies - 21 January 2026
Oh, so now we’re treating software as if it’s a physician? How quaint. I suppose next we’ll have AI write our wills and algorithmically decide who gets a liver transplant. The arrogance of assuming a 90-day CBT module can outperform a trained therapist is almost as alarming as the fact that insurance companies are mandating this nonsense. The future is here-it’s just not evenly distributed. And it’s definitely not safer.
Roshan Joy - 22 January 2026
As someone who works with rural diabetic patients in India, I’ve seen DTx apps change lives-but only when paired with local health workers. One lady, 68, couldn’t use DarioEngage until her granddaughter sat with her every morning for a week. Now her HbA1c is 7.1. The tech? Just a tool. The real magic? Someone who cared enough to show up. We need more of that, not less.
Madhav Malhotra - 23 January 2026
From India, I’ve seen how tech can bridge gaps-like a rural mom using a DTx app to track her child’s asthma triggers and sharing data with her city-based doctor over WhatsApp. But the key is simplicity. No jargon. No complex menus. Just clear, calm prompts. And always, always a human on the other end. Tech should serve, not replace, compassion.
Priscilla Kraft - 25 January 2026
Just read someone say DTx is 'just an app.' That’s like saying insulin is 'just a liquid.' It’s not about the form-it’s about the function. If it’s FDA-cleared as a medical device, prescribed by a doctor, and alters clinical outcomes? It’s a treatment. And treatments need monitoring, just like pills. We need adverse event reporting systems for DTx. And we need them yesterday. 🙏