Phenytoin and Generics: What You Need to Know About Therapeutic Drug Monitoring
Dec 1 2025 - Health and Pharmaceuticals
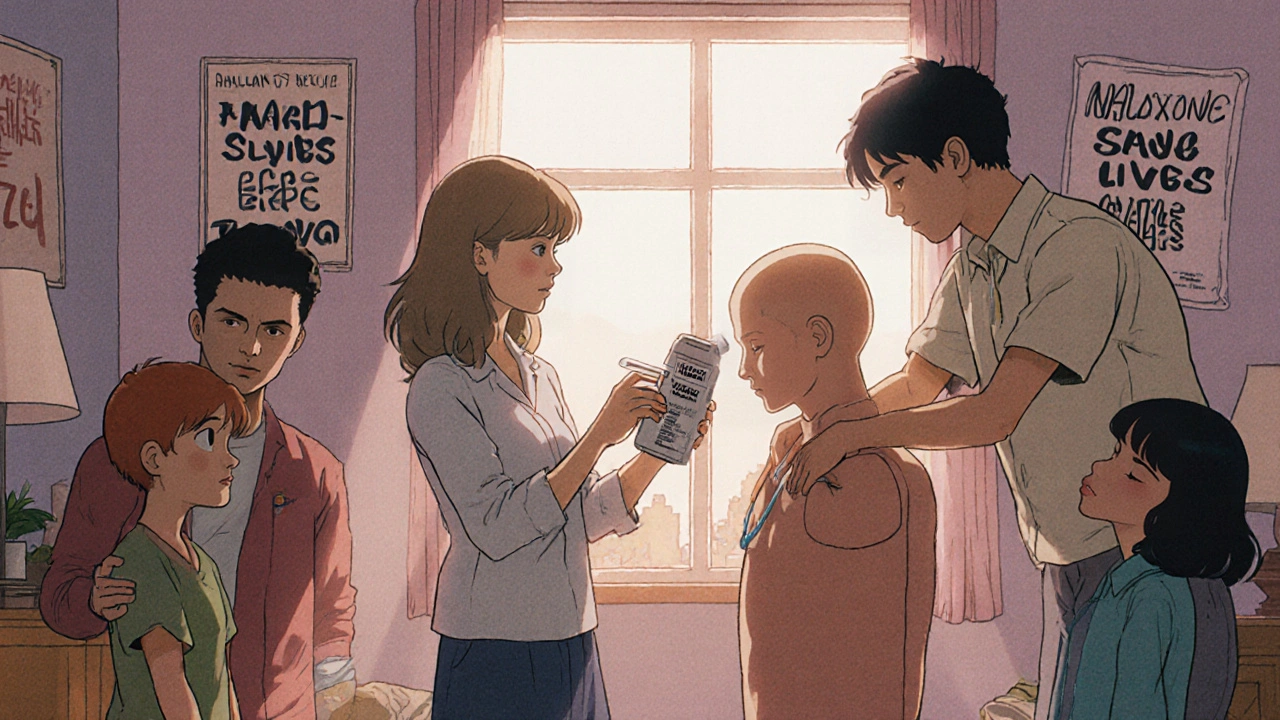
When someone overdoses on opioids, every second counts. naloxone, a fast-acting medication that blocks opioid effects in the brain. Also known as Narcan, it’s not a cure—it’s a rescue. For patients taking opioids for pain, or for those with opioid use disorder, naloxone is the difference between life and death. It doesn’t get you high. It doesn’t treat addiction. It simply flips the switch back on when breathing has stopped.
Naloxone for patients isn’t just for hospitals. It’s for families, friends, and people who use drugs. Many states now let anyone buy it without a prescription at pharmacies. It comes in nasal sprays and injectable forms, both easy to use—even without medical training. The opioid overdose, a sudden loss of breathing due to too much opioid in the system doesn’t care if you’re a teen, a veteran, or a grandparent. It happens fast, and naloxone works fast—usually within 2 to 5 minutes.
But naloxone isn’t foolproof. It only lasts 30 to 90 minutes. Opioids like fentanyl can stay in the body much longer, which means someone can stop breathing again after the first dose wears off. That’s why calling 911 is non-negotiable—even if the person wakes up. Also, multiple doses may be needed. Fentanyl is so strong that some overdoses require two or three sprays. And while naloxone reverses the overdose, it doesn’t remove the drug from the body. Withdrawal can hit hard: nausea, shaking, panic. That’s why follow-up care matters.
Patients on long-term opioid therapy, like those with chronic pain or opioid use disorder, should always have naloxone on hand. So should their caregivers. Studies show that when naloxone is distributed to people who use opioids, overdose deaths drop. It’s not about enabling—it’s about survival. The CDC and WHO both recommend making naloxone widely available. In fact, some clinics now give it out with every opioid prescription, like a seatbelt for your lungs.
There’s also a growing movement to train people in schools, shelters, and even grocery stores. You don’t need to be a doctor to save a life. If you see someone unresponsive, not breathing, or turning blue, give naloxone. Then call for help. It’s that simple. And it’s legal in every state.
What you’ll find in this collection are real, practical guides on how naloxone fits into patient care. From how to store it in your medicine cabinet, to what to do after giving a dose, to how it interacts with other medications like benzodiazepines. You’ll also see how it’s used in emergency rooms, in prisons, and in homes where someone is recovering from addiction. These aren’t theory pieces—they’re field reports from patients, nurses, and families who’ve been there.
A naloxone readiness plan saves lives by ensuring quick access to overdose-reversing medication for anyone on opioids. Learn how to store, use, and distribute naloxone effectively-with real-world data and step-by-step guidance.
read more© 2026. All rights reserved.
