Steroid Injection Safety Calculator
This tool helps you understand your risk level for systemic side effects and long-term joint damage based on your injection history and health conditions. Remember: steroid injections can help, but they should not be the first or only answer for joint pain.
Personal Information
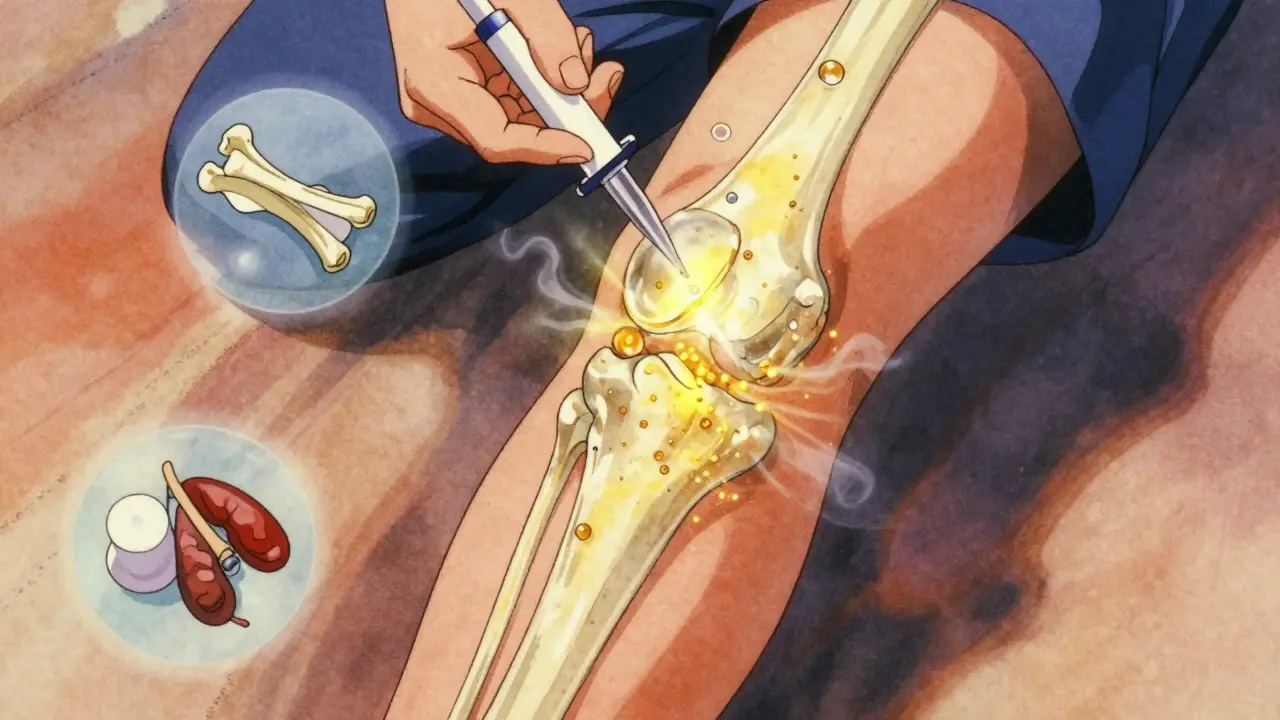
When you’ve got a knee or hip that aches with every step, an intra-articular steroid injection can feel like a lifeline. It’s quick, it’s common, and for many, it brings relief within days. But here’s something most people don’t know: those shots aren’t just staying in the joint. They’re leaking into your bloodstream-and that’s where things get complicated.
How These Injections Really Work
Intra-articular corticosteroid injections (IACS) have been used since the 1950s. Back then, Dr. Philip S. Hench won a Nobel Prize for proving cortisone could calm inflammation. Today, doctors still use that same principle: inject a powerful anti-inflammatory directly into a swollen joint to shut down pain signals. Common steroids used include triamcinolone acetonide, methylprednisolone acetate, and betamethasone. Doses range from 10 to 80 mg, depending on whether it’s a finger joint or a hip. The idea is simple: local treatment, minimal side effects. But that’s not what’s happening in real life. A 2023 study in Radiology found that even when injected into a joint, these steroids don’t stay put. Up to 40% of the dose can enter the bloodstream. That’s not a tiny leak-it’s enough to trigger systemic effects, especially if you’re getting multiple shots over time.The Hidden Risks: More Than Just a Flare-Up
Most patients know about the short-term risks: a temporary spike in pain (called a steroid flare), redness, or swelling at the injection site. But the real concerns are the ones that show up months-or years-later.- Accelerated joint damage: A study tracking 1,000 patients found that 1% developed rapid joint destruction after injections. That means cartilage wearing down faster, bone surfaces grinding together, and in some cases, the joint breaking down so badly that replacement surgery becomes unavoidable.
- Subchondral fractures: These are tiny cracks in the bone just under the cartilage. They don’t show up on regular X-rays until it’s too late. They’re linked to repeated steroid exposure.
- Osteonecrosis: Bone tissue dies because blood flow is cut off. This isn’t rare-it’s been documented after hip and knee steroid shots, especially in people with diabetes or those on high doses.
- Radiographic progression: Patients who got knee injections had 3.2 times higher odds of joint space narrowing on X-rays. For those who got multiple injections, the odds jumped to 4.67. That’s not just inflammation-it’s structural damage.
- High blood sugar-especially dangerous for diabetics. One study showed glucose levels spiked within hours and stayed elevated for days.
- Adrenal suppression: Your body stops making its own cortisol because the injection tricks your brain into thinking it’s got enough. This can lead to fatigue, dizziness, and even life-threatening crashes during illness or stress.
- Fluid retention and high blood pressure: Common in people getting repeated shots.
- Osteoporosis: Steroids leach calcium from bones. Postmenopausal women are at highest risk.
- Facial flushing, mood swings, and even Cushing’s syndrome with chronic use.
Who’s Most at Risk?
Not everyone gets hurt. But some people are walking into a minefield without knowing it.- People with early-stage osteoarthritis: If your X-ray shows only mild wear and tear but you’re in a lot of pain, the problem might not be the joint itself. It could be inflammation from another source. Steroids won’t fix that-and they might make the joint worse.
- Diabetics: Even one injection can send blood sugar through the roof. Some need to adjust insulin for a week after the shot.
- Postmenopausal women: Bone density drops faster under steroid exposure. One injection might not do much. Three a year? That’s a problem.
- People planning surgery: If you’re thinking about a joint replacement in the next 6-12 months, steroids can delay healing and increase infection risk.
- Those already on oral steroids: Every injection adds to your total steroid burden. Doctors often forget to count them.

The Controversy: Why Do Doctors Still Recommend Them?
This is where it gets messy. On one side, you’ve got solid research showing harm. On the other, you’ve got decades of clinical practice saying these shots are safe. The American Academy of Orthopaedic Surgeons still conditionally recommends corticosteroid injections for knee osteoarthritis. The American Family Physician says benefits outweigh risks. But here’s the catch: most of those studies only looked at short-term pain relief. None tracked joint structure over 5+ years. Dr. Ali Guermazi, lead author of the 2023 Radiology study, put it bluntly: “We’ve been telling patients that even if these injections don’t relieve your pain, they’re not going to hurt you. But now we suspect that this is not necessarily the case.” Meanwhile, other studies-like one by Dr. Raynauld-found no change in joint space narrowing. So what’s going on? The answer might be in the details:- Some studies use different steroids. Triamcinolone acetonide has higher systemic absorption than others.
- Dosing varies. A 40 mg shot in the knee isn’t the same as an 80 mg shot in the hip.
- Imaging methods differ. MRI picks up cartilage loss early. X-rays don’t.
- Follow-up time matters. Harm shows up after 1-2 years, but many trials only look at 3-6 months.
What Are the Current Limits?
Most guidelines say: no more than 3-4 injections per joint per year. But that’s a guess. There’s no hard science behind that number. The Joint Rehabilitation Center’s 2023 analysis suggests we need personalized limits:- For a 70-year-old with advanced osteoarthritis and no other health issues: 2-3 shots a year might still be reasonable.
- For a 55-year-old with mild osteoarthritis and type 2 diabetes: Even one shot might be too much.
- For someone with osteoporosis or a history of fractures: Avoid them altogether.

What Else Can You Do?
Steroid shots aren’t the only option. And for many, they’re not even the best one.- Physical therapy: Stronger muscles around the joint reduce stress. Studies show PT is just as effective as steroids for knee pain-and it lasts longer.
- Weight loss: Losing 10 pounds reduces knee pressure by 40 pounds per step. That’s more effective than any injection.
- Bracing or orthotics: Especially helpful for knee osteoarthritis. They shift load away from the damaged part of the joint.
- Platelet-rich plasma (PRP) or hyaluronic acid: These are newer options. PRP may help rebuild tissue. Hyaluronic acid lubricates. Neither has the same systemic risks as steroids.
- Exercise: Walking, swimming, cycling. Low-impact movement keeps joints healthy and reduces inflammation naturally.
The Bottom Line
Intra-articular steroid injections aren’t evil. They’re a tool. But like any tool, they can be misused. If you’re considering one:- Ask your doctor: “What’s the goal? Is this for short-term relief or long-term joint protection?”
- Ask: “Have you checked my bone density? My blood sugar? My recent X-rays?”
- Ask: “What happens if I don’t get this shot?”
- Ask: “Is there a safer alternative?”
There’s no magic fix for joint pain. But there are smarter ways to manage it. Steroid injections can help-but they shouldn’t be the first, or the only, answer.
Can intra-articular steroid injections cause long-term joint damage?
Yes. Multiple studies, including a 2023 study in Radiology, show that repeated corticosteroid injections can accelerate cartilage loss, cause subchondral fractures, and lead to rapid joint destruction. Patients with mild osteoarthritis are at higher risk because their joints are still repairable-and steroids can interfere with that process.
Do steroid shots affect blood sugar?
Absolutely. Even a single injection can raise blood glucose levels for several days. Diabetics often need to adjust insulin or oral medications after a shot. Monitoring glucose for 3-7 days post-injection is strongly recommended.
How many steroid injections are safe per year?
Most guidelines recommend no more than 3-4 injections per joint per year. But this isn’t based on solid evidence. For people with diabetes, osteoporosis, or early osteoarthritis, even 1-2 shots a year may carry too much risk. Individual risk assessment is essential.
Are there alternatives to steroid injections for joint pain?
Yes. Physical therapy, weight loss, low-impact exercise, bracing, hyaluronic acid injections, and platelet-rich plasma (PRP) are all alternatives with fewer systemic risks. For many patients, especially those with mild to moderate osteoarthritis, these options provide longer-lasting relief without damaging the joint.
Can steroid injections cause adrenal suppression?
Yes. Corticosteroids suppress the body’s natural cortisol production. This can happen even with local injections, especially with frequent use. Symptoms include fatigue, dizziness, nausea, and low blood pressure. In rare cases, it can lead to adrenal crisis during illness or stress. Patients on multiple injections should be monitored.
Why do some doctors still say steroid injections are safe?
Many older studies focused only on short-term pain relief, not long-term joint structure. Guidelines from organizations like the American Academy of Orthopaedic Surgeons still recommend injections because they work quickly. But newer research shows that short-term relief doesn’t equal long-term safety. The medical community is slowly shifting toward a more cautious approach.
What should I do if I’ve had multiple steroid shots?
Schedule a follow-up with your doctor. Ask for a new X-ray or MRI to check for joint damage. Get your blood sugar and bone density tested if you haven’t recently. Consider switching to non-steroid treatments like physical therapy or weight management. If you’ve had more than 3 injections in a year for the same joint, it’s time to change your strategy.

Tracy Howard - 20 January 2026
Oh, sweet mercy-another ‘medical miracle’ turned slow-motion car crash. I’ve seen this in Toronto clinics: grandmas getting three knee shots a year like they’re getting free lattes, then showing up six months later with a joint that looks like a crumbled cookie. And the doctors? Smiling, billing, and pretending they didn’t just hand out nuclear waste in a syringe. This isn’t medicine-it’s institutionalized negligence wrapped in a white coat.
Jake Rudin - 21 January 2026
It’s not merely a question of dosage-or even systemic absorption-it’s a metaphysical betrayal of the body’s autonomy. The injection, intended as a localized intervention, becomes a Trojan horse of endocrine disruption, silently overriding the hypothalamic-pituitary-adrenal axis, which, in its evolved wisdom, was never designed to be coerced by exogenous glucocorticoids. We mistake symptom suppression for healing-and in doing so, we colonize our own physiology with the illusion of control.
Lydia H. - 21 January 2026
I’ve had two of these shots in my hip over the past year. Felt amazing at first. Then, my blood sugar went nuts for weeks, and I started feeling like a zombie after 3 p.m. I didn’t connect the dots until I read this. Now I’m doing PT three times a week, lost 12 pounds, and my pain’s actually better. No more shots. Honestly? I wish someone had told me this before I signed the consent form.
Aman Kumar - 23 January 2026
Let me elucidate the pathological cascade: corticosteroids induce upregulation of matrix metalloproteinases (MMPs), particularly MMP-13, which degrades type II collagen-the primary structural component of articular cartilage. Concurrently, they suppress chondrocyte proliferation and glycosaminoglycan synthesis, thereby accelerating degenerative arthropathy. The 3.2x radiographic progression metric is not merely correlational-it is mechanistically deterministic. To recommend these injections without MRI surveillance is not clinical practice-it is malpractice.
Astha Jain - 23 January 2026
so like... i got 3 shots last year and now my bones feel kinda... crumbly? like my hip just kinda sighs when i stand up? and my sugar’s been wild. i thought it was just aging. guess not. thx for the heads up lol
Phil Hillson - 24 January 2026
OMG this is why I hate doctors they just wanna keep you coming back for more shots so they get paid and nobody cares that you’re slowly turning into a walking steroid zombie with osteoporosis and diabetes and no joy in life just pain meds and a cane
Valerie DeLoach - 25 January 2026
To anyone reading this: if you’re considering an injection, please ask your provider to sit with you for 15 minutes-not to sell you the procedure, but to listen. Ask what they’d do if it were their parent, their sibling, their child. The answer might surprise you. And if they don’t pause? Walk out. Your body isn’t a vending machine. It’s a living, breathing system that deserves respect, not quick fixes.
Christi Steinbeck - 26 January 2026
YOU ARE NOT ALONE. I was skeptical about PT, but after 6 weeks of working with my physical therapist, my pain dropped 70%. I didn’t need the shot. I didn’t need the risk. I just needed to move better. If you’re reading this and you’re scared to stop the shots-start with a 10-minute walk today. Your future self will thank you. You’ve got this.
Jacob Hill - 27 January 2026
I appreciate this post so much. I’ve been getting injections for my knee for 4 years-3 a year. I never thought about how they might be making things worse. I just wanted the pain to go away. Now I’m scheduling an MRI and a bone density scan. I’m also starting a walking program. Thank you for giving me the courage to question what I’ve been told.
Lewis Yeaple - 29 January 2026
It is imperative to note that the pharmacokinetics of triamcinolone acetonide exhibit a significantly higher systemic bioavailability compared to methylprednisolone acetate, as demonstrated in comparative plasma concentration studies. Consequently, the recommendation to limit injections to three per annum is not evidence-based but rather consensus-derived. The absence of longitudinal, randomized controlled trials with structural endpoints renders current guidelines speculative at best.
Jackson Doughart - 30 January 2026
I’ve been a physical therapist for 18 years. I’ve seen patients come in after their third steroid shot, their joint already collapsing, and they’re furious because ‘the doctor said it was safe.’ I wish I could go back in time and hand every one of them this article. You don’t have to suffer. You don’t have to sacrifice your joint for a few months of relief. There’s a better way. It just takes patience.
Malikah Rajap - 1 February 2026
Wait, so... if I got a shot last month, and now I’ve been feeling super tired and my face is puffier? Is that... is that Cushing’s? Should I be scared? I’m not trying to panic, but I didn’t know this could happen from just one shot... I’m gonna call my doctor tomorrow.
sujit paul - 1 February 2026
These injections are not merely medical-they are part of a grand pharmaceutical orchestration to keep you dependent, docile, and monetizable. The FDA, the AAOS, the insurance companies-they all profit from your chronic pain. The truth? They don’t want you healed. They want you managed. Your joint is not broken. Your system is being manipulated. Wake up.