Mind-Body Practice Selector for Crohn's Disease
Recommended Practices for Your Situation
Each practice has unique benefits for managing Crohn's symptoms. Here's what they offer:
- Meditation: Reduces cortisol levels and eases anxiety
- Yoga: Improves gut motility and reduces pain perception
- Tai Chi: Gentle stretching that builds stress resilience
- Biofeedback: Helps retrain pelvic floor muscles
- Guided Imagery: Visualizes healing and supports pain coping
Tip: Start with one practice for two weeks before adding another.
Key Takeaways
- Mindfulness and related mind‑body practices can lower stress hormones that worsen Crohn’s symptoms.
- Clinical trials show modest reductions in disease activity scores after regular meditation or yoga.
- Start with short, low‑impact sessions and track symptoms to find what works for you.
- Combine mind‑body work with medical treatment; never replace prescribed meds.
- Reliable resources include IBD‑focused apps, local support groups, and certified instructors.
Living with Crohn's disease is a chronic inflammatory bowel condition that causes abdominal pain, diarrhea, and fatigue can feel like a constant battle against your own body. While medication tackles the inflammation, daily stress often fuels flare‑ups. That’s where mind-body practices step in - they don’t cure the disease, but they give you tools to calm the nervous system, improve gut function, and boost quality of life.
Why Stress Matters for Crohn’s
The gut‑brain axis is a two‑way street: emotional stress can alter gut motility, increase permeability, and change the microbiome. In turn, gut inflammation sends signals that heighten anxiety. A 2023 gastroenterology study found that patients reporting high perceived stress had 1.8‑times higher odds of a severe flare within six months.
Understanding this loop helps you see why calming the mind isn’t a fluff supplement - it’s a strategic part of disease management.
Mindfulness Explained
Mindfulness is the practice of paying non‑judgmental attention to the present moment. It can be cultivated through breathing exercises, body scans, or simple awareness of thoughts as they arise. Regular mindfulness practice lowers cortisol, the stress hormone that can aggravate intestinal inflammation.
Evidence Linking Mindfulness to Inflammatory Bowel Disease
Several randomized controlled trials have examined mindfulness‑based stress reduction (MBSR) in IBD patients. One 2022 trial with 120 participants reported a 12‑point drop in the Harvey‑Bradshaw Index (a Crohn’s activity score) after an eight‑week MBSR program, compared to a 3‑point drop in the control group. A meta‑analysis covering six studies concluded that mindfulness interventions yielded a small‑to‑moderate effect size (Cohen’s d ≈ 0.45) on symptom severity.
These numbers don’t replace medication, but they demonstrate a real, measurable benefit that can complement standard care.
Mind‑Body Practices Worth Trying
Beyond formal mindfulness meditation, many movement‑based practices activate the parasympathetic nervous system, which helps calm gut inflammation. Below is a quick snapshot of the most studied options:
| Practice | Typical Session Length | Main Benefit for Crohn’s | Evidence Level |
|---|---|---|---|
| Yoga | 20‑40min | Improves gut motility, reduces pain perception | Moderate (several pilot trials) |
| Meditation | 10‑30min | Lowers cortisol, eases anxiety | Strong (multiple RCTs) |
| Tai Chi | 15‑30min | Gentle stretching, balance improves stress resilience | Emerging (small studies) |
| Biofeedback | 30‑45min | Helps retrain pelvic floor, reduces urgency | Limited (case series) |
| Guided Imagery | 5‑20min | Visualizes healing, supports pain coping | Low (pilot work) |
Getting Started: A Step‑by‑Step Routine
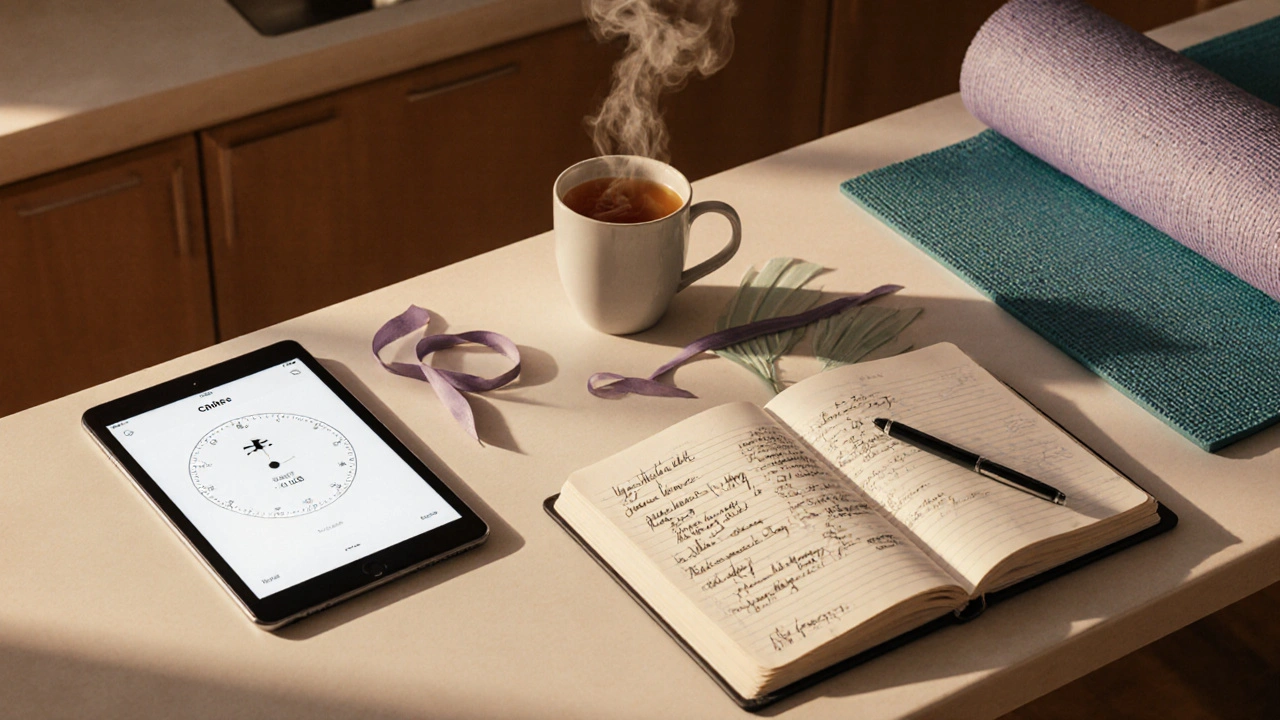
- Choose ONE practice that feels approachable. If you’ve never moved much, start with a seated meditation.
- Set a realistic daily window - even five minutes counts.
- Find a guided resource. Apps like Insight Timer (meditation) or Yoga with Adriene (YouTube yoga) offer free sessions.
- Track symptoms in a simple journal: note pain level, stool frequency, and mood before and after each session.
- Review the log every two weeks. Look for patterns - does a 10‑minute meditation precede a calmer day?
- Adjust duration or style based on what the data tells you. Some weeks a gentle yoga flow may be better; other weeks a quick breathing exercise wins.
- Talk to your gastroenterologist about your practice. They can help you align the routine with medication timing.
Consistency beats intensity. The brain needs repeated exposure to rewire the stress response, just like muscles need regular movement to grow stronger.
Tips, Pitfalls, and Safety
- Listen to your body. If a pose causes sharp abdominal pain, modify or skip it. The goal is relaxation, not strain.
- Avoid practicing immediately after a heavy meal; give digestion a few hours.
- Stay hydrated. Dehydration can amplify flare‑up symptoms, especially during longer yoga sessions.
- Beware of “quick‑fix” claims. No single session will eradicate inflammation - think of it as a supportive habit.
- Combine practices. A 10‑minute meditation followed by a gentle stretch can amplify the calming effect.
Resources and Next Steps
Here are a few trusted places to deepen your practice:
- Crohn’s & Colitis Foundation - offers free webinars on stress management.
- Mindful.org - a library of short, evidence‑backed meditations.
- Yoga for IBD - a specialized online program created by a gastroenterology‑trained yoga therapist.
- Headspace - a subscription app with a free trial that includes a “Stress Less” series.
- Local hospital or community center - many host beginner‑friendly tai chi or mindfulness groups.
Pick one, try it for two weeks, and see how you feel. Small wins add up to a more resilient gut and a calmer mind.
Frequently Asked Questions
Can mindfulness replace my medication?
No. Mindfulness is a complementary tool. It can lower stress‑related flare triggers, but it doesn’t treat the underlying inflammation. Always follow your doctor’s prescription plan.
How often should I practice?
Start with 5‑10 minutes daily. If you feel comfortable, work up to 20‑30 minutes once or twice a day. Consistency matters more than length.
Is yoga safe during a flare?
Gentle, low‑impact poses (like seated twists or child's pose) are usually fine, but avoid deep bends or intense core work that could increase abdominal pressure.
Do I need a certified instructor?
For beginners, guided videos or apps are sufficient. If you have severe disease activity, a certified instructor familiar with IBD can help modify poses safely.
Are there specific meditation techniques for gut health?
Body‑scan meditation, which systematically brings attention to each organ, has been shown to improve interoceptive awareness and may help patients notice early signs of a flare.



Zen Avendaño - 5 October 2025
Thanks for putting together such a thorough guide. I especially love the step‑by‑step routine; it makes it feel doable even on a tough day. The emphasis on tracking symptoms is spot on – data is our friend when we’re managing a chronic condition. I’ve found that starting with a five‑minute meditation and adding a short yoga flow really calmed my flare‑ups. Keep sharing these practical tips, they’re a lifeline for many of us.
Michelle Guatato - 7 October 2025
While the guide looks helpful, have you considered who’s really benefiting from these mind‑body hacks? Big pharma loves to push medication, but they’ll never admit that stress‑reduction could cut their profits. The so‑called "evidence" often comes from tiny studies funded by supplement companies. If you’re not careful, you’ll just be buying another product that keeps the cycle going. It’s worth questioning the motives behind the research they highlight.
Gabrielle Vézina - 9 October 2025
Honestly the whole idea of using mindfulness to tame a gut that’s on fire feels like a romantic notion at best. The gut‑brain axis is a complex mess and not something you can fix with a few deep breaths. You can try meditation but expect only a fleeting calm that won’t halt an actual inflammation flare. Yoga poses might stretch a tight abdomen for a moment but they won’t stop immune cells from attacking the lining. Tai Chi’s gentle moves are soothing but they do not replace steroids when a crisis hits. Biofeedback sounds fancy yet its limited case series can’t convince a skeptic. Guided imagery may paint pretty pictures but the gut still erupts when stress spikes. Consistency is praised but life is chaotic; finding daily quiet is a luxury for many. Tracking symptoms is useful but people often misinterpret normal day‑to‑day variance as progress. The guide’s tip to add one practice for two weeks is prudent yet overly simplistic. For every patient who feels better, there are countless who see no change and get frustrated. The table of evidence levels is helpful but does not convey the quality of the underlying studies. When you read that meditation has "strong" evidence you must ask what "strong" really means – how many participants, blinding, control groups? The promise of a calmer mind is attractive but not a cure, and the article could be clearer about that. In the end, these practices are adjuncts, not replacements, and the tone should reflect the seriousness of Crohn’s disease. So, while the optimism is nice, a more tempered, data‑driven approach would serve readers better.
carl wadsworth - 11 October 2025
Great breakdown, especially the caution about not viewing these tools as a cure. I’d add that pairing a short meditation with a gentle yoga flow can create a synergistic calm that many patients notice. Encourage keeping a simple log – even a bullet‑point note works – to spot real patterns. And remember, it’s perfectly fine to adjust the routine based on how you feel day‑to‑day.
Neeraj Agarwal - 12 October 2025
Your guide is thorough but there are a few points to clarify. The term "strong (multiple RCTs)" should be accompanied by sample sizes – many of those trials involve fewer than fifty participants. Also, "emerging (small studies)" for Tai Chi often lacks proper blinding, which can inflate perceived benefits. Lastly, while you recommend apps, ensure they comply with HIPAA standards if users share health data.
Rose K. Young - 13 October 2025
This post is overly optimistic.
Christy Pogue - 15 October 2025
Love how you kept it practical! The suggestion to start with a five‑minute meditation lowers the barrier for beginners. I’ve tried the Insight Timer app and it really helped me stay consistent during a tough flare. Pairing it with a short yoga video from Yoga with Adriene made my mornings feel gentler. Thanks for the encouragement – it’s exactly the boost many of us need.
Helena Pearson - 16 October 2025
Exactly! 🌟 Starting small builds habit momentum and the brain starts to rewire. I’ve seen my anxiety drop after just ten minutes of guided breathing. Keep sharing these gems – the community thrives on positivity! 🙌
Patricia Fallbeck - 18 October 2025
All this “mind‑body” hype feels like a trendy wellness fad wrapped in scientific jargon. Sure, a few studies hint at benefits, but the majority are underpowered and riddled with bias. People with Crohn’s need hard‑core medical treatment, not a feel‑good mantra. The article glosses over the fact that many of these practices are marketed by profit‑driven wellness brands. If you’re looking for real change, focus on diet and medication adherence, not on chanting “ouch”. 🙄
Brett Snyder - 19 October 2025
While I respect the skepticism, dismissing every mind‑body approach ignores centuries of holistic healing. In many cultures, meditation and gentle movement are core to health, and they’re now being validated by modern science. Let’s not forget that mental resilience can actually improve medication efficacy. So, a balanced view is best – not outright rejection.
Nidhi Jaiswal - 21 October 2025
The guide oversimplifies a complex disease. Tracking symptoms is good but it won’t replace regular check‑ups.
Sunil Sharma - 22 October 2025
Agreed, regular doctor visits are essential. The mindfulness tools can complement treatment, but they’re not a substitute. Keep the focus on a collaborative approach with your healthcare team.