Most people don’t talk about hemorrhoids-until they have them. Then it’s all you can think about. The itching, the pain, the embarrassment, the fear that maybe it’s something worse. The truth? Hemorrhoids are incredibly common. About 75% of people will deal with them at some point in their lives. And while they’re not dangerous, they can make daily life miserable. The key to feeling better fast is knowing whether you’re dealing with internal or external hemorrhoids-and what treatments actually work for each.
What Are Hemorrhoids, Really?
Hemorrhoids aren’t some weird abnormality. They’re normal blood vessels in your rectum and anus that help with stool control. Think of them like tiny cushions. But when pressure builds up-from straining during bowel movements, pregnancy, sitting too long, or chronic constipation-those cushions swell. That’s when they become a problem. There are two main types, and they’re not just different in location-they’re different in how they feel, what they do, and how you treat them. The big divider? The dentate line. That’s a natural boundary inside your anus. Above it? Internal hemorrhoids. Below it? External hemorrhoids. And that one line makes all the difference.Internal Hemorrhoids: Silent but Not Ignorable
Internal hemorrhoids sit inside the rectum, covered by tissue that doesn’t have pain nerves. That’s why they’re often painless. But don’t let that fool you. They can still cause serious issues. The most common sign? Bright red blood. You might see it on the toilet paper after wiping, in the toilet bowl, or streaked on your stool. It’s usually not mixed in with the stool-it’s separate, fresh, and alarming if you’ve never seen it before. You might also feel like you haven’t fully emptied your bowels, even after going. Or you might feel a sense of fullness or pressure deep inside. These symptoms often get worse with straining or after long periods of sitting. Internal hemorrhoids are graded from I to IV:- Grade I: Bleeds but doesn’t prolapse (protrude).
- Grade II: Prolapses when you strain, but pops back in on its own.
- Grade III: Prolapses and stays out-you have to push it back in.
- Grade IV: Stays out permanently and can’t be pushed back. This one can get very uncomfortable and may need surgery.
External Hemorrhoids: The Painful Ones
External hemorrhoids form under the skin around your anus. This area is packed with nerves. So when they swell, you feel it-badly. Symptoms include:- Painful lumps you can see or feel near your anus
- Itching or irritation
- Swelling and discomfort when sitting
- Sharp pain during bowel movements

What’s Not a Hemorrhoid? (And Why It Matters)
Not every bit of rectal bleeding or anal pain is a hemorrhoid. Mistaking something else for hemorrhoids can delay real treatment. An anal fissure-a small tear in the lining of the anus-can look similar. But instead of the dull ache or itching of hemorrhoids, fissures cause a sharp, tearing pain during bowel movements. You might also see a small crack in the skin. Fissures don’t usually cause lumps or swelling. Even scarier? Rectal bleeding can be a sign of something more serious: colorectal cancer, inflammatory bowel disease, or infections. That’s why if you’re over 50, have a family history of colon cancer, or notice changes in your bowel habits-like ongoing diarrhea, constipation, or weight loss-you need to see a doctor. Don’t assume it’s just hemorrhoids.Treatment: What Actually Works
The good news? Most hemorrhoids get better with simple, low-tech fixes. You don’t need surgery right away.For Mild Cases: Lifestyle First
This is step one for everyone, no matter the type:- Eat more fiber. Aim for 25-30 grams daily. Think beans, lentils, oats, broccoli, apples, and whole grains. Fiber softens stool so you don’t have to strain.
- Drink water. At least 8-10 glasses a day. Fiber without water makes things worse.
- Don’t sit on the toilet for more than 5 minutes. Reading or scrolling just increases pressure. Use a small footstool to raise your knees above your hips. That position reduces rectal pressure by about 30%.
- Move more. Walking, stretching, light exercise helps keep things moving and reduces pressure.
Over-the-Counter Relief
These help manage symptoms while your body heals:- Witch hazel pads: Soothe itching and swelling. Apply after bowel movements.
- Hydrocortisone cream (1%): Reduces inflammation and itching. Don’t use for more than a week without checking with a doctor.
- Sitz baths: Sit in warm (not hot) water for 15-20 minutes, 2-3 times a day. It relaxes the area, reduces swelling, and cleans gently.
For Internal Hemorrhoids: Minimally Invasive Procedures
If lifestyle changes don’t cut it, and you’re Grade I-III, doctors have options:- Rubber band ligation: A tiny band is placed around the base of the hemorrhoid. It cuts off blood flow. The hemorrhoid shrinks and falls off in a few days. It’s about 90% effective. You might feel pressure or mild cramping for a day or two.
- Sclerotherapy: A chemical solution is injected into the hemorrhoid. It causes scarring and shrinkage. Less painful than banding, but slightly less effective.
- Infrared coagulation: Heat is applied to the hemorrhoid to shrink it. Often used for smaller, bleeding ones.
For Thrombosed External Hemorrhoids: Quick Relief
If you’ve got a painful purple lump that came on suddenly, see a doctor within 72 hours. The best treatment? A small cut to remove the clot. It’s done in the office under local anesthetic. Pain drops dramatically within hours. Waiting too long means the clot hardens, and you’ll just have to wait it out-which can take weeks.Surgery: When It’s Necessary
For Grade IV internal hemorrhoids, recurrent cases, or severe external hemorrhoids that won’t heal:- Hemorrhoidectomy: The hemorrhoid is surgically removed. It’s the most effective option-95% success rate. But recovery takes 2-4 weeks. Pain is significant at first, and you’ll need prescription pain meds.
- Stapled hemorrhoidopexy: Used mainly for prolapsed hemorrhoids. The surgeon staples the tissue back into place and cuts off blood flow. Less pain than traditional surgery, but higher chance of recurrence.
What Doesn’t Work (And Why to Avoid It)
There’s a whole industry selling “miracle cures” online: creams that promise instant relief, herbal pills that “cure hemorrhoids in 3 days,” or devices that “vacuum them away.” None of these are backed by science. The American Gastroenterological Association and the American Society of Colon and Rectal Surgeons both warn against them. They don’t fix the root cause-pressure on the veins. And they can delay real treatment. Also, don’t rely on old advice like “eat more spicy food” or “don’t sit on cold surfaces.” These myths don’t help. Stick to what’s proven: fiber, water, movement, and medical care when needed.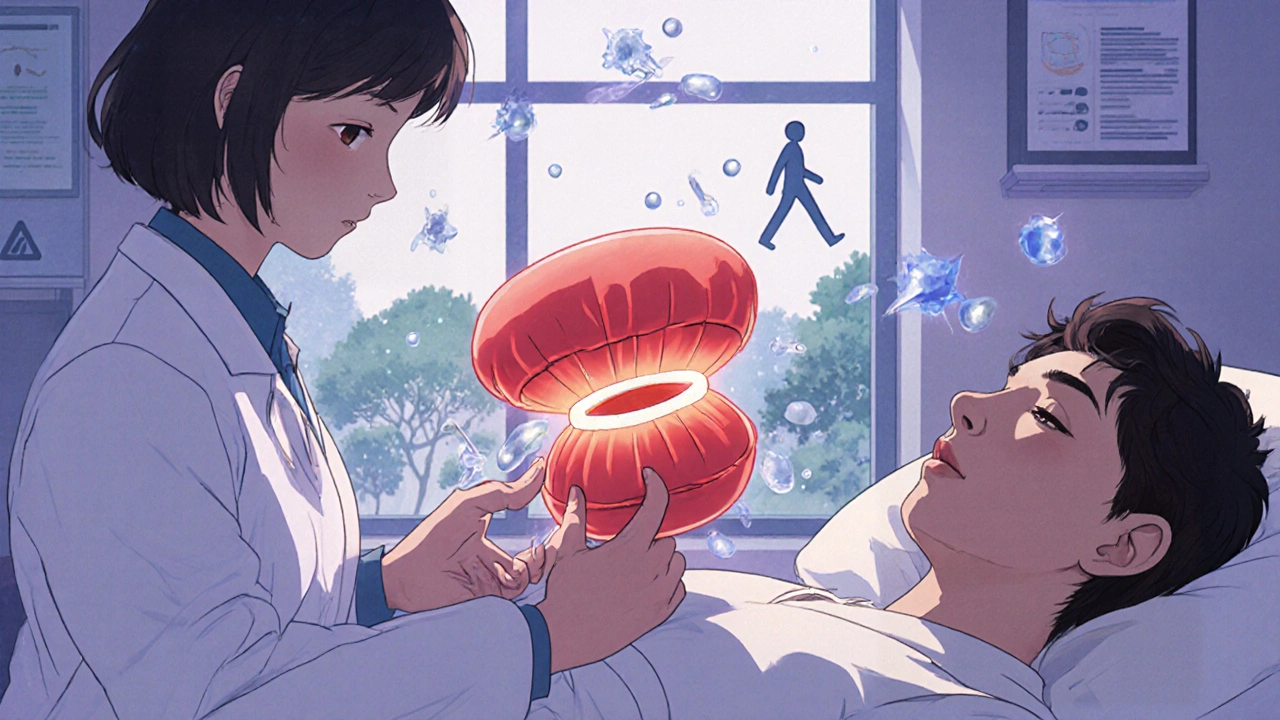
When to See a Doctor
You don’t need to suffer in silence. Call a doctor if:- Pain is severe or doesn’t improve after a week of home care
- Bleeding is heavy or keeps coming back
- You feel dizzy, weak, or lightheaded-signs of significant blood loss
- You notice changes in bowel habits: new constipation, diarrhea, or narrow stools
- You’re over 50 and haven’t had a colon cancer screening
Prevention: Stop the Cycle
The best treatment is avoiding them in the first place. Here’s what works:- Maintain high fiber intake daily-even after symptoms go away.
- Stay hydrated. Dehydration is a silent trigger.
- Don’t delay bowel movements. Holding it in increases pressure.
- Exercise regularly. Even a daily 20-minute walk helps.
- For pregnant women: pelvic floor exercises and sleeping on your left side reduce pressure on pelvic veins. Up to 35% of pregnant people get hemorrhoids, but many can prevent them with these steps.
Final Thought: It’s Manageable
Hemorrhoids are not a life sentence. They’re not a sign of weakness or poor hygiene. They’re a common, treatable condition caused by physical pressure. With the right info and a few simple changes, most people get relief without surgery. The key is knowing the difference between internal and external, recognizing when it’s time to see a doctor, and avoiding the scams that promise quick fixes. Your body is trying to tell you something. Listen to it. Take care of it. And don’t let embarrassment stop you from getting the help you need.Can internal hemorrhoids turn into external ones?
No, internal and external hemorrhoids are separate based on their location relative to the dentate line. However, an internal hemorrhoid can prolapse-meaning it pushes out through the anus-and become visible and irritated outside the body. It’s still an internal hemorrhoid that’s prolapsed, not a new external one. But you can have both types at the same time.
Do hemorrhoids go away on their own?
Mild hemorrhoids often shrink and improve within a few days to a week with home care: fiber, water, sitz baths, and avoiding straining. But they rarely disappear completely unless the root cause-like chronic constipation or prolonged sitting-is fixed. Without lifestyle changes, they tend to come back.
Is it safe to pop a thrombosed hemorrhoid myself?
Never try to pop or cut a thrombosed hemorrhoid yourself. That can lead to serious infection, uncontrolled bleeding, or scarring. If you have a painful purple lump, see a doctor within 72 hours. They can safely drain it in the office with a tiny incision and local anesthetic. The relief is immediate and the risk is minimal.
Can hemorrhoids cause cancer?
No, hemorrhoids do not cause cancer. But rectal bleeding-a common symptom of hemorrhoids-is also a symptom of colorectal cancer. That’s why any new or persistent bleeding, especially after age 50, should be checked by a doctor. Never assume bleeding is just hemorrhoids without ruling out other causes.
Will hemorrhoids affect my sex life?
External hemorrhoids, especially if swollen or thrombosed, can make sitting, walking, or sexual activity uncomfortable. Internal hemorrhoids usually don’t interfere unless they’re prolapsed and irritated. Once treated, most people return to normal activity without issue. If discomfort persists after treatment, talk to your doctor-there may be another underlying cause.
Are hemorrhoids more common in men or women?
Hemorrhoids affect men and women equally overall. But women are more likely to develop them during pregnancy due to increased pressure on pelvic veins from the growing uterus. Up to 35% of pregnant women experience hemorrhoids, especially in the third trimester. They often improve after delivery, but not always.
How long does recovery take after hemorrhoid surgery?
Recovery after a traditional hemorrhoidectomy usually takes 2 to 4 weeks. Pain is most intense in the first 7-10 days, and you’ll need prescription pain medication. Most people can return to light work after a week, but avoid heavy lifting or strenuous activity for 4 weeks. Stapled hemorrhoidopexy has a shorter recovery-about 1-2 weeks-but has a higher chance of recurrence.
Can stress cause hemorrhoids?
Stress doesn’t directly cause hemorrhoids, but it can contribute indirectly. High stress often leads to poor diet, less water intake, irregular bowel habits, and increased straining-all of which raise pressure on rectal veins. Stress can also worsen constipation or diarrhea, making hemorrhoids more likely to flare up.




Latrisha M. - 15 November 2025
Just want to say this is one of the clearest, most practical guides I’ve read on hemorrhoids. Fiber and water really are the foundation-no magic creams needed. I’ve seen people waste hundreds on ‘miracle’ ointments while ignoring the basics. Simple changes work if you stick with them.
Jamie Watts - 16 November 2025
LMAO so many people think sitting on cold floors causes hemorrhoids like its 1950 and we still believe in miasma theory. Bro its pressure from straining and sitting too long not your toilet seat. Also stop eating spicy food thinking it helps its just makes it burn worse. I know because I used to be one of those guys
Deepak Mishra - 17 November 2025
OMG I JUST HAD A THROMBOSIS LAST WEEK!!! IT WAS LIKE A PUNCH TO THE BUTT!!! I TRIED TO POP IT WITH A NEEDLE!!! 😱😭 DON’T DO THAT!!! I WENT TO THE DOCTOR AND THEY JUST SLIT IT OPEN AND IT WAS LIKE A WEIGHT WAS LIFTED OFF MY BODY!!! 🙏🔥
Diane Tomaszewski - 17 November 2025
I used to think this was just something that happened to older people or people who ate too much junk. Turns out I got them after my second kid and months of bad sleep and skipping meals. The sitz baths were the only thing that made me feel human again. Not glamorous but it works.
David Rooksby - 18 November 2025
Here’s the thing nobody tells you about hemorrhoids and the medical industrial complex-they make money off your discomfort. They push surgery because it’s profitable. Rubber band ligation? Sure it works. But did you know most Grade II cases resolve with just a high-fiber diet and squatting posture? The system wants you to think you need a procedure when you just need to stop sitting like a statue all day. Also the dentate line? That’s the body’s natural firewall. Respect it. Don’t ignore it. Don’t treat it like a glitch in the matrix.
Daniel Stewart - 19 November 2025
It’s funny how we’ll talk about depression or anxiety for hours but the moment someone says ‘hemorrhoids’ the room goes silent. Like it’s some sacred taboo. But here’s the truth-it’s a bodily function issue. We all poop. We all strain. We all sit. And when the body rebels? We panic. But it’s not a moral failure. It’s biology. And the fact that we’re still pretending it doesn’t exist is what makes it worse.
Dan Angles - 20 November 2025
Thank you for the comprehensive and clinically accurate overview. I would like to add that while lifestyle modifications are foundational, the role of pelvic floor physical therapy is underappreciated. Many patients with recurrent hemorrhoids have underlying pelvic floor dyssynergia. Addressing this can reduce recurrence by up to 60%. Consult a qualified PT if symptoms persist despite dietary changes.
John Mwalwala - 21 November 2025
Did you know the government doesn’t want you to know that hemorrhoids are caused by 5G radiation and fluoride in the water? They’re suppressing the truth because Big Pharma profits from surgeries. I’ve seen videos where people use magnets and essential oils and boom-gone. But the FDA won’t let you see them. Also I read somewhere that the dentate line is actually a secret portal to another dimension. That’s why it’s called ‘dentate’-it’s not teeth, it’s dimensional teeth. Don’t let them fool you.
Melanie Taylor - 21 November 2025
My mom had hemorrhoids after having me and she swore by witch hazel pads and coconut oil. She’d say ‘honey, your body’s just trying to tell you to chill out.’ I laughed at the time. Now I’m 32, pregnant, and I use them every day. She was right. Also-yes, it’s okay to cry while sitting in a warm bath. Nobody’s judging. 😊