When researchers talk about Alzheimer's disease is a progressive neurodegenerative disorder that impairs memory, thinking, and behavior, they usually focus on the brain. But the eyes can reveal early signs, and a growing body of research links Alzheimer's disease to various forms of vision loss.
Vision loss refers to a reduction in the ability to see clearly, ranging from mild blurriness to complete blindness, can be caused by cataracts, glaucoma, age‑related macular degeneration (AMD), or damage to the optic nerve. When dementia enters the picture, the pattern of eye problems often looks different, and spotting those differences can be a clue that cognitive decline is starting.
Alzheimer’s Disease in a Nutshell
Alzheimer’s disease affects roughly 55 million people worldwide, and the number is climbing as populations age. The disease is marked by two hallmarks: beta‑amyloid plaques are sticky protein clumps that accumulate between nerve cells, and tau tangles are twisted fibers that build up inside neurons. Together they disrupt communication, starve brain cells of nutrients, and eventually cause cell death.
Typical symptoms begin with short‑term memory lapses, then progress to language problems, disorientation, and loss of executive function. Diagnosis usually relies on cognitive testing, brain imaging, and sometimes analysis of cerebrospinal fluid.
How Vision Loss Shows Up in Alzheimer’s
People with Alzheimer’s often report blurry vision, difficulty recognizing faces, and trouble reading. These issues are not always due to age‑related eye disease; they can stem from the same pathological processes that damage the brain.
- Retinal thinning: Optical coherence tomography (OCT) studies have shown that the retinal nerve‑fiber layer becomes thinner in Alzheimer’s patients, mirroring cortical thinning.
- Reduced contrast sensitivity: Even when visual acuity is normal, patients struggle to differentiate shades, hinting at dysfunction in the visual processing pathways.
- Visual hallucinations: Up to 25 % of individuals with moderate‑to‑severe Alzheimer’s experience vivid, often unsettling, images that are not present.
These symptoms can be mistaken for ordinary aging, but research published in 2023 found that retinal changes can appear up to 10 years before memory problems become obvious.
Biological Bridges: Why the Eyes and Brain Talk
The eye is an extension of the central nervous system; the retina shares embryonic origins with the brain. This common lineage means that neurodegenerative processes can affect both structures.
Key mechanisms linking Alzheimer’s to vision loss include:
- Beta‑amyloid deposition in the retina: Post‑mortem studies discovered amyloid plaques in the retinal pigment epithelium, suggesting that the same toxic protein aggregates form outside the brain.
- Tau pathology in optic nerve fibers: Animal models reveal that tau tangles travel along the optic tract, compromising signal transmission from eye to brain.
- Microvascular damage: Small blood‑vessel disease reduces oxygen delivery to both the brain and the retina, leading to ischemic injury.
- Inflammatory cascades: Chronic inflammation driven by activated glial cells can spill over into ocular tissues, worsening cataract formation and dry‑eye symptoms.
These pathways create a feedback loop: as brain cells die, visual processing deteriorates, which in turn can accelerate cognitive decline because the brain receives less accurate sensory input.
What the Latest Studies Say
Several high‑profile studies have shaped our understanding in the past few years:
| Study | Population | Primary Eye Measure | Result |
|---|---|---|---|
| Smith et al., 2021 | 120 adults 60‑80 y | Retinal nerve‑fiber layer thickness (OCT) | Average 12 µm thinner in early Alzheimer’s vs controls |
| Lee & Patel, 2022 | 85 diagnosed patients | Beta‑amyloid PET imaging of retina | Positive retinal amyloid signal correlated with lower Mini‑Mental State Exam scores |
| Gonzalez et al., 2023 | 200 community‑dwelling seniors | Contrast sensitivity test | Reduced contrast sensitivity predicted conversion to dementia within 3 years |
| Kumar et al., 2024 | 60 patients with mild cognitive impairment | Visual hallucination questionnaire | 30 % reported hallucinations; all had elevated tau levels in cerebrospinal fluid |
These findings reinforce that eye exams can serve as a low‑cost screening tool for early Alzheimer’s, especially in primary‑care settings.
Practical Steps for Patients and Caregivers
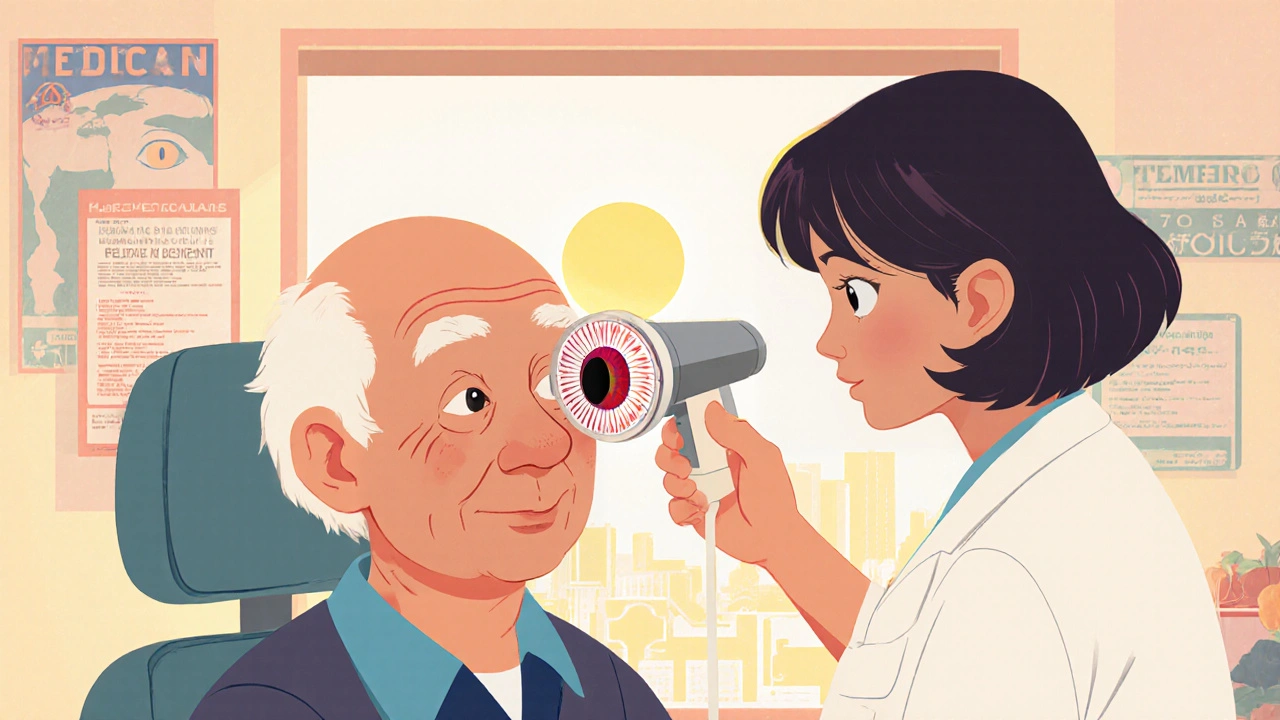
If you or a loved one is dealing with memory issues, consider the following eye‑health actions:
- Schedule regular comprehensive eye exams: At least once a year after age 60, or more often if you have known risk factors.
- Ask about retinal imaging: OCT and, where available, retinal amyloid scans can add valuable information.
- Monitor visual symptoms: Sudden changes in glare, depth perception, or the appearance of visual hallucinations should be reported promptly.
- Control vascular risk factors: Manage blood pressure, cholesterol, and diabetes to protect both brain and eye vessels.
- Stay active mentally and physically: Exercise, puzzles, and social engagement have been shown to slow both cognitive and visual deterioration.
Implications for Early Detection
Traditional Alzheimer’s screening relies on neuropsychological tests, which may miss subtle early changes. Eye‑based biomarkers offer a complementary approach:
- Non‑invasive and quick: An OCT scan takes less than five minutes and does not require contrast agents.
- Potential for mass screening: Vision clinics already see millions of older adults annually, providing an existing infrastructure.
- Cost‑effective: Compared with brain MRI or PET scans, retinal imaging is far cheaper.
Researchers are now developing AI algorithms that analyze retinal photographs to predict Alzheimer’s risk with up to 85 % accuracy. If these tools become mainstream, a simple eye check could become a routine part of dementia prevention programs.
Future Directions and Ongoing Trials
Several clinical trials are exploring whether treating retinal amyloid deposits can slow brain disease:
- Anti‑amyloid eye drops: A Phase II trial in 2024 tested a topical formulation that clears retinal plaques; early data show modest improvement in contrast sensitivity.
- Neuroprotective supplements: Omega‑3 fatty acids and lutein are being evaluated for their ability to preserve retinal nerve‑fiber thickness.
- Gene‑editing approaches: Researchers are investigating CRISPR‑based strategies to reduce tau expression in ocular tissues, hoping to protect optic nerve health.
While many of these studies are still in early stages, they illustrate a growing belief that the eye is not just a passive observer but a potential therapeutic target.
Take‑Home Messages
- Alzheimer’s disease and vision loss share common pathways, including beta‑amyloid buildup, tau pathology, and microvascular damage.
- Retinal thinning, reduced contrast sensitivity, and visual hallucinations can appear years before memory loss becomes obvious.
- Regular eye exams, especially OCT imaging, can help flag early neurodegeneration.
- Lifestyle choices that protect vascular health benefit both brain and eyes.
- Emerging AI and drug research may soon turn routine eye checks into powerful dementia‑screening tools.
Frequently Asked Questions
Can vision loss cause Alzheimer’s disease?
No. Vision loss itself does not cause Alzheimer’s, but shared risk factors and similar pathological processes mean that eye problems can be a warning sign of brain changes.
What eye test is most useful for spotting Alzheimer’s?
Optical coherence tomography (OCT) is currently the most promising because it measures retinal nerve‑fiber layer thickness, which tends to thin in early Alzheimer’s.
Are cataracts related to Alzheimer’s?
Cataracts are caused by lens protein clumping and are not directly linked to Alzheimer’s, though both conditions become more common with age.
How often should someone with mild cognitive impairment get eye exams?
At least once a year, and more frequently if any new visual symptoms appear.
Can treating eye disease improve memory?
Treating eye conditions can improve quality of life and reduce visual strain, but it does not reverse existing brain pathology. However, better vision may help maintain mental engagement.


WILLIS jotrin - 22 October 2025
It's fascinating how the retina can act like a window into the brain's health.
The article does a solid job summarizing the shared pathways between Alzheimer's and vision loss.
I think the most compelling point is that retinal thinning shows up years before any memory complaints.
That gives clinicians a real chance for early intervention, especially if we integrate OCT scans into routine check‑ups.
Of course, lifestyle factors still matter; protecting vascular health benefits both eyes and mind.
Kiara Gerardino - 31 October 2025
The reckless neglect of ocular biomarkers is an ethical catastrophe that betrays our most vulnerable elders.
Sameer Khan - 8 November 2025
Recent advances in ocular imaging have elucidated a robust mechanistic convergence between neurodegenerative pathology and retinal physiology.
Beta‑amyloid deposition, historically characterized within cerebral parenchyma, has now been consistently identified in the retinal pigment epithelium via post‑mortem immunohistochemistry.
Concurrently, hyperphosphorylated tau aggregates have been observed traversing optic nerve axons, implicating axonal transport disruption as a shared etiological vector.
Microvascular compromise, as evidenced by reduced retinal capillary density on fluorescein angiography, mirrors cerebral small‑vessel disease, thereby accentuating a systemic vascular component.
These observations are corroborated by optical coherence tomography studies demonstrating a statistically significant reduction in retinal nerve‑fiber layer thickness, averaging 12 µm in early‑stage Alzheimer's cohorts compared with age‑matched controls.
Moreover, functional assessments such as contrast sensitivity testing have yielded prognostic value, with diminished thresholds predicting conversion to dementia within a three‑year horizon.
From a biomarker standpoint, the non‑invasive nature of OCT and the potential for AI‑driven retinal image analysis present a scalable screening paradigm.
Algorithmic models trained on large retinal datasets have achieved up to 85 % accuracy in discriminating preclinical Alzheimer's pathology.
Importantly, these retinal signatures appear up to a decade prior to overt cognitive deficits, suggesting a window for preemptive therapeutic strategies.
Interventional trials employing anti‑amyloid eye drops are currently exploring whether local clearance can attenuate downstream neurodegeneration.
Parallel investigations into neuroprotective nutraceuticals, such as lutein and omega‑3 fatty acids, aim to preserve retinal ganglion cell integrity, which may indirectly support cortical visual processing.
Gene‑editing approaches targeting tau expression in ocular tissue are in nascent stages but hold theoretical promise for mitigating axonal degeneration.
Clinically, integrating regular ophthalmologic evaluation into geriatric care pathways could facilitate early detection, especially when combined with vascular risk factor optimization.
Nevertheless, methodological heterogeneity across studies necessitates standardized protocols for retinal imaging and data interpretation.
In sum, the convergence of molecular pathology, vascular health, and advanced imaging underscores the retina's potential as a sentinel organ for neurodegeneration.
Michael Vandiver - 17 November 2025
Wow Sameer this is mind‑blowing 🤯 OCT scans could be a game‑changer for us regular folks 🙌 let’s push for more eye‑doc visits!
Suryadevan Vasu - 25 November 2025
The correlation between retinal microvasculature and cerebral perfusion is well‑documented; clinicians should therefore consider OCT as an adjunctive diagnostic tool.
Tiffany Davis - 4 December 2025
I appreciate the practical checklist; scheduling annual eye exams and monitoring visual changes are simple steps that can make a big difference.
Don Goodman-Wilson - 12 December 2025
Sure, because waiting for a fancy eye‑drop to fix brain decay is exactly what the healthcare system needs right now.
Bret Toadabush - 20 December 2025
They don’t want us to know that the big pharma labs are hiding the real cure-just push their expensive eye scans to keep the money flowing.
Diane Thurman - 29 December 2025
Eye exams are great but dont forget the brain tests too.
Iris Joy - 6 January 2026
Don, while the sarcasm is noted, there are genuine studies showing modest benefits from ocular treatments, and staying proactive with regular check‑ups can still provide valuable information for overall health.
Sarah Riley - 15 January 2026
The retinal‑cerebral axis exemplifies a neurovascular coupling paradigm amenable to quantitative imaging biomarkers.
Tammy Sinz - 23 January 2026
Given the evidence, shouldn't we advocate for integrating retinal OCT into standard dementia screening protocols, especially in primary care settings where early detection is paramount?
Christa Wilson - 1 February 2026
Absolutely Tammy! 🌟 Early detection saves lives and smiles – let’s spread the word and make eye health a community priority! 😊