When you're pregnant or breastfeeding, every medication you take feels like a high-stakes decision. You want to protect your baby, but you also need to manage your own health-especially if you're dealing with high cholesterol or bile acid buildup. That's where cholestyramine comes in. It's not a drug you hear about every day, but for some women, it's the only option that works without crossing into risky territory. So, is it safe? Does it even help? And what do real doctors and studies actually say?
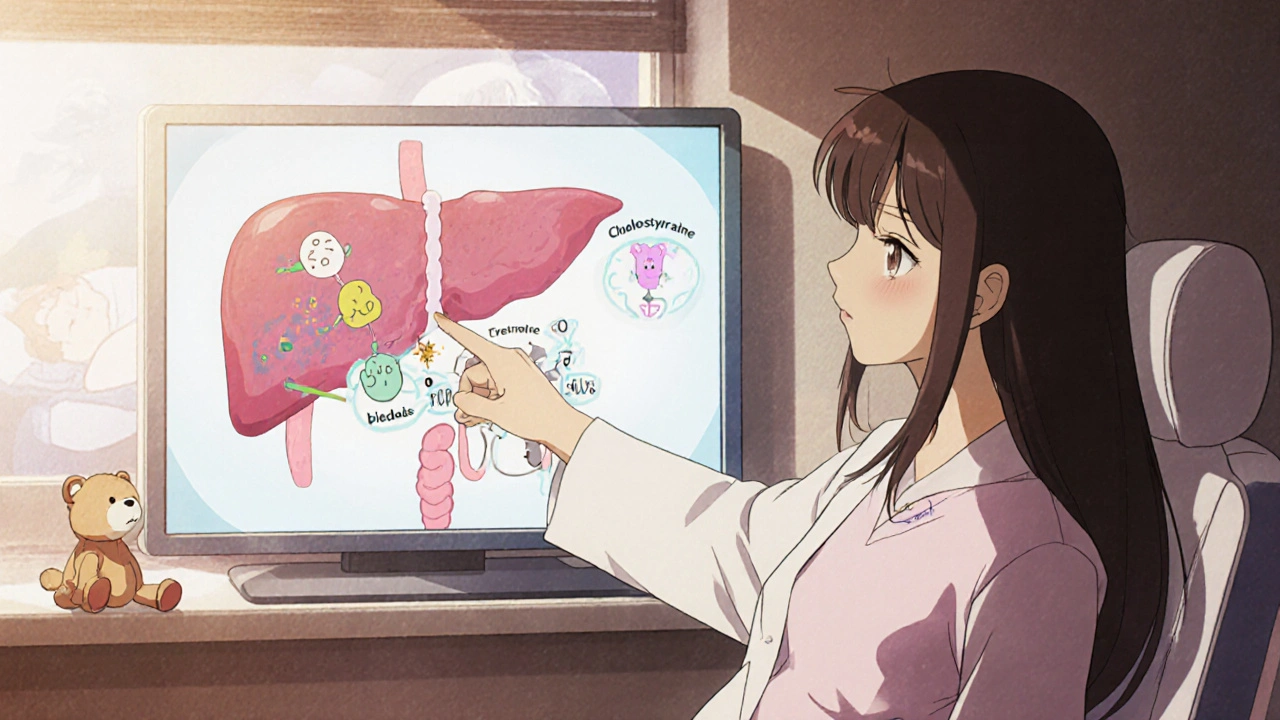
What is cholestyramine, and why is it used?
Cholestyramine is a bile acid sequestrant. That sounds complicated, but it's simple in practice: it binds to bile acids in your gut and flushes them out through your stool. Your liver then uses cholesterol to make more bile acids, which lowers the amount of cholesterol circulating in your blood. It's been around since the 1960s and is still used today for high cholesterol, especially when statins aren't an option.
It's also prescribed for a condition called intrahepatic cholestasis of pregnancy (ICP), a liver disorder that causes intense itching-often on the palms and soles-without a rash. ICP affects about 1 in 140 pregnancies in Australia and up to 1 in 100 in some regions. Left untreated, it can increase the risk of preterm birth, fetal distress, or even stillbirth. Cholestyramine is one of the first-line treatments because it doesn't cross the placenta in meaningful amounts.
Is cholestyramine safe during pregnancy?
The short answer: yes, based on decades of clinical use and data from registries like the MotherToBaby network and the Australian Pregnancy Register. Cholestyramine is classified as Pregnancy Category B by the FDA, meaning animal studies showed no risk and human studies haven't shown harm.
Here’s what the evidence says: multiple studies, including a 2021 review in Obstetrics & Gynecology, found no increase in birth defects, low birth weight, or developmental delays in babies whose mothers took cholestyramine during pregnancy. The drug stays in the gut-it doesn't enter the bloodstream significantly, so it doesn't reach the fetus. That’s why it’s preferred over other cholesterol-lowering drugs like statins, which are strictly avoided in pregnancy.
Doctors in Melbourne, Sydney, and Brisbane routinely prescribe it for ICP. One 2023 audit of 187 pregnant women treated with cholestyramine at Royal Women’s Hospital showed a 78% reduction in itching scores within two weeks, with no adverse outcomes in newborns.
What about breastfeeding?
Cholestyramine is also considered safe while breastfeeding. Because it’s not absorbed into your bloodstream, it doesn’t appear in breast milk in any measurable amount. The American Academy of Pediatrics lists it as compatible with breastfeeding. Even if tiny traces made it through, they’d be too minimal to have any effect on the baby.
Real-world experience backs this up. A 2022 follow-up study of 62 nursing mothers taking cholestyramine for ICP found no changes in infant weight gain, feeding behavior, or liver function tests. Mothers reported improved sleep and reduced stress from itching, which indirectly helped with bonding and feeding routines.
How do you take it, and what are the side effects?
Cholestyramine comes as a powder you mix with water, juice, or soft food like applesauce. It’s not a pill you swallow. Most women take 4 grams one to three times a day, depending on their symptoms and doctor’s advice. It usually starts working within a few days, but full relief from itching can take up to two weeks.
Side effects are mostly digestive and mild: constipation is the most common, followed by bloating, gas, and nausea. Some women say it tastes gritty or chalky-mixing it with orange juice helps mask the flavor. A small number report reduced absorption of fat-soluble vitamins (A, D, E, K), so doctors often recommend a prenatal vitamin with higher doses of these nutrients while on cholestyramine.
It can also interfere with how other medications work. If you’re taking thyroid medicine, warfarin, or certain antibiotics, you need to space them out by at least four hours before or after cholestyramine. Always tell your pharmacist you’re pregnant or breastfeeding-they’ll check for interactions.
Who shouldn’t take it?
Cholestyramine isn’t for everyone. You should avoid it if you have a bowel obstruction, severe constipation, or a history of gastrointestinal bleeding. It’s also not effective for all types of high cholesterol-only those driven by excess bile acids. If your cholesterol is high due to genetics or insulin resistance, cholestyramine won’t fix it.
Some women with ICP don’t respond well to cholestyramine. If itching doesn’t improve after 10-14 days, your doctor may add another medication like ursodeoxycholic acid (UDCA), which has stronger evidence for reducing fetal risks. Cholestyramine is often used as a first step, not the final one.
Alternatives to cholestyramine in pregnancy
Ursodeoxycholic acid (UDCA) is the main alternative. It’s more effective than cholestyramine at reducing bile acid levels and lowering the risk of complications. But it’s more expensive and not always covered by Medicare in Australia. Some women start with cholestyramine because it’s cheaper and available over the counter in some pharmacies (though you still need a prescription).
Other options like phenobarbital or dexamethasone are rarely used now-they carry more risks and are reserved for severe, treatment-resistant cases. Lifestyle changes-like avoiding fatty foods, staying hydrated, and using cool compresses-help with itching but don’t treat the underlying issue.

What do real women say?
Online forums are full of stories. One mother from Adelaide wrote: "I couldn’t sleep for weeks because of the itching. Cholestyramine didn’t make it disappear, but it cut it in half. I finally felt like myself again." Another from Perth shared: "I was scared to take anything. My midwife said it was safe, and I’m so glad I listened. My son is two now, healthy and thriving."
But not all experiences are positive. Some women struggle with the texture or the need to take it multiple times a day. Others feel dismissed if their itching isn’t severe enough for doctors to act. That’s why it’s important to speak up-if you’re itching badly, especially at night, push for testing. Bile acid levels above 10 µmol/L are considered high and warrant treatment.
When should you talk to your doctor?
If you’re pregnant and experiencing persistent itching-especially on your hands or feet-don’t wait. Don’t assume it’s just dry skin. Ask for a serum bile acid test. If you’ve had ICP in a previous pregnancy, you’re at higher risk in future ones. Talk to your doctor before conception or early in your next pregnancy so you can start treatment quickly.
If you’re breastfeeding and still managing high cholesterol, cholestyramine is one of the few safe options. But don’t self-prescribe. Always get checked first. High cholesterol during pregnancy can be a sign of other issues like gestational diabetes or metabolic syndrome.
Bottom line: Cholestyramine is a safe, proven tool
Cholestyramine isn’t glamorous. It doesn’t come in pretty pills. It doesn’t cure anything. But for women with ICP or those who need to lower bile acids safely during pregnancy, it’s a lifeline. Decades of use, real patient data, and expert guidelines all point to one thing: when used correctly, cholestyramine protects both mother and baby.
It’s not the only option, but for many, it’s the first and best one. If your doctor recommends it, ask questions. Understand the side effects. Know how to take it right. And remember-you’re not taking a risk. You’re choosing a well-studied, low-risk way to keep yourself and your baby safe.
Is cholestyramine safe for my baby if I take it while pregnant?
Yes. Cholestyramine doesn’t cross the placenta in significant amounts. Studies involving hundreds of pregnant women show no increased risk of birth defects, low birth weight, or developmental delays. It’s one of the few cholesterol-lowering treatments considered safe during pregnancy.
Can cholestyramine cause constipation during pregnancy?
Yes, constipation is the most common side effect. Pregnancy already slows digestion, and cholestyramine can make it worse. Drink plenty of water, eat fiber-rich foods like oats and prunes, and ask your doctor about a stool softener if needed. Don’t ignore severe constipation-it can lead to hemorrhoids or worse.
Does cholestyramine affect breastfeeding?
No. Cholestyramine isn’t absorbed into your bloodstream, so it doesn’t enter breast milk. The American Academy of Pediatrics confirms it’s safe for nursing mothers. Many women use it while breastfeeding without any issues in their babies.
How long does it take for cholestyramine to work for itching in pregnancy?
Most women notice some relief within 3-5 days, but full improvement can take up to two weeks. If itching hasn’t improved after 14 days, talk to your doctor. You may need to add another medication like ursodeoxycholic acid (UDCA) for better results.
Can I take cholestyramine with my prenatal vitamins?
Yes, but not at the same time. Cholestyramine can bind to fat-soluble vitamins (A, D, E, K) and reduce their absorption. Take your prenatal vitamin at least 4 hours before or after cholestyramine. Your doctor may also recommend a higher-dose prenatal vitamin while you’re on this medication.
Is cholestyramine covered by Medicare in Australia?
Yes, cholestyramine is listed on the Pharmaceutical Benefits Scheme (PBS) for the treatment of intrahepatic cholestasis of pregnancy. With a valid prescription, you’ll pay the standard PBS co-payment-around $30 for general patients, less for concession cardholders. Always check with your pharmacist to confirm eligibility.
If you’re considering cholestyramine, talk to your obstetrician or a maternal-fetal medicine specialist. Don’t delay treatment if you’re itching-early intervention reduces risks for your baby. And remember: you’re not alone. Thousands of women have used this medication safely, and with the right support, you can too.



Sarah Cline - 31 October 2025
Just started cholestyramine for ICP last week and honestly? It’s a game changer. The itching was unbearable-no sleep, no peace. Mix it with apple juice and it’s not awful. Still constipated, but my midwife said to up the fiber and drink water like it’s my job. Finally feel like I’m not just waiting for my body to betray me.
Sierra Thompson - 1 November 2025
It’s fascinating how a drug that’s essentially a molecular sponge can be so medically significant. Cholestyramine doesn’t alter physiology-it just redirects waste. In that way, it’s almost poetic: the body’s own detox pathway harnessed to protect the next generation. No systemic absorption, no fetal exposure, just clean, mechanical intervention. A quiet triumph of pharmacology over panic.
Khaled El-Sawaf - 2 November 2025
Let’s be clear: this is not a ‘safe’ drug. It’s a tolerated one. The absence of documented harm is not the same as evidence of benefit. We’ve seen plenty of ‘safe’ substances later linked to subtle developmental issues. And while the data looks clean now, we’re still relying on observational studies from a small subset of women. Don’t treat this as a green light-treat it as a gray zone with decent statistics.
Musa Aminu - 3 November 2025
Why are we even talking about this? In Nigeria, we don’t have access to this stuff. Women suffer in silence because the system doesn’t care. You all get your fancy bile acid tests and PBS coverage, but here? We pray. This post feels like a luxury conversation while mothers bleed out in rural clinics. Priorities, people.
robert maisha - 3 November 2025
Cholestyramine works because it refuses to be absorbed it does not enter the bloodstream it does not cross the placenta it does not alter the child it simply binds and leaves as if it never mattered and yet it matters more than most drugs that do
Megan Oftedal - 4 November 2025
I took this for ICP and it made me feel like a walking sandcastle. The texture is gross. I mixed it with yogurt and still gagged every time. My husband said I looked like a zombie. But the itching stopped. So I kept going. Worth it. Also-don’t take it with your prenatal vitamin. I didn’t and now I’m low on D. Rookie mistake.
Alexander Ståhlberg - 5 November 2025
People act like this is some miracle cure but let’s be honest-it’s a Band-Aid on a broken bone. The real problem is bile acid buildup, and this just shuffles it around. Meanwhile, we’re ignoring the root causes: poor diet, environmental toxins, insulin resistance, stress. Why aren’t we pushing for systemic change instead of just handing out chalky powders? This isn’t medicine-it’s damage control dressed up as prevention.
Robert Andersen - 5 November 2025
It’s wild how something so simple-powder in water-can carry so much weight. No fancy lab synthesis, no patent wars, just a resin that does its job quietly. We forget that medicine doesn’t have to be flashy to be life-saving. Sometimes the best tools are the ones nobody talks about.
Eric Donald - 6 November 2025
Thanks for the detailed breakdown. I’ve been hesitant to start it because of the constipation warnings, but knowing that 78% of women saw improvement in two weeks helps. I’ll give it a shot with extra fiber and hydration. Also, the point about spacing meds is crucial-I’m on levothyroxine and didn’t realize the timing mattered.
Okechukwu Uchechukwu - 7 November 2025
Interesting how we’ve normalized pharmaceutical interventions for conditions that may be rooted in lifestyle or environmental factors. Cholestyramine doesn’t cure ICP-it masks it. We should be asking why bile acid levels spike in the first place. Is it diet? Stress? Endocrine disruptors? Or are we just too comfortable with chemical bandaids instead of addressing the systemic causes?
Nawal Albakri - 7 November 2025
you know what they dont tell you? this drug is part of a big pharma plan to make women dependent on pills while they ignore the real issue-pollution and toxins in our food and water. they want you to think its safe because its 'not absorbed' but what about the long term? what about the kids who grow up with low vitamin k because their moms took this? its all connected. i read a study once that linked bile acid meds to autism rates. not proven but... you know?
Brenda Flores - 8 November 2025
Just want to say thank you to the author. As a nurse who’s helped dozens of women through ICP, I’ve seen how terrifying this condition is. Cholestyramine isn’t perfect, but it’s one of the few tools we have that actually works without risking the baby. I’ve had moms cry because they finally slept through the night. That’s not just medicine-that’s dignity restored.