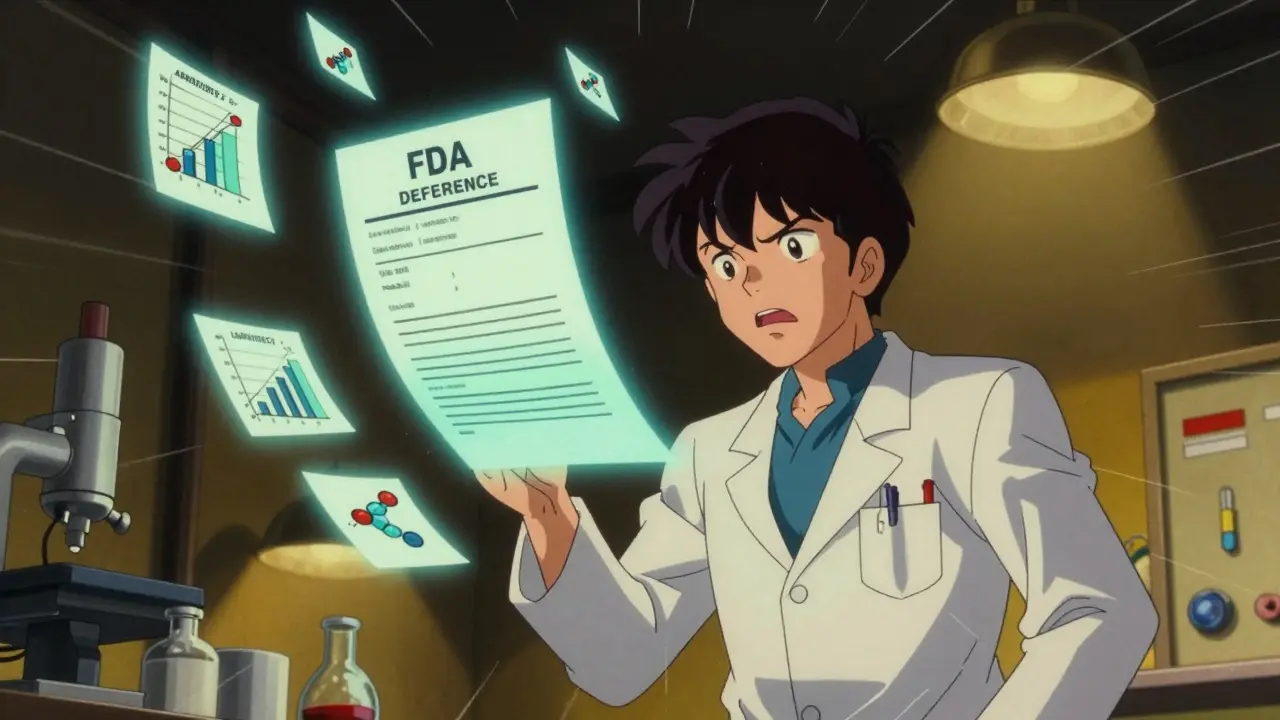
When a generic drug company submits an application to the FDA, it’s not a simple yes-or-no decision. Most applications don’t get approved on the first try. Instead, they get a deficiency letter-a formal notice listing everything the FDA thinks is wrong or missing. These letters aren’t just bureaucratic delays. They can cost companies millions and delay life-saving medications from reaching patients for over a year.
What Exactly Is a Deficiency Letter?
A deficiency letter from the FDA is a detailed breakdown of why an Abbreviated New Drug Application (ANDA) can’t be approved yet. It’s not a rejection. It’s a roadmap. The FDA tells applicants exactly what needs to be fixed: missing data, flawed methods, unclear documentation, or failure to prove the drug is the same as the brand-name version. These letters emerged as a formal process in 2003, replacing vague feedback with standardized, actionable feedback. Today, over 70% of all major issues in ANDAs are quality-related. That means most problems aren’t about safety or efficacy-they’re about how the drug is made, tested, or described.Top 5 Deficiency Categories in Generic Drug Applications
Based on FDA data from 2023 and 2024, these are the most common reasons generic drug applications get stuck:- Dissolution Issues (23.3%)-This is the #1 problem. The FDA requires generic drugs to dissolve in the body at the same rate and extent as the brand-name drug. If the dissolution method doesn’t match real-world conditions-like using outdated lab equipment or testing at only one pH level-the application fails. Many companies still use Apparatus 2 for all products, even when modified-release tablets need Apparatus 3 or 4.
- Drug Substance Sameness (19%)-The active ingredient must be chemically and physically identical to the reference drug. For complex molecules like peptides, this means proving the protein’s folding, aggregation, and secondary structure match. Missing circular dichroism or size-exclusion chromatography data is a common reason for failure.
- Unqualified Impurities (20%)-Every drug has impurities. The FDA requires toxicology studies for any impurity above certain thresholds. Many applicants skip this step or assume ICH guidelines don’t apply to them. The result? A 14- to 18-month delay while they run new animal studies.
- Elemental Impurities (13%)-Heavy metals like lead, cadmium, or arsenic can sneak into drugs through raw materials or manufacturing equipment. The FDA’s ICH Q3D guidelines set strict limits. Companies often submit incomplete risk assessments or fail to test final products.
- Manufacturing and Process Controls (18%)-The FDA wants to know exactly how the drug is made at commercial scale. If the bioequivalence batch doesn’t reflect the real production line, or if process changes aren’t documented, the application gets flagged. Many small companies use lab-scale equipment and assume it’s enough.
Why Do Some Companies Keep Failing?
It’s not just about technical mistakes. The biggest gap is between academic development and real-world manufacturing. A 2023 study found that nearly half of all Drug Substance sameness failures come from researchers who developed the drug in a university lab but never worked in a GMP facility. They focus on purity and yield, not consistency, scalability, or control strategies. Another issue? Poor communication. A 2023 survey of 127 generic manufacturers found that 78% said they didn’t understand why the FDA flagged certain issues. They’d get a letter saying “inadequate control strategy” but no example of what adequate looks like. That’s changing. In April 2025, the FDA released template responses for the 10 most common deficiencies. Now, applicants can see exactly what data the agency expects-for example, how many pH conditions to test for dissolution, or what analytical methods are required for peptide characterization.
Complex Drugs Are the Biggest Challenge
Not all generic drugs are created equal. Immediate-release tablets? Relatively straightforward. Modified-release tablets? Peptides? Topical creams? These are “complex generics,” and they’re where most failures happen. Despite making up only 22% of all ANDA submissions, complex generics account for 38% of deficiency letters. Why? Because they’re harder to characterize, harder to replicate, and harder to prove bioequivalence for. For example, a modified-release tablet might need 10+ dissolution points across different pH levels, plus in vivo studies to prove the release profile matches the brand. Many companies try to shortcut this with just three time points and a single pH. The FDA catches it every time. Companies that invest in Quality by Design (QbD) from the start-mapping critical quality attributes early, using risk assessments, and building controls into the process-see deficiency rates drop by 40% or more.Who Gets Approved on the First Try?
The odds aren’t equal across the industry. Companies with 50 or more approved ANDAs have a deficiency rate 22% lower than those with fewer than 10. Why? Experience. They’ve seen these letters before. They know what the FDA expects. They’ve built internal teams with regulatory, analytical, and manufacturing experts who talk to each other. Also, companies that request a pre-ANDA meeting with the FDA are 32% less likely to get a deficiency letter. That meeting isn’t optional for complex products. It’s a safety net. The FDA’s Competitive Generic Therapy (CGT) program shows what’s possible. Products in this program get extra guidance and priority review. Over 73% of CGT applications get approved on the first cycle-compared to just 52% for the rest.
How to Avoid a Deficiency Letter
If you’re submitting an ANDA, here’s what actually works:- Use the latest FDA guidance documents-Don’t rely on old versions. The May 2021 dissolution guidance, ICH Q3D for elemental impurities, and M7 for mutagenic impurities have all been updated. Missing one update can sink your application.
- Test under biorelevant conditions-Dissolution isn’t just about speed. It’s about how the drug behaves in the gut. Use media that mimics stomach and intestinal fluids, not just water or buffer.
- Match your bio-batch to commercial scale-If your bioequivalence batch was made in a 10-liter reactor but your commercial line runs at 500 liters, the FDA will ask for justification. If you can’t prove they’re equivalent, expect a deficiency.
- Document everything-Applications with detailed development reports have 27% fewer deficiencies. Don’t just say “we tested it.” Show the data, the method, the rationale, and the control strategy.
- Request a pre-submission meeting-Especially for complex products. It’s free. It’s confidential. And it can save you 18 months.
The Cost of a Deficiency Letter
Every delay costs money. A 2023 study found that each additional review cycle adds $1.2 million in costs-more for delays caused by toxicology studies or process changes. But the real cost is patient access. When a generic drug is delayed, patients pay more for brand-name versions. The U.S. generic drug market is worth $110 billion. Every deficiency letter that holds up a product means millions in lost savings. The FDA knows this. That’s why they’re launching new tools. By Q3 2026, they plan to roll out AI-assisted pre-submission screening. It will flag common errors-like missing M7 assessments or incorrect apparatus selection-before the application even reaches a reviewer. Industry experts predict that with these changes, first-cycle approval rates could jump from 52% to 68% by 2027. That’s 15 to 20 more generic drugs hitting the market every year.Final Thought: It’s Not About Luck
Getting an ANDA approved isn’t about luck. It’s about preparation. The FDA doesn’t hide its expectations. They publish guidelines, host forums, and release templates. The problem isn’t that the rules are unclear-it’s that too many companies don’t read them. The companies that succeed don’t just submit applications. They study the letters. They learn from others’ mistakes. They invest in expertise. And they treat the FDA as a partner, not a hurdle. If you’re working on a generic drug application, don’t wait for the deficiency letter. Start preparing for it now.What happens after you receive a deficiency letter from the FDA?
After receiving a deficiency letter, you have 12 months to respond with the requested data or corrections. You must submit a formal response that addresses each point raised by the FDA. The agency then reviews your reply and either approves the application, issues another deficiency letter, or withdraws the application. Missing the deadline or failing to fully address the issues typically results in refusal to approve.
Can you appeal a deficiency letter from the FDA?
You can’t formally appeal a deficiency letter, but you can request a meeting with the FDA to discuss the issues. This is called a “reconsideration meeting.” You can present new data, clarify misunderstandings, or ask for clarification on the agency’s expectations. Many companies use this step to avoid a second deficiency letter. However, if the FDA stands by its original findings, you must fix the issues before resubmitting.
How long does it take to resolve a deficiency letter?
Resolution time varies. Simple issues like missing documentation can be fixed in 2-3 months. Complex problems-like generating new toxicology data for impurities or redesigning a dissolution method-can take 12 to 18 months. The FDA gives you 12 months to respond, but if you need more time, you can request an extension. Delays beyond that often lead to application withdrawal.
Do deficiency letters apply to all generic drugs?
Yes, all Abbreviated New Drug Applications (ANDAs) are subject to deficiency letters. However, the likelihood and complexity vary. Simple immediate-release tablets have lower deficiency rates. Complex products like peptides, modified-release formulations, and topical dermatologicals are far more likely to receive detailed deficiency letters due to their technical challenges and higher scrutiny.
Is there a way to reduce the chance of getting a deficiency letter?
Yes. Companies that invest in pre-submission meetings, use Quality by Design (QbD) principles, follow the latest FDA guidance, and ensure their bioequivalence batches reflect commercial manufacturing see significantly lower deficiency rates. Using the FDA’s new template responses for common issues also helps. Early engagement and thorough documentation are the most effective ways to avoid delays.



Ryan W - 27 January 2026
Let’s be real - this whole system is a joke. The FDA spends more time nitpicking dissolution methods than actually ensuring patient safety. Meanwhile, Indian manufacturers are pumping out 80% of the world’s generics, and they’re getting slapped with deficiency letters for using the wrong apparatus? Wake up. This isn’t regulation - it’s protectionism disguised as science.
Renia Pyles - 27 January 2026
Oh please. You act like the FDA is the villain here, but guess what? The companies that keep failing are the ones who treat this like a homework assignment they didn’t study for. If you can’t even follow ICH Q3D or use biorelevant media, you don’t deserve to make medicine. Stop blaming the regulators for your incompetence.
Conor Flannelly - 29 January 2026
There’s something deeply human here - we treat medicine like a product line, but it’s a lifeline. The FDA’s deficiency letters aren’t red tape; they’re the last guardrail before a kid with asthma gets a cheap inhaler that doesn’t work. I’ve seen what happens when dissolution fails - not in a lab report, but in a hospital bed. The cost isn’t just $1.2M per delay. It’s sleepless nights for families who can’t afford the brand. Maybe we need more empathy in regulation, not less.
Nicholas Miter - 29 January 2026
Biggest thing no one talks about: the people writing these apps are often PhDs who’ve never set foot in a GMP plant. They’re brilliant at chemistry, terrible at scale. I’ve seen guys who can synthesize a peptide in a 50ml flask but have zero clue how to make 500kg without introducing impurities. It’s not the FDA’s fault - it’s the training gap. QbD isn’t a buzzword, it’s survival.
Conor Murphy - 30 January 2026
Man, I remember when my cousin’s company got a deficiency letter for ‘inadequate control strategy.’ They had no idea what that even meant. No examples, no templates, just a wall of jargon. Then the FDA dropped those new templates last year? Game changer. Suddenly, everyone knew what ‘adequate’ looked like. Sometimes the system just needs a little clarity - not more bureaucracy.
Rakesh Kakkad - 31 January 2026
It is imperative to note that the regulatory framework established by the FDA is not merely a guideline but a non-negotiable standard for global pharmaceutical integrity. The assertion that Indian manufacturers are somehow exempt from these protocols is not only inaccurate but dangerously misleading. Compliance is not optional - it is the cornerstone of public health.
Suresh Kumar Govindan - 1 February 2026
QbD? Pre-submission meetings? Please. These are just expensive consultants’ toys. Real manufacturers know: if you’re not cutting corners, you’re losing money. The FDA’s ‘templates’ are just PR to make regulators look helpful. The truth? They want you to fail so they can justify their budgets. You think they want generics to succeed? Think again.
Aishah Bango - 2 February 2026
Let me just say - if you’re submitting an ANDA and you didn’t read the May 2021 dissolution guidance, you’re not just negligent, you’re morally irresponsible. People die waiting for affordable meds because companies treat this like a game of chance. You don’t get to be a doctor of medicine if you don’t study. Why should you get to make medicine without studying the rules?
Marian Gilan - 3 February 2026
Anyone else notice the FDA’s new AI screening tool drops in Q3 2026? Coincidence? Nah. They’ve been secretly collecting all our data since 2020 to train an algorithm that’ll replace reviewers. Next thing you know, your application gets auto-rejected by a bot that doesn’t even know what ‘Apparatus 4’ is. They’re not fixing the system - they’re outsourcing it to a Silicon Valley black box. Wake up.
Patrick Merrell - 4 February 2026
Just submitted my 3rd ANDA. First time ever got approved on the first try. Used every template, did the pre-meeting, matched my bio-batch to commercial scale. Took 18 months of work. Worth it. No more deficiency letters. No more sleepless nights. Just a quiet win for patients. 🤝