Comprehensive Review of TrueCanadaPharmacy.com - Your Trusted Canadian Online Pharmacy for Xifaxan
Dec 31 2023 - Online Pharmacy Reviews
When dealing with pheochromocytoma, a rare catecholamine‑producing tumor that originates in the adrenal medulla. Also known as adrenal medullary tumor, it pheochromocytoma encompasses the adrenal gland, the paired organ atop each kidney that releases hormones into the bloodstream. The tumor’s hallmark is the uncontrolled release of catecholamines, chemical messengers such as adrenaline and noradrenaline that regulate heart rate and blood pressure. This surge directly hypertension, elevated arterial pressure that can spike suddenly during attacks, and fuels the classic triad of pounding headache, profuse sweating, and rapid heartbeat. Understanding these connections helps clinicians recognize the disease early, before organ damage sets in.
Genetic predisposition plays a huge role: mutations in the RET, a gene linked to multiple endocrine neoplasia type 2, VHL, the von Hippel‑Lindau tumor suppressor, and NF1, the neurofibromatosis‑type‑1 gene each increase the risk of developing pheochromocytoma. These inherited forms often present at a younger age and may coexist with other endocrine tumors. Clinically, patients report episodic pounding headaches, trembling, pallor or flushing, and anxiety that mimics panic attacks. The gold‑standard screening test is a plasma free metanephrine assay, which requires accurate laboratory techniques to catch small hormone spikes. Imaging—usually a contrast‑enhanced CT or MRI of the abdomen—then localizes the tumor, while functional scans such as 123I‑MIBG confirm catecholamine activity. Together, biochemical and radiologic data provide a comprehensive picture that guides treatment decisions.
Treatment centers on controlling the hormone surge before safely removing the tumor. First‑line medical therapy employs selective alpha‑blockers (e.g., phenoxybenzamine) to blunt vasoconstriction, followed by beta‑blockers to manage tachycardia; this two‑step approach prevents the dangerous hypertensive crisis that can occur if beta‑blockade is started alone. Once blood pressure is stable, minimally invasive laparoscopic adrenalectomy is the preferred surgical method, offering quicker recovery and lower complication rates than open surgery. In patients with bilateral disease or hereditary syndromes, cortical‑sparing adrenalectomy may preserve some hormone function. Post‑operative follow‑up involves periodic plasma metanephrine checks because recurrence can happen years later, especially in genetically driven cases. Below you’ll find a curated selection of articles that dive deeper into each of these aspects—genetic testing guides, symptom check‑lists, diagnostic algorithms, medication comparisons, and step‑by‑step surgical overviews—so you can explore the full spectrum of pheochromocytoma management.
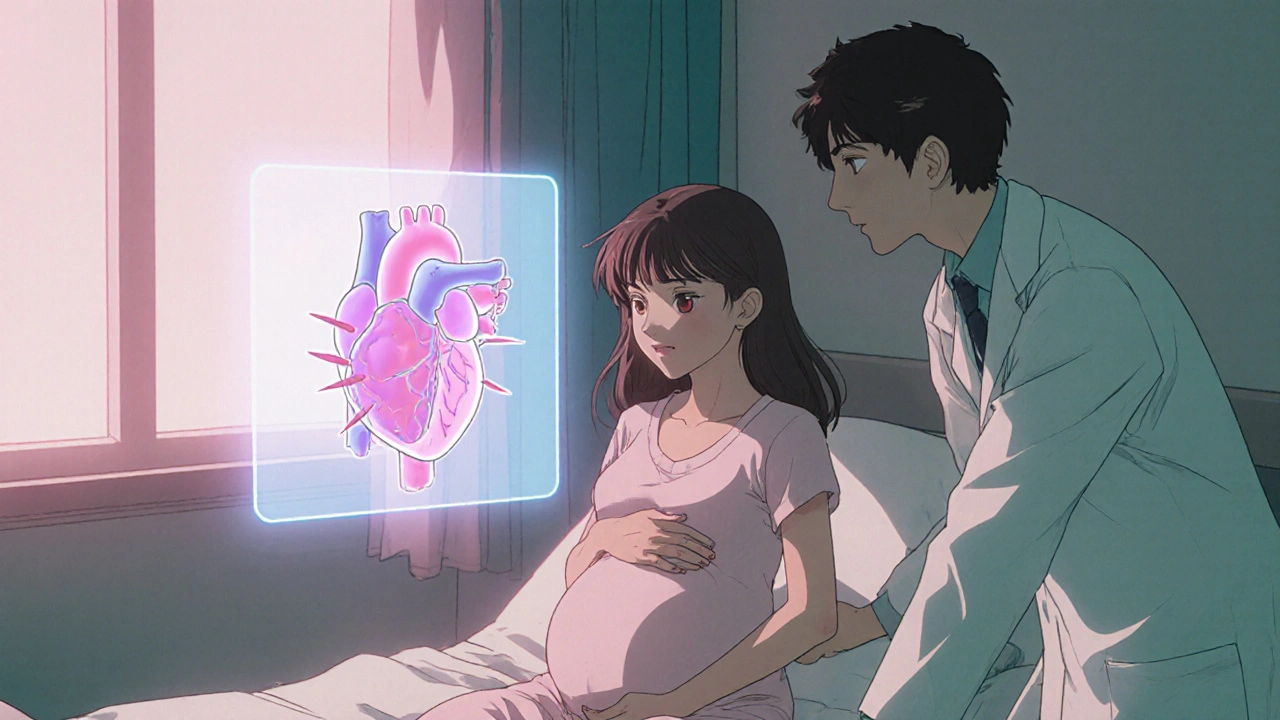
Learn how pheochromocytoma affects pregnancy, spot symptoms, manage risks, choose treatment options, and plan delivery for a safe outcome.
read more© 2026. All rights reserved.
