Every year, more than 36 million older adults in the U.S. fall-and nearly 32,000 of them die from it. Falls aren’t just accidents. For many, they’re the quiet result of a medication that was never meant to be taken long-term. Sedating drugs like benzodiazepines, antidepressants, and opioids are commonly prescribed to manage sleep, anxiety, or pain in older adults. But these same drugs can turn a steady walk into a stumble, and a stumble into a broken hip or worse. The good news? Most of these falls are preventable-not by adding more safety gear, but by reviewing what’s in the medicine cabinet.
Why Sedating Medications Increase Fall Risk
Sedating medications don’t just make you drowsy. They slow down your brain’s ability to process balance, react to changes in terrain, or recover from a misstep. Drugs like diazepam, amitriptyline, and oxycodone affect the central nervous system, leading to dizziness, delayed reflexes, and confusion. These effects get worse when multiple drugs are taken together. This is called polypharmacy-when someone takes three or more medications daily. The more drugs, the higher the risk. A 2021 study found that each additional medication increased fall risk by about 10%. Some medications carry especially high risks. Baclofen, a muscle relaxant, has the highest documented fall risk among its class. Antidepressants like trazodone and amitriptyline can cause orthostatic hypotension-a sudden drop in blood pressure when standing up. Opioids, even at moderate doses, double the chance of falling in people over 65. And benzodiazepines? They’re among the most dangerous. Even short-term use can impair coordination for hours after taking the pill.What Are FRIDs? The Hidden List of Fall Risks
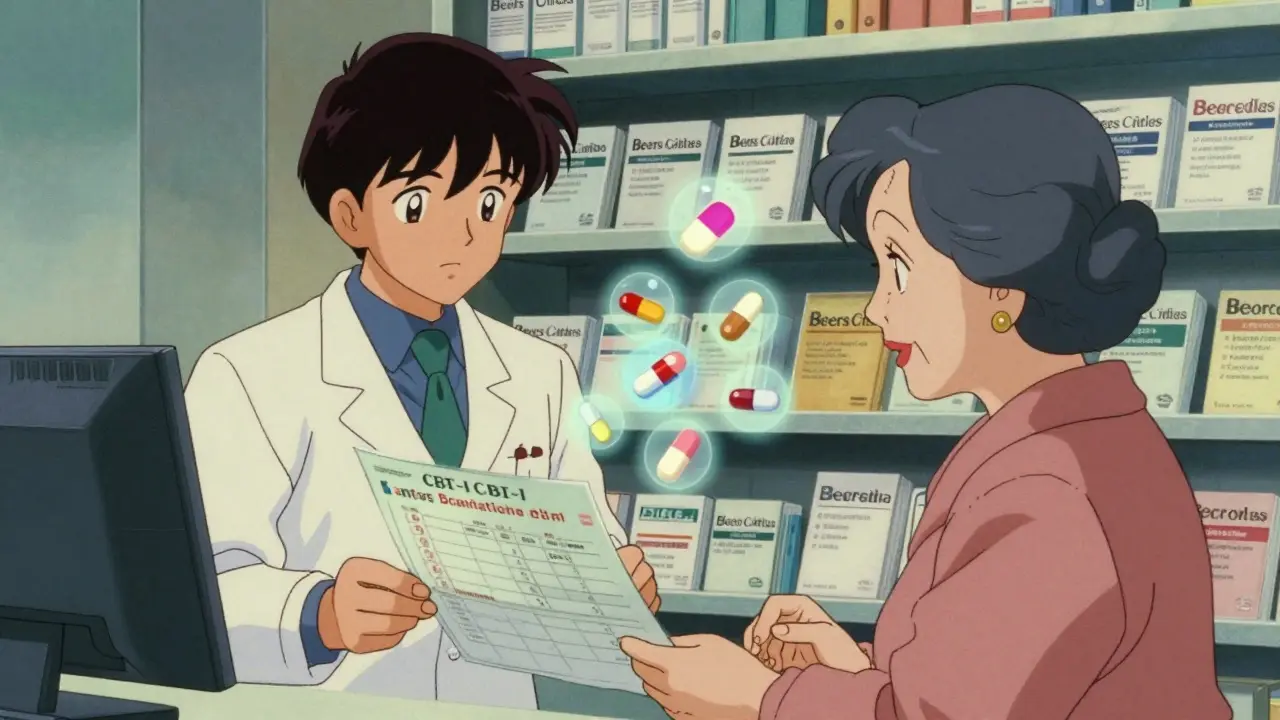
FRID stands for Fall Risk Increasing Drug. It’s not a household term, but it should be. The American Geriatrics Society’s Beers Criteria, updated in 2023, lists dozens of medications that fall into this category. These include:- Anticonvulsants (like gabapentin and pregabalin)
- Antidepressants (especially tricyclics and sedating SSRIs)
- Antipsychotics (used for dementia-related agitation)
- Benzodiazepines and other sedative-hypnotics (like lorazepam and zolpidem)
- Antihypertensives (especially when blood pressure drops too low)
- Opioids (codeine, hydrocodone, oxycodone)
- Antispasmodics and muscle relaxants (like cyclobenzaprine and baclofen)
The STEADI-Rx Approach: A Proven System for Prevention
The CDC’s STEADI-Rx program is the gold standard for tackling medication-related falls. It’s not a suggestion. It’s a step-by-step system used in pharmacies and clinics across the U.S. since 2019. It has three clear parts:- Screen-Ask if the person has fallen in the past year, feels unsteady, or is afraid of falling. A simple yes answers the first red flag.
- Assess-Review every medication on the list. Look for FRIDs, check for drug interactions, and note if the person is taking multiple drugs from the same class.
- Intervene-Work with the prescriber to adjust, reduce, or replace risky medications.
Medication Review Alone Isn’t Enough
You can’t fix a fall risk problem with pills alone. Studies show that the most effective approach combines medication review with physical activity. The Cochrane Review found that exercise programs-especially those focused on balance, strength, and gait training-reduced falls by up to 29%. When paired with medication changes, the results are even stronger. A 65-year-old woman taking amitriptyline for nerve pain and a nightly dose of zolpidem for sleep might be told to stop both. But without a plan to rebuild her balance, she’s still at risk. That’s why physical therapy is part of the solution. Simple exercises like standing on one foot, heel-to-toe walking, or using a resistance band for leg strength can make a huge difference. Programs that meet 30-90 minutes, 2-3 times a week for at least 12 weeks show the best outcomes. Vitamin D is often suggested too. But the evidence is mixed. The U.S. Preventive Services Task Force recommends 800 IU daily, but some studies show no benefit. Still, if someone is deficient-which is common in older adults-it helps. Don’t rely on it alone, but don’t ignore it either.Why It’s So Hard to Change Medications
If the solutions are clear, why are so many older adults still on risky drugs? One reason: fear. Many patients believe their medication is the only thing keeping them calm, sleeping, or pain-free. A 2021 survey by the National Council on Aging found that 63% of older adults resisted deprescribing because they worried symptoms would return. Another reason: doctors don’t always know what’s being taken. A patient might see three different providers and get prescriptions from each-none of them aware of the full picture. Pharmacists are often the missing link. In community pharmacies, they’re the ones who see the full list of meds, catch duplicates, and spot interactions. But only 45% of pharmacists report having enough time to do full medication reviews. And even when they do, prescribers sometimes ignore their recommendations. Real change needs teamwork. A pharmacist flags a risky combination. The doctor reviews it. The patient gets educated. Then, a physical therapist steps in. That’s the ideal. But it only works if systems support it.
What You Can Do Right Now
You don’t need a fancy program to start reducing fall risk. Here’s what you can do today:- Make a complete list-Write down every medication, supplement, and over-the-counter pill you take. Include doses and why you take them.
- Ask your pharmacist-Bring the list to your pharmacy. Ask: “Which of these could make me unsteady or increase my fall risk?”
- Ask your doctor-“Is this medication still necessary? Are there safer alternatives?” Don’t be afraid to say, “I’m worried about falling.”
- Start moving-Even 10 minutes a day of balance exercises helps. Try standing on one foot while brushing your teeth. Walk heel-to-toe along a wall.
- Check your home-Remove throw rugs, install grab bars in the bathroom, and make sure stairs have railings on both sides.
The Bigger Picture
Falls aren’t just a health issue-they’re a system failure. We prescribe sedating drugs too easily and forget to ask: “Is this helping more than it hurts?” With the number of people over 65 expected to hit 80 million in the U.S. by 2040, this problem will only grow. But the tools to fix it already exist. The CDC’s STEADI-Rx program, the Beers Criteria, pharmacist-led reviews, and evidence-based exercise programs are all proven. What’s missing is consistent implementation. The goal isn’t to eliminate all medications. It’s to make sure every pill you take is truly necessary-and that the risks are understood and managed. For older adults, staying steady on their feet isn’t about luck. It’s about smart choices, teamwork, and asking the right questions.What are the most dangerous sedating medications for fall risk in older adults?
The highest-risk medications include benzodiazepines (like diazepam and lorazepam), sedating antidepressants (such as amitriptyline and trazodone), opioids (like oxycodone and hydrocodone), and muscle relaxants (especially baclofen). These drugs slow reaction time, cause dizziness, and impair balance. Even a single dose can increase fall risk, and the danger grows with multiple medications or higher doses.
Can stopping a sedating medication reduce fall risk?
Yes-often dramatically. A 2021 study showed that switching from a high-risk medication to a safer alternative reduced falls by up to 30% within six months. For example, replacing a nightly benzodiazepine with cognitive behavioral therapy for insomnia led to zero nighttime falls in several case reports. However, stopping abruptly can be dangerous. Always work with a doctor or pharmacist to taper safely.
How often should older adults have their medications reviewed?
At least once a year, or anytime a new medication is added, a dose is changed, or after a fall. For those on three or more medications, quarterly reviews are ideal. Pharmacists trained in geriatric care can conduct these reviews and flag potential risks before they lead to injury.
Is vitamin D effective for preventing falls in older adults?
The evidence is mixed. The U.S. Preventive Services Task Force recommends 800 IU daily for older adults at risk of falls, citing modest benefits. But a Cochrane review found no significant reduction in falls from vitamin D alone. It may help if someone is deficient, but it should never replace medication review or exercise. Think of it as a small piece of the puzzle, not the solution.
What role do pharmacists play in fall prevention?
Pharmacists are frontline defenders against medication-related falls. They review all prescriptions, spot dangerous combinations, identify FRIDs, and communicate with prescribers using tools like the CDC’s Provider Consult Form. In the STEADI-Rx program, pharmacists made recommendations in 75% of cases, and most involved switching to a safer drug. Yet, only 45% of pharmacists feel they have enough time to do this thoroughly-highlighting the need for better support and reimbursement.
Are there alternatives to sedating medications for sleep or anxiety?
Yes. For insomnia, cognitive behavioral therapy (CBT-I) is just as effective as sleep meds and has no fall risk. For anxiety, non-sedating antidepressants like sertraline or escitalopram are often safer long-term options. Non-drug strategies like mindfulness, light therapy, and regular movement can also help. Always discuss alternatives with your provider before stopping any medication.




Winni Victor - 25 December 2025
So let me get this straight-we’re telling grandmas to stop their benzos because they might trip over a rug, but the same people who wrote this article are probably sipping kombucha and doing yoga while their kid’s TikTok account has 2M followers? I’m not saying meds are perfect, but if you think a 78-year-old man suddenly switching to chair yoga is gonna fix a decade of insomnia and anxiety, you’re sipping the Kool-Aid with the glitter in it. 🤡
Bailey Adkison - 26 December 2025
Medication reviews are not optional. They are medical necessities. The CDC’s STEADI-Rx protocol is evidence-based, peer-reviewed, and implemented in over 800 clinics. Ignoring it is negligence. Period.
Katherine Blumhardt - 27 December 2025
my uncle took zolpidem for 8 years and then stopped cold turkey and now he thinks the government is spying on him through his pacemaker. i dont know what to believe anymore 😭
Rick Kimberly - 29 December 2025
It is imperative to recognize that polypharmacy among geriatric populations represents a significant public health concern. The pharmacokinetic alterations associated with aging necessitate a reevaluation of therapeutic regimens, particularly those involving CNS depressants. Empirical data from the Beers Criteria substantiate the correlation between medication burden and fall incidence. A multidisciplinary approach remains the cornerstone of intervention.
Lindsay Hensel - 30 December 2025
I’ve seen this. My mother was on three sedatives. She stopped two. Started balance classes. Now she dances with her grandkids. It’s not magic. It’s care.
Mussin Machhour - 31 December 2025
Yo if you’re 70 and on benzos, just try walking barefoot on grass for 10 mins a day. Seriously. It’s free, it’s calming, and your feet will thank you. No pills needed.
Carlos Narvaez - 1 January 2026
STEADI-Rx? Cute acronym. But let’s be real-pharmacists aren’t doctors. They’re glorified cashiers with a pharmacy degree. Let the professionals handle this.
Harbans Singh - 2 January 2026
In India, we don’t have access to all these fancy programs. But we have family. We watch our elders. We make sure they don’t climb ladders. We cook them turmeric tea. Sometimes, simple love beats a prescription.
Zabihullah Saleh - 4 January 2026
It’s funny how we treat aging like a glitch to be fixed with pills. What if the real problem isn’t the meds-but the fact that we’ve stopped listening to older people? They’re not broken. We just stopped making space for them.
Oluwatosin Ayodele - 5 January 2026
You think this is new? In 2008, I worked in a Nigerian hospital where elders were given diazepam for ‘nervousness’-no diagnosis, no follow-up. We called it ‘spirit medicine’. Same thing. America just calls it ‘standard care’. Wake up.
Jason Jasper - 6 January 2026
I know a guy who quit his antidepressant after a fall. He said he felt ‘lighter’-not just physically. Like the weight of the pills had been holding him down longer than the meds had helped.
sagar patel - 7 January 2026
Pharmacists are the real heroes here. They see the full list. Doctors don’t even know what their patients are taking. This is systemic failure and everyone knows it but nobody fixes it
Linda B. - 8 January 2026
Of course they blame the meds. What about the fluoride in the water? The 5G towers? The fact that every pill comes with a warning label but nobody reads them? This is all part of the pharmaceutical control agenda. You think they want you to walk better? No-they want you to keep buying.
Christopher King - 9 January 2026
They don’t want you to fall because then you’ll die and they won’t have to pay for your hospice. They want you to be docile, sedated, and silent. The real enemy isn’t benzodiazepines-it’s the system that profits from your fragility. Wake up. The fall isn’t an accident. It’s a feature.