PharmacyEscrow.com Review 2023: Trusted Canadian Online Pharmacy & Affordable Prescription Drugs
Dec 13 2023 - Health and Pharmaceuticals
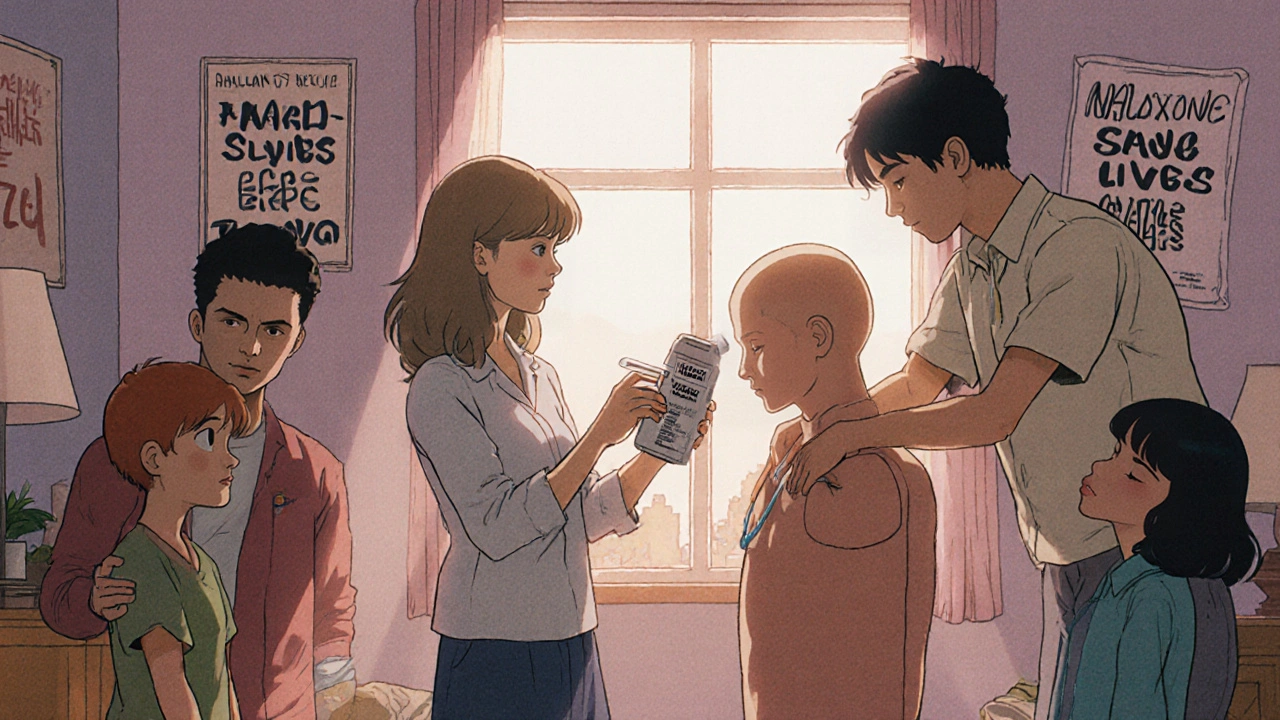
When someone overdoses on opioids, every minute counts. A naloxone readiness plan, a prepared strategy to quickly administer naloxone during an opioid overdose. Also known as overdose response protocol, it’s not just for hospitals—it’s for homes, schools, workplaces, and streets. Naloxone is a safe, FDA-approved medication that can reverse an opioid overdose in minutes. It doesn’t work on other drugs like cocaine or alcohol, but for heroin, fentanyl, oxycodone, or prescription painkillers, it’s often the difference between life and death.
Having a naloxone readiness plan, a prepared strategy to quickly administer naloxone during an opioid overdose. Also known as overdose response protocol, it’s not just for hospitals—it’s for homes, schools, workplaces, and streets. means knowing who’s at risk, where to keep the kit, and how to act fast. People on long-term opioid therapy, those recovering from addiction, and even users who don’t think they’re at risk can suddenly overdose—especially when street drugs are laced with fentanyl. A 2023 CDC report found that over 70% of opioid deaths involved fentanyl, and naloxone is one of the few tools that can stop it in its tracks.
It’s not just about having the drug. It’s about training. You don’t need to be a doctor to use naloxone. Most kits come with simple instructions—inject or spray into the nose, wait 2–3 minutes, and if there’s no response, give a second dose. Keep it in your car, your purse, your medicine cabinet. Teach your family, your coworkers, your friends. Many states now allow pharmacies to hand out naloxone without a prescription. Some community centers, clinics, and even libraries offer free kits and quick training sessions.
And it’s not just for individuals. Schools, shelters, and first responders are building naloxone readiness plans into their daily operations. Emergency crews carry it. Peer support groups train members. Even some churches keep kits on hand. This isn’t about enabling drug use—it’s about keeping people alive long enough to get help. Every overdose reversed is a second chance.
What’s missing from most people’s plans? Knowing what to do after naloxone kicks in. The drug wears off in 30–90 minutes, but opioids can stay in the system much longer. That means someone can stop breathing again after the first dose. Always call 911—even if they wake up. Stay with them. Monitor their breathing. Don’t assume they’re out of danger just because they’re conscious.
There’s also the emotional side. People often feel ashamed or afraid to use naloxone. They worry about legal trouble, judgment, or making things worse. But in most places, Good Samaritan laws protect those who help. The goal isn’t to shame—it’s to save. If you’ve ever wondered if you could handle an overdose, the answer is yes—if you’re ready.
Below, you’ll find real-world guides on opioid monitoring, medication safety, and overdose prevention. These aren’t theoretical articles—they’re tools used by doctors, pharmacists, and families to keep people alive. Whether you’re managing pain, supporting someone in recovery, or just want to be prepared, this collection gives you the facts you need—no fluff, no jargon, just what works.
A naloxone readiness plan saves lives by ensuring quick access to overdose-reversing medication for anyone on opioids. Learn how to store, use, and distribute naloxone effectively-with real-world data and step-by-step guidance.
read more© 2026. All rights reserved.
