When a generic drug hits the shelf, you might assume it’s just a cheaper copy of the brand-name version. But behind that simple label is a complex science designed to prove it works the same way in your body. That’s where bioequivalence testing comes in. It’s not just a formality-it’s the gatekeeper ensuring that generics are safe, effective, and interchangeable. And there are two main ways to prove it: in vivo and in vitro. Knowing when each is used helps explain why some generics are approved quickly and cheaply, while others face years of testing and millions in costs.
What Is Bioequivalence, Really?
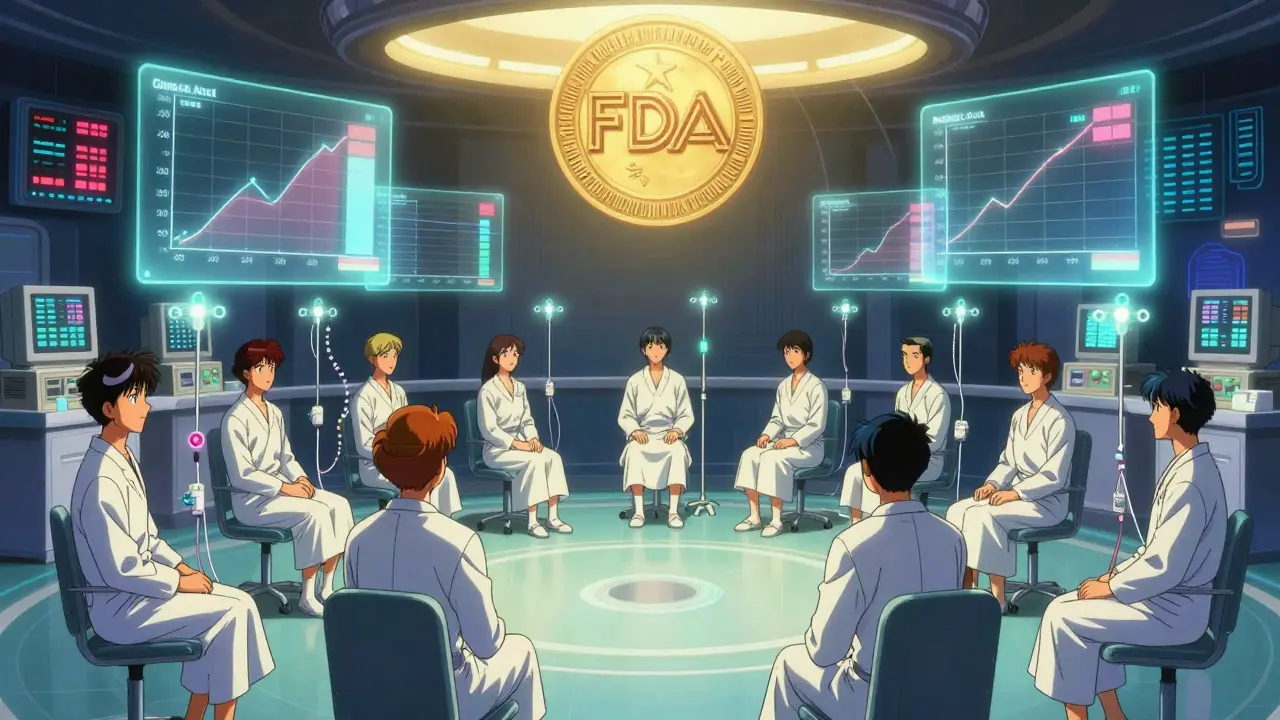
Bioequivalence means two drug products-say, a brand-name pill and its generic version-deliver the same amount of active ingredient into your bloodstream at the same rate. It’s not about looking the same or tasting the same. It’s about whether your body absorbs and uses the drug the same way. The U.S. Food and Drug Administration (FDA) requires this proof before allowing a generic drug to be sold. Without it, you could get a version that’s too weak to work, or too strong and causes side effects.
The standard measure? Two key numbers: Cmax (the highest concentration of the drug in your blood) and AUC (how much of the drug your body is exposed to over time). For a generic to be approved, the 90% confidence interval for the ratio of these values between the generic and brand-name version must fall between 80% and 125%. That’s a tight window. For drugs with a narrow therapeutic index-like warfarin or levothyroxine-it’s even tighter: 90% to 111.11%. One percentage point outside that range, and the drug gets rejected.
In Vivo Testing: The Gold Standard
In vivo bioequivalence testing means testing in a living organism-usually healthy human volunteers. This is the traditional, most widely used method. Around 95% of generic oral solid drugs still rely on it. Here’s how it works: 24 healthy adults are enrolled in a crossover study. They take the brand-name drug in one period, then after a washout period (usually a week or two), they take the generic. Blood samples are drawn over 24 to 72 hours to track how the drug moves through their system.
Why use humans? Because the body is messy. Stomach acid, gut motility, enzyme activity, food in the stomach, even genetics-all these affect how a drug is absorbed. In vivo testing captures all of it. That’s why it’s still required for drugs with complex behavior: those that are affected by food, those with nonlinear absorption, or those where the site of action isn’t the bloodstream (like asthma inhalers that work in the lungs).
But it’s expensive. A single in vivo study costs between $500,000 and $1 million. It takes 3 to 6 months from start to finish. You need certified clinical sites, trained staff, ethical approvals, and strict data systems that meet FDA’s 21 CFR Part 11 rules. And while it’s safe for healthy volunteers, it’s not risk-free. Some people experience mild side effects. That’s why regulators push for alternatives when possible.
In Vitro Testing: The Lab-Based Shortcut
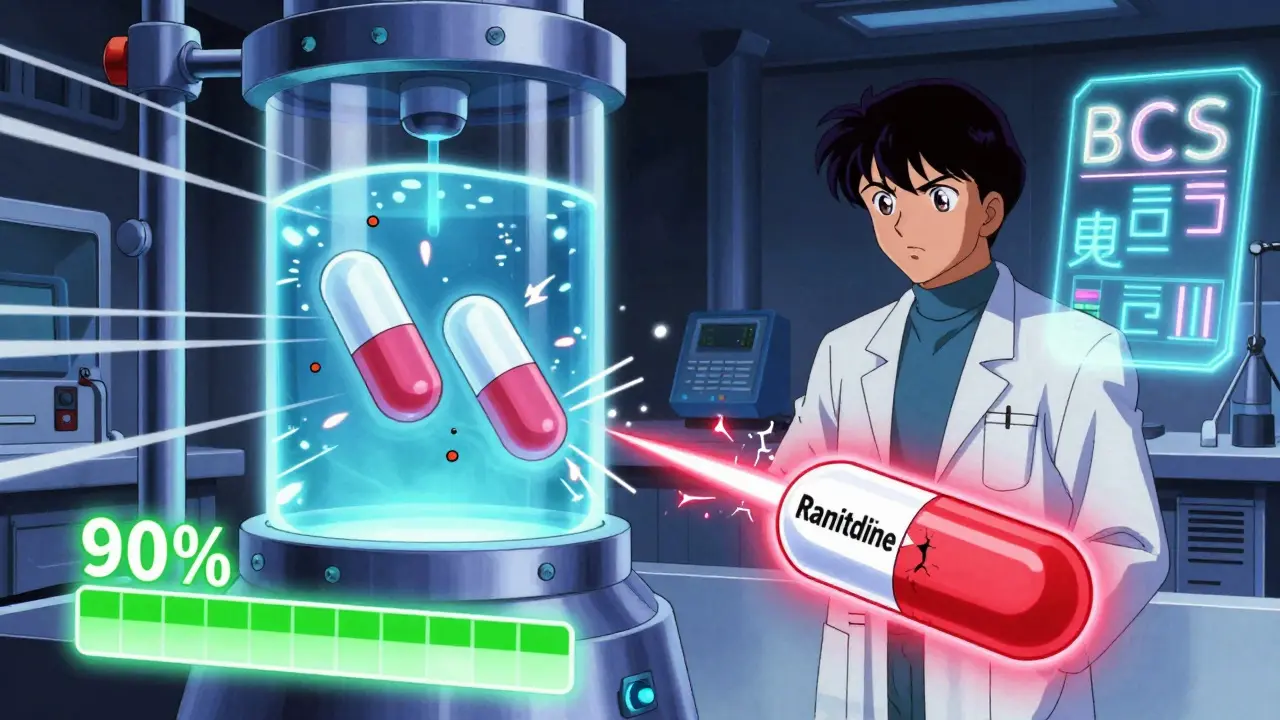
In vitro means “in glass.” These are lab tests done outside the body. Think dissolution machines that dissolve pills in simulated stomach fluid, laser devices that measure droplet size in inhalers, or microscopes that count particle sizes in creams. These tests are precise, repeatable, and don’t involve people.
For simple, fast-dissolving drugs-especially BCS Class I drugs (high solubility, high permeability)-in vitro testing can be just as reliable as human studies. In fact, the FDA granted 78% of biowaivers for BCS Class I drugs in 2021 based solely on in vitro data. That means companies skipped the human trial entirely. One Teva scientist reported saving $1.2 million and 8 months by using an in vitro method instead of an in vivo study. The catch? It took them 3 extra months to develop and validate the dissolution method to FDA standards.
Why is this possible? Because for these drugs, dissolution in the gut is the only step that matters. If the pill dissolves the same way in a test tube as the brand-name version, it’ll likely behave the same in your body. In vitro dissolution testing has a coefficient of variation (CV) under 5%, compared to 10-20% in human studies. That’s more consistent. And it’s cheaper: $50,000 to $150,000 per study, with results in 2-4 weeks.
When Do Regulators Let You Skip the Human Trial?
Not every drug qualifies for in vitro testing. The FDA and EMA have clear rules. You can often avoid in vivo testing if:
- Your drug is BCS Class I (like metoprolol or atenolol).
- You’re making a generic version of an immediate-release tablet with the same formulation and manufacturing process.
- Your drug is a topical cream or ointment that acts locally (like clotrimazole for athlete’s foot), where blood levels don’t matter.
- You’re making an inhaler or nasal spray, and you’ve validated your in vitro method with cascade impactor testing and physiologically relevant dissolution.
For example, in October 2022, the FDA approved Teva’s generic budesonide nasal spray based entirely on in vitro data-no human subjects involved. That was a milestone. It showed regulators were ready to accept advanced lab methods for complex delivery systems.
But if your drug is BCS Class III (low solubility, high permeability), in vitro methods only predict in vivo performance about 65% of the time. That’s not good enough. For drugs like ranitidine or cimetidine, you still need human data.
Why In Vivo Is Still Necessary
Just because in vitro testing is cheaper doesn’t mean it’s always better. There are situations where human testing is non-negotiable:
- Narrow therapeutic index drugs-warfarin, digoxin, phenytoin. A tiny difference in absorption can cause bleeding or seizures. Regulators won’t trust a test tube here.
- Food effects-some drugs only work if taken with food. You need to test both fasting and fed states.
- Nonlinear pharmacokinetics-where doubling the dose doesn’t double the blood level. Human studies are needed to see how the body responds.
- Local action drugs-like inhaled corticosteroids. Blood levels don’t reflect lung concentration. In vitro testing helps, but human data confirms delivery.
One real-world lesson: a topical antifungal product approved via in vitro testing had to be pulled for a post-marketing in vivo study after reports of reduced effectiveness. The company spent $850,000 and lost 11 months. In vitro didn’t catch a subtle difference in how the drug penetrated skin layers.
The Rise of Hybrid Models
The future isn’t in vivo OR in vitro. It’s in vivo AND in vitro-with modeling in between. The FDA is pushing for IVIVC (in vitro-in vivo correlation) models. These are mathematical relationships built from data: if a drug dissolves 90% in 30 minutes at pH 1.2, then it will reach a certain Cmax in humans. When the correlation is strong (r² > 0.95), regulators accept in vitro as a stand-in.
Even more advanced? Physiologically based pharmacokinetic (PBPK) modeling. This uses computer simulations to predict how a drug behaves based on anatomy, physiology, and chemistry. The FDA approved its first PBPK-based generic in 2022. It’s not common yet, but it’s growing fast.
By 2025, the FDA plans to release two new guidances on in vitro testing for complex products like nasal sprays and injectables. The goal? To make in vitro the default for most generics, with in vivo reserved only for the riskiest cases.
What This Means for Patients and Manufacturers
For patients, this shift means faster access to affordable generics. For manufacturers, it means lower costs and quicker approvals-but higher upfront investment in lab tech and expertise. A single USP apparatus 4 flow-through cell (needed for advanced dissolution testing) costs $85,000 to $120,000. Companies need scientists trained in biopharmaceutics, not just pharmacists or chemists.
Regulatory agencies are catching up. The EMA approved 214 biowaivers based on in vitro data in 2022-a 27% jump from 2020. Japan and the U.S. now align on BCS Class I waivers. Global harmonization is real.
But don’t mistake this for a total replacement. In vivo testing isn’t going away. It’s being reserved for the high-stakes cases. The goal isn’t to eliminate human testing-it’s to use it wisely.
Bottom Line
In vivo testing is the full-body scan. In vitro is the X-ray. One shows everything. The other shows what matters-when you know what to look for. For simple, well-understood drugs, in vitro is faster, cheaper, and just as accurate. For complex, high-risk, or poorly understood drugs, nothing beats testing in real people. The best approach? Use the right tool for the job. And increasingly, regulators are letting manufacturers choose-so long as they can prove it works.



Emily P - 20 December 2025
Interesting how the FDA’s 80-125% window feels so arbitrary until you realize how much variation there is in human metabolism. I’ve read papers where Cmax differences of 10% led to clinically significant outcomes in elderly patients on anticoagulants. It’s not just math-it’s biology playing dice with your life.
Vicki Belcher - 21 December 2025
SO COOL!! 🌟 Finally, someone explained this without making my eyes glaze over. In vitro = lab magic, in vivo = real human chaos. And yes, Teva saving $1.2M?? YES PLEASE. More affordable meds = happier me 💊❤️
Jedidiah Massey - 22 December 2025
One must acknowledge the epistemological superiority of in vivo models-they encapsulate systemic pharmacodynamic feedback loops that in vitro dissolution profiles simply cannot capture, regardless of R² values. The BCS classification is a heuristic, not a law. To privilege in vitro data without IVIVC validation is to commit a Type I error in therapeutic equivalence.
pascal pantel - 23 December 2025
Lmao another ‘FDA-approved’ generic. You think a dissolution curve in pH 1.2 buffer actually predicts what happens when someone’s stomach is full of pizza and beer? Wake up. Most of these ‘biowaivers’ are corporate loopholes. And don’t get me started on how they skip post-marketing studies until someone dies.
Sahil jassy - 24 December 2025
In vitro for simple drugs, in vivo for the risky ones. Makes sense. Save money, save time, save lives. Good job science 👍
Nicole Rutherford - 26 December 2025
Of course they’re pushing in vitro. It’s cheaper. But let’s be real-regulators don’t care about safety. They care about speed to market. That’s why you see these ‘approved’ generics failing in the real world. And now they’re using computer models? Please. You can’t simulate human biology with a spreadsheet.
Mark Able - 26 December 2025
Wait so if I take a generic and it doesn’t work, is it because of the test method or because I’m just weird? I’ve had generics that made me feel like a zombie and others that worked better than the brand. Is that just me? Can we test for that? Should we all get DNA tested before taking meds?
Chris Clark - 27 December 2025
Man, I love how this whole thing is like a science fair project gone corporate. Dissolution machines, PBPK models, cascade impactors-sounds like NASA stuff. But at the end of the day, if your pill don’t dissolve right in your gut, you’re just swallowing plastic. And yeah, I once took a generic for my anxiety and it felt like someone turned down the volume on my brain. Took me weeks to realize it was the generic. Not cool.
Carolyn Benson - 28 December 2025
Is this not just another iteration of the Enlightenment’s false dichotomy-reductionism versus holism? We reduce the body to pharmacokinetic curves, then pretend those curves are the soul of efficacy. But the human organism is not a closed system. It is a narrative, a history, a constellation of microbiomes, traumas, and metabolic idiosyncrasies. To replace lived experience with a dissolution profile is to mistake the map for the territory. And the FDA? They’re not regulators-they’re accountants in lab coats.
Chris porto - 28 December 2025
It’s kinda beautiful how science is learning to be smarter, not just harder. You don’t need to test on people if you can prove the pill behaves the same in the lab. It’s like using a compass instead of walking the whole trail. Saves time, saves money, saves people from needles. Just gotta make sure the compass is calibrated right.
Aadil Munshi - 29 December 2025
Oh wow, so the FDA lets you skip human trials if your drug is ‘BCS Class I’? That’s like saying ‘if your car is red, it’ll drive fine in a hurricane.’ And now they’re using computer models? Next thing you know, we’ll be approving drugs based on TikTok trends. 🤡
Danielle Stewart - 30 December 2025
For anyone worried about generics: if your doctor prescribes it and you’re not having side effects, it’s probably fine. The system isn’t perfect, but it’s rigorously checked. And honestly? I’ve taken generics for 15 years-never had an issue. Don’t let fear-mongers scare you. Science > hype.
jessica . - 31 December 2025
Who’s funding these ‘in vitro’ studies? Big Pharma. And who controls the FDA? Big Pharma. They want to cut costs. They don’t care if your kid has a seizure because the generic didn’t dissolve right. This is a conspiracy. The government is letting them poison us with cheap pills. Wake up, sheeple.