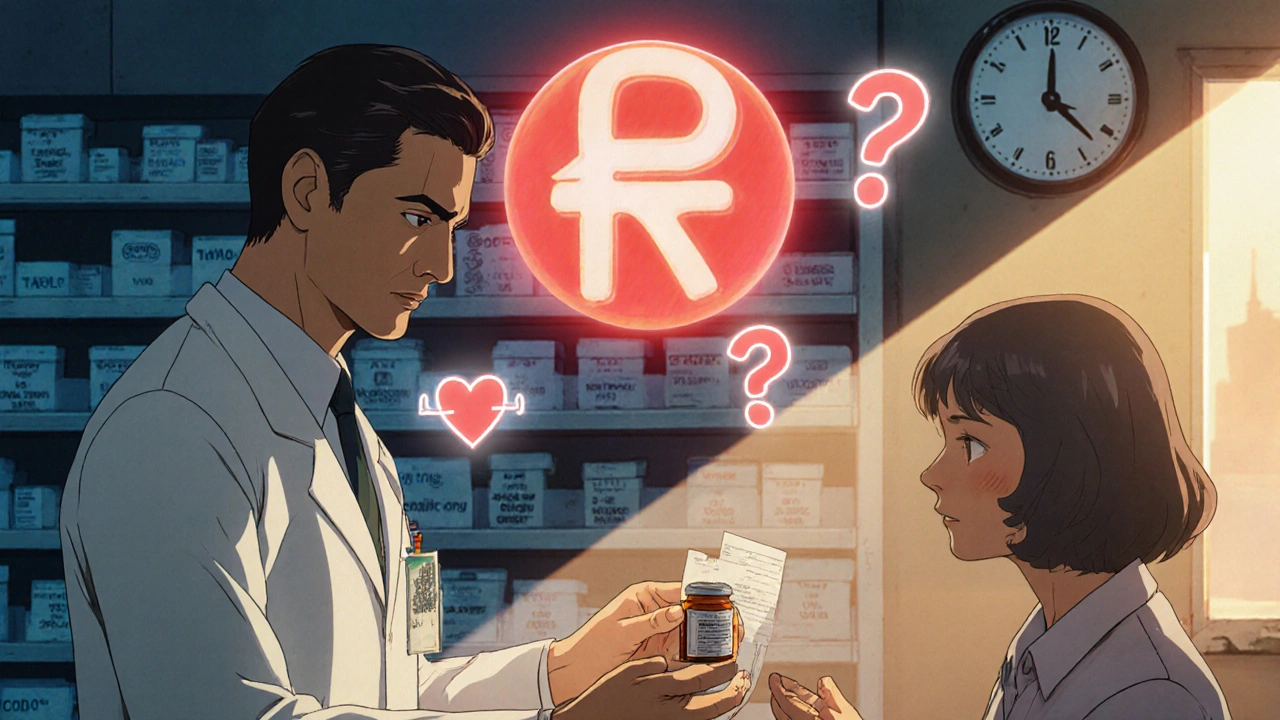
When your doctor writes a prescription for a brand-name medication, and the pharmacy hands you a different pill with a cheaper label, you might not think much of it. But behind that simple swap is a high-stakes battle between insurers pushing for cost cuts and providers trying to keep patients safe. This isn’t just about money-it’s about trust, time, and sometimes, life or death.
Why Insurers Push for Generics
Health insurers don’t mandate generic drugs because they dislike brand names. They do it because generics cost 80-85% less. That’s not a guess-it’s FDA data. In 2022, 90% of all prescriptions filled in the U.S. were for generics, but those generics made up only 18% of total drug spending. For insurers, that’s a massive savings. A $150 monthly brand-name drug can drop to $15 as a generic. Multiply that across millions of prescriptions, and you’re talking billions saved every year. But here’s the catch: those savings aren’t always passed on to patients. Instead, insurers use tiered formularies to make brand-name drugs financially unattractive. A generic might cost a $10 copay. The brand-name version? $75 or more. Some plans even require 40% coinsurance for brand drugs, meaning you pay almost half the price out of pocket. That’s not a nudge-it’s a shove. Insurers also use step therapy: you have to try-and fail-on the generic first before they’ll cover the brand. And prior authorization? That’s a paperwork maze. Providers must submit clinical notes, lab results, and sometimes even letters from patients explaining why the generic didn’t work. All of this is designed to make switching to generics the easiest path… for the insurer.How Providers Are Fighting Back
Doctors aren’t passive players in this game. They’re caught between an insurer’s rules and their duty to their patients. Many have adapted by becoming experts in the system-learning each insurer’s unique rules, building templates for appeals, and even hiring staff just to handle prior authorization. A 2023 MGMA survey found physicians spend an average of 16.9 minutes per prior authorization request. That’s nearly 13 hours a week for many practices. Some clinics now have dedicated prior authorization coordinators. In medium-sized practices, that role costs over $112,000 a year per person. It’s not efficiency-it’s damage control. Providers also document everything. A doctor in Minnesota told the AMA about a patient who needed a brand-name anticoagulant because the generic caused dangerous bleeding. The insurer denied coverage three times. It took 22 days and two emergency room visits before the patient got the right medication. Now, that doctor includes clinical evidence in every single prescription for brand-name drugs-lab values, prior adverse reactions, even patient letters. It’s not ideal. But it’s necessary. Some providers are using technology to cut through the noise. Electronic prior authorization (ePA) systems integrated into EHRs have cut approval times by 55%, according to a 2024 JAMIA study. But not all systems talk to each other. Insurers still use different standards, and many don’t clearly define what counts as “medical necessity.” One provider described it like trying to solve a puzzle with missing pieces.
State Laws Are Changing the Game
Not all states let insurers run unchecked. California’s AB 347, effective January 2024, forced a major shift. It requires insurers to respond to step therapy exceptions within 72 hours for urgent cases and 5 business days for standard ones. Approval rates jumped to 92% on first submission. A psychiatrist in Los Angeles said it went from a two-week nightmare to a 72-hour formality. Arizona took it further. In May 2025, HB 2175 banned insurers from denying coverage based solely on AI algorithms. Medical directors must now personally review denials. Implementation is required by June 30, 2026. That’s a direct response to cases where automated systems flagged a patient’s request as “low risk” and denied a needed medication-without ever reading a chart. These laws aren’t outliers. In 2024-2025, 34 states introduced bills to limit prior authorization abuse. The federal Improving Seniors’ Timely Access to Care Act, signed in late 2022, already requires Medicare Advantage plans to respond to urgent prior authorization requests within 72 hours. By 2027, CMS will require all Medicaid and Medicare Advantage plans to use standardized electronic systems. That could cut processing time by 40-60%.The Clinical Risks Nobody Wants to Talk About
Generics are safe-for most drugs. The FDA requires them to be bioequivalent within 80-125% of the brand-name version. But that range is wide. For drugs with a narrow therapeutic index-like levothyroxine, warfarin, or certain seizure medications-even small differences can cause harm. The AMA reports that 28% of physicians have seen adverse outcomes after switching patients to a different generic version of levothyroxine. Patients report fatigue, weight gain, or heart palpitations. When labs show TSH levels shifting, it’s often too late. One study found that switching thyroid meds led to a 30% increase in hospitalizations for arrhythmias. And it’s not just about chemistry. Patients lose trust. When a drug that worked for years suddenly stops working after a switch, they feel like their care was treated like a commodity. A Reddit post from a cardiologist in 2024 got over 140 upvotes when he wrote: “I now tell every patient, ‘If you’ve been on this brand for years and it works, don’t let them switch you. Fight it.’” Insurers claim 98.7% of substitutions go smoothly. But that 1.3%? That’s thousands of patients a year. And for those patients, it’s 100%.
What Providers Can Do Right Now
You don’t need to wait for new laws to protect your patients. Here’s what works today:- Use templates. 68% of physicians use pre-written letters for common exceptions. Save time and increase approval rates.
- Know your insurer’s rules. 89% of providers say each insurer has different criteria. Keep a cheat sheet: what’s required for UnitedHealthcare vs. Cigna vs. Blue Cross.
- Submit objective data. Lab results, prior treatment failures, documented allergies-these boost approval rates by 37%.
- Build relationships. Find the case manager at your insurer who actually answers the phone. A personal connection can cut through bureaucracy.
- Use ePA. If your EHR supports it, use electronic prior authorization. It’s faster, trackable, and reduces errors.
- Advocate. Tell your patients: “This isn’t about cost-it’s about your health. If you feel worse after a switch, call me immediately.”
The Bigger Picture
The pressure to use generics isn’t going away. UnitedHealthcare aims for 95% generic utilization by 2030. PBMs like CVS Caremark and OptumRx control 85% of prescriptions in the U.S. and are tightly linked to their parent insurers. They’re not just middlemen-they’re gatekeepers. But providers are pushing back. Not with protests, but with paperwork, data, and persistence. The system is broken, but it’s not unbeatable. The real winners aren’t the insurers who save the most money. They’re the ones who save lives without sacrificing care. The FDA is reviewing how generics are tested for complex drugs, with new guidance expected in late 2025. That could mean tighter standards for drugs like thyroid meds or blood thinners. Until then, providers are the last line of defense. Patients don’t care about corporate cost targets. They care about whether their medication works. And if it doesn’t? They’ll come back to you-not the insurer.Are generic drugs always safe to substitute for brand-name drugs?
For most medications, yes. The FDA requires generics to be bioequivalent to brand-name drugs within an 80-125% range. But for drugs with a narrow therapeutic index-like levothyroxine, warfarin, or certain epilepsy medications-even small differences can cause side effects or treatment failure. Physicians report adverse outcomes in 28% of cases after switching thyroid meds to generics. Always consider the patient’s history before allowing a substitution.
Why do insurers require step therapy before approving brand-name drugs?
Step therapy forces patients to try cheaper generic drugs first, with the goal of reducing costs. If the patient doesn’t respond-or has side effects-they can then appeal for the brand-name version. But this delays care and can lead to worsening conditions. In some cases, patients experience emergency visits or hospitalizations while waiting for approval.
How long does prior authorization typically take?
Response times vary. For urgent cases, federal rules now require Medicare Advantage plans to respond within 72 hours. For non-urgent requests, it can take up to 5 business days. In states without strong regulations, delays of 10-14 days are common. Electronic prior authorization (ePA) systems have reduced this to under 48 hours in many cases.
Can a provider be denied coverage even with clinical documentation?
Yes. Insurers sometimes deny requests even with solid documentation if they claim the criteria weren’t met-often because their definition of “medical necessity” is vague or inconsistent. In Arizona, new law (HB 2175) now requires a medical director to personally review denials, not just rely on AI or external reviewers. This is becoming a model for other states.
What’s the best way to increase approval rates for prior authorization requests?
Include objective clinical evidence: lab results showing therapeutic failure, documented adverse reactions to the generic, or previous hospitalizations linked to substitution. Providers who submit this type of data see approval rates 37% higher. Also, use electronic systems and build relationships with insurer case managers. Template letters help, but data wins.

mike tallent - 16 November 2025
Just had a patient switch from brand levothyroxine to generic and ended up in the ER with atrial fibrillation. Lab values were all over the place. I told her to stop the generic immediately and go back to the brand-insurance denied it again. Now I write ‘DO NOT SUBSTITUTE’ in red pen and attach her last three TSH results. It’s not ideal, but it’s the only way to keep people alive. 🩺💔
Julie Roe - 18 November 2025
I’ve been a nurse for 22 years and I’ve seen this play out a hundred times. Patients don’t understand why their meds ‘stop working’ after a switch. They think it’s them-‘Am I not taking it right?’ ‘Did I do something wrong?’ The truth is, the system is broken. Providers are doing their best with one hand tied behind their back and the other holding a fax machine. I wish more people knew how much time we spend fighting insurers instead of treating patients. It’s heartbreaking. And honestly? We’re not even getting thanked for it.
Sylvia Clarke - 18 November 2025
Let’s be real-insurers aren’t evil. They’re just following the logic of a broken system where profit is the only metric that matters. But here’s the irony: the same companies that push generics are the ones charging patients $700 for a single insulin vial. It’s not about cost-it’s about control. And the real tragedy? The people who suffer most are the ones who can’t afford to fight back. I’ve seen elderly patients skip doses because they can’t pay the $75 copay. That’s not healthcare. That’s financial predation dressed up as ‘efficiency.’
Joyce Genon - 19 November 2025
Look, I get that generics save money, but let’s not pretend this is some noble cost-cutting initiative. The real savings go to PBMs and shareholders-not patients. And the 98.7% ‘success rate’? That’s a lie wrapped in a statistic. Who counts the patient who got depressed after switching antidepressants and never told their doctor? Or the one who had a seizure because their generic epilepsy med had a 5% different absorption rate? Those aren’t ‘adverse outcomes’-they’re just invisible collateral damage. And now we’re supposed to be grateful for ePA systems that still take 48 hours? Please. We’re not fixing the system-we’re just making the paperwork prettier.
Jennifer Howard - 21 November 2025
It is imperative to note, with the utmost gravity, that the FDA's bioequivalence parameters for generic pharmaceuticals are not only statistically lax, but ethically indefensible. An 80-125% variance in serum concentration is not 'equivalent'-it is, in fact, a pharmacological gamble. Furthermore, the utilization of electronic prior authorization systems, while ostensibly streamlining, introduces a dangerous layer of algorithmic opacity. One must ask: who audits the auditors? And why, pray tell, are we permitting corporate entities to dictate clinical decisions? This is not medicine. It is corporate feudalism, masquerading as public policy. I shall be writing my congressperson immediately.
Gary Lam - 21 November 2025
Man, I’m from Hawaii and we’ve got a whole different vibe here-people don’t fight insurance, they just… wait. And pray. My cousin’s dad had to wait 11 days for a brand-name blood thinner because the insurer said ‘needs more documentation.’ He had a stroke on day 9. Now he can’t talk. The pharmacy tech just shrugged and said, ‘That’s just how it is.’ I don’t know if I’m mad or just… tired. 😔
Abdul Mubeen - 21 November 2025
Is it just me, or is this entire system a controlled demolition? Who benefits from the chaos? PBMs? Pharma? The same companies that own the brand drugs and the generics? And why are we not talking about the fact that the FDA’s testing protocols for generics were designed in the 1980s? This isn’t regulation-it’s a loophole with a badge. I’ve seen the internal emails. They don’t even pretend to care about patients. They just want the cheapest pill that doesn’t immediately kill someone. And we call this progress?
jalyssa chea - 22 November 2025
ugh i swear doctors are just lazy they could just use the generic and if the patient complains then switch back why make it so hard i mean its not like people die from it all the time right also why do you need 16 pages of paperwork for a thyroid med its just a pill
John Wayne - 23 November 2025
Interesting. But let’s not confuse anecdotal evidence with clinical reality. The overwhelming majority of patients transition seamlessly. The outliers are precisely that-outliers. The real issue is not the system, but the emotionalization of pharmaceuticals. Patients treat medication like a talisman. It’s not about chemistry-it’s about psychological dependency. If we removed the stigma around substitution, this entire debate would collapse under its own weight.